Abstract
Objective
Determine impact of using delivery criteria to initiate antibiotics among very low birth weight (VLBW) and extremely low birth weight (ELBW) infants.
Study design
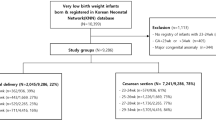
Single site cohort study from 01/01/2009 to 01/31/2020. After 04/2017, infants delivered by Cesarean section, without labor or membrane rupture were categorized as low-risk for early-onset infection and managed without empiric antibiotics. We determined effect of this guideline by pre-post, and interrupted time-series analyses.
Results
After 04/2017, antibiotic initiation ≤3 days decreased among low-risk VLBW (62% vs. 13%, p < 0.001) and low-risk ELBW (88% vs. 21%, p < 0.001) infants. In time series analysis, guideline was associated with decreased initiation among low-risk ELBW infants. In contrast, low-risk VLBW infants demonstrated decreased antibiotic initiation throughout study period. Incidence of confirmed infection, death, or transfer ≤7 days age was unchanged.
Conclusion
Delivery criteria may be used to optimize early antibiotic initiation among preterm infants without short-term increase in adverse outcomes.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Fouhy F, Guinane CM, Hussey S, Wall R, Ryan CA, Dempsey EM, et al. High-throughput sequencing reveals the incomplete, short-term recovery of infant gut microbiota following parenteral antibiotic treatment with ampicillin and gentamicin. Antimicrob Agents Chemother. 2012;56:5811–20.
Le J, Nguyen T, Okamoto M, McKamy S, Lieberman JM. Impact of empiric antibiotic use on development of infections caused by extended-spectrum beta-lactamase bacteria in a neonatal intensive care unit. Pediatr Infect Dis J. 2008;27:314–8.
Ting JY, Roberts A, Sherlock R, Ojah C, Cieslak Z, Dunn M, et al. Duration of initial empirical antibiotic therapy and outcomes in very low birth weight infants. Pediatrics. 2019;143. https://doi.org/10.1542/peds.2018-2286.
Kuppala VS, Meinzen-Derr J, Morrow AL, Schibler KR. Prolonged initial empirical antibiotic treatment is associated with adverse outcomes in premature infants. J Pediatr. 2011;159:720–5.
Ting JY, Synnes A, Roberts A, Deshpandey AC, Dow K, Yang J, et al. Association of antibiotic utilization and neurodevelopmental outcomes among extremely low gestational age neonates without proven sepsis or necrotizing enterocolitis. Am J Perinatol. 2018;35:972–8.
Flannery DD, Ross RK, Mukhopadhyay S, Tribble AC, Puopolo KM, Gerber JS. Temporal trends and center variation in early antibiotic use among premature infants. JAMA Netw Open. 2018;1:e180164–e180164.
Puopolo KM, Mukhopadhyay S, Hansen NI, Cotten CM, Stoll BJ, Sanchez PJ, et al. Identification of extremely premature infants at low risk for early-onset sepsis. Pediatrics. 2017;140. https://doi.org/10.1542/peds.2017-0925. Epub 2017 Oct.
Greenberg RG, Chowdhury D, Hansen NI, Smith PB, Stoll BJ, Sanchez PJ, et al. Prolonged duration of early antibiotic therapy in extremely premature infants. Pediatr Res. 2019;85:994–1000.
Benirschke K. Routes and types of infection in the fetus and the newborn. AMA J Dis Child. 1960;99:714–21.
Mukhopadhyay S, Puopolo KM. Clinical and Microbiologic Characteristics of Early-onset Sepsis Among Very Low Birth Weight Infants: Opportunities for Antibiotic Stewardship. Pediatr Infect Dis J. 2017;36:477–81.
Puopolo KM, Benitz WE, Zaoutis TE. Committee on Fetus and Newborn, Committee on Infectious Diseases. Management of neonates born at less than or equal to 34 6/7 weeks’ gestation with suspected or proven early-onset bacterial sepsis. Pediatrics. 2018;142. https://doi.org/10.1542/peds.2018-2896.
Stoll BJ, Hansen NI, Sanchez PJ, Faix RG, Poindexter BB, Van Meurs KP, et al. Early onset neonatal sepsis: the burden of group B Streptococcal and E. coli disease continues. Pediatrics. 2011;127:817–26.
Mukhopadhyay S, Sengupta S, Puopolo KM. Challenges and opportunities for antibiotic stewardship among preterm infants. Arch Dis Child Fetal Neonatal Ed. 2019;104:F327–32.
Bell MJ. Neonatal necrotizing enterocolitis. N Engl J Med. 1978;298:281–2.
Caswell JM. Interrupted time series analysis for single series and comparative designs: a guide for beginners with SAS macro. 2019. https://www.academia.edu/35275583/Interrupted_Time_Series_Analysis_for_Single_Series_and_Comparative_Designs_A_Guide_for_Beