Abstract
Objective
When an infant’s prognosis is uncertain, communication between neonatologists and parents surrounding goals of care and decision-making can be challenging. This qualitative study explored communication between neonatologists and parents to discover qualities which may enhance or impede parent–clinician partnership under such difficult circumstances.
Study design
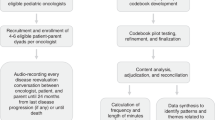
Guided by the National Cancer Institute (NCI) Patient Centered Communication framework, semi-structured individual interviews were conducted and analyzed regarding neonatologist and parent perceptions of their communication. Subjects consisted of nine dyads of neonatologists and English-speaking parents whose infant had an uncertain prognosis.
Results
Parents were overall satisfied with neonatologists’ communications concerning their infant’s uncertain trajectory. Nonetheless, both experienced challenges and distress during communication, impeding collaboration and engagement.
Conclusions
Families and neonatologists value principles of patient centered communication but report challenges implementing this practice. Incorporating a multidisciplinary approach in settings of prognostic uncertainty to foster patient centered communication, may enhance communication surrounding NICU care.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Wilfond BS. Tracheostomies and assisted ventilation in children with profound disabilities: navigating family and professional values. Pediatrics. 2014;133:S44–S49.
Snaman, JM, Feraco AM, Wolfe J, Baker JN. “What if?” Addressing uncertainty with families. Pediatric Blood Cancer. 2019;66:e27699.
Heller KS, Solomon MZ. Initiative for Pediatric Palliative Care (IPPC) Investigator Team. Continuity of care and caring: what matters to parents of children with life-threatening conditions. J Pediatr Nurs. 2005;20:335–46.
Shaw C, Stokoe E, Gallagher K, Aladangady N, Marlow N. Parental involvement in neonatal critical care decision-making. Sociol Health Illn. 2016;38:1217–12422.
Bell EF. American academy of pediatrics committee on fetus and newborn: noninitiation or withdrawal of intensive care for high-risk newborns. Pediatrics. 2007;119:401–3.
Racine E, Bell E, Farlow B, Miller S, Payot A, Rasmussen LA, et al. The ‘ouR-HOPE’ approach for ethics and communication about neonatal neurological injury. Developmental Med Child Neurol. 2016;59:125–35.
Stokes TA, Kukora SF, Boss RD. Caring for families at the limits of viability: the education of Dr. Green. Clin Perinatol. 2017;44:447–59.
Graham RJ, Robinson WM. Integrating palliative care into chronic care for children with severe neurodevelopmental disabilities. J Developmental Behav Pediatrics. 2005;26:361–5.
Kirschen MP, Walter JK. Ethical issues in neuroprognostication after severe pediatric brain injury. Semin Pediatr Neurol. 2015;22:187–95.
Politi MC, Clark MA, Ombao H, Legare F. The impact of physicians’ reactions to uncertainty on patients’ decision satisfaction. J Evaluation Clin Pract. 2011;17:675–8.
Haward MF, Gaucher N, Payot A, Robson K, Janvier A. Personalized decision making: practical recommendations for antenatal counseling for fragile neonates. Clin Perinatol. 2017;44:429–45.
Mishel MH. Uncertainty in illness. Image J Nurs Scholarsh. 1988;20:225–32.
Eidelman AI. Dilemmas in the treatment of premature infants at the borderline of viability. Rambam Maimonides Med J. 2011;2:e0066 https://doi.org/10.5041/RMMJ.10066
Ghosh AK. On the challenges of using evidence-based information: the role of clinical uncertainty. J Lab Clin Med. 2004;144:60–64.
Han PK, Klein WM, Arora NK. Varieties of uncertainty in health care: a conceptual taxonomy. Med Decis Mak. 2011;31:828–38.
Pepper D, Rempel G, Austin W, Ceci C, Hendson L. More than information: a qualitative study of parents’ perspectives on neonatal intensive care at the extremes of prematurity. Adv Neonatal Care. 2012;12:303–9.
Quill TE, Suchman AL. Uncertainty and control: learning to live with medicine’s limitations. Hum Med. 1993;9:109–20.
Evans LR, Boyd EA, Malvar G, Apatira L, Luce JM, Lo B, et al. Surrogate decision-makers’ perspectives on discussing prognosis in the face of uncertainty. Am J Respir Crit Care Med. 2009;179:48–53.
Luther VP, Crandall SJ. Commentary: ambiguity and uncertainty: neglected elements of medical education curricula? Academic Med. 2011;86:799–800.
Seely AJ. Embracing the certainty of uncertainty: implications for health care and research. Perspect Biol Med. 2013;56:65–77.
Solomon MZ, Seller DE, Heller KS, Dokken DL, Levetown M, Rushton C, et al. New and lingering controversies in pediatric end-of-life care. Pediatrics. 2005;116:871–83.
Tanis M, Beukeboom CJ. Organizational identification and the communication of identity: Effects of message characteristics on cognitive and affective identification. Br J Soc Psychol. 2011;50:784–91.
Meyer EC, Ritholz MD, Burns JP, Truog RD. Improving the quality of end-of-life care in the pediatric intensive care unit: parents’ priorities and recommendations. Pediatrics. 2006;117:649–57.
Russell G, Sawyer A, Rabe H, Abbott J, Gyte G, Duley L, et al. Parents’ views on care of their very premature babies in neonatal intensive care units: a qualitative study. BMC Pediatr. 2014;14:230–9.
Kavanaugh K, Savage T, Kilpatrick S, Kimura R, Hershberger P. Life support decisions for extremely premature infants: report of a pilot study. J Pediatr Nurs. 2005;20:347–59.
Miquel-Verges F, Woods SL, Aucott SW, Boss RD, Sulpar LJ, Donohue PK. Prenatal consultation with a neonatologist for congenital anomalies: parental perceptions. Pediatrics. 2009;124:e573–579.
Feudtner C. Partnering leadership. Arch Pediatr Adolesc Med. 2011;165:487–8.
Kasper J, Légaré F, Scheibler F, Geiger F. Turning signals into meaning—‘Shared decision making’ meets communication theory. Health Expect. 2012;15:3–11.
Klick JC, Ballantine A. Providing care in chronic disease: the ever-changing balance of integrating palliative and restorative medicine. Pediatr Clin North Am. 2007;54:799–812.
Levetown M. Communicating with children and families: from everyday interactions to skill in conveying distressing information. Pediatrics. 2008;121:e1441–1460. https://doi.org/10.1542/peds.2008-0565
Henry MS. Uncertainty, responsibility, and the evolution of the physician/patient relationship. J Med Ethics. 2006;32:321–3.
Wellbery C. The value of medical uncertainty? Lancet. 2010;375:1686–7.
Gaucher N, Payot A. From powerlessness to empowerment: Mothers expect more than information from the prenatal consultation for preterm labour. Paediatr Child Health. 2011;16:638–42.
Orzalesi M, Aite L. Communication with parents in neonatal intensive care. J Matern-Fetal Neonatal Med. 2011;24:135–7.
Shapiro J, Astin J, Shapiro SL, Robitshek D, Shapiro DH. Coping with loss of control in the practice of medicine. Families Syst Health. 2011;29:15–28.
Boss RD, Donohue PK, Larson SM, Arnold RM, Roter DL. Family conferences in the neonatal intensive care unit: observation of communication dynamics and contributions. Pediatr Crit Care Med. 2016;17:223–30.
French KB. Care of extremely small premature infants in the neonatal intensive care unit: a parent’s perspective. Clin Perinatol. 2017;44:275–82.
Harrison H. Principles of family centered care in NICU. Pediatrics 1993;92:643–50.
Institute of Medicine (US) Committee on Quality of Health Care in America. Crossing the quality chasm: a new health system for the 21st century. Washington DC: National Academies Press; 2001.
Latour JM, Hazelzet JA, Duivenvoorden HJ, van Goudoever JB. Perceptions of parents, nurses, and physicians on neonatal intensive care practices. J Pediatr. 2010;157:215–20.
Gooding JS, Cooper LG, Blaine AI, Franck LS, Howse JL, Derns SD. Family support and family-centered care in the neonatal intensive care unit: origins, advances, impact. Semin Perinatol. 2011;35:20–28.
Finlayson K, Dixon A, Smith C, Dykes F, Flacking R. Mothers’ perceptions of family centered care in neonatal intensive care units. Sex Reprod Healthc. 2014;5:119–24.
Epstein R, Street RL. Patient-centered communication in cancer care: promoting healing and reducing suffering. Bethesda, MD: National Cancer Institute, US Department of Health and Human Services, National Institutes of Health; 2007. Aug 24
Haward MF, Janvier A. An introduction to behavioural decision‐making theories for paediatricians. Acta Paediatr. 2015;104:340–5.
Cameron RA, Mazer BL, DeLuca JM, Mohile SG, Epstein RM. In search of compassion: a new taxonomy of compassionate physician behaviours. Health Expect. 2015;18:1672–85.
Davies B, Steele R, Krueger G, Albersheim S, Baird J, Bifirie M, et al. Best Practice in Provider/Parent Interaction. Qual Health Res. 2017;27:406–20.
Lantos JohnD. Ethical problems in decision making in the neonatal ICU. N Engl J Med. 2018;379:1851–60.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Drach, L.L., Hansen, D.A., King, T.M. et al. Communication between neonatologists and parents when prognosis is uncertain. J Perinatol 40, 1412–1422 (2020). https://doi.org/10.1038/s41372-020-0673-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-0673-6
This article is cited by
-
Uncertainty and probability in neonatal end-of-life decision-making: analysing real-time conversations between healthcare professionals and families of critically ill newborns
BMC Palliative Care (2023)
-
Words matter: exploring communication between parents and neonatologists
Journal of Perinatology (2022)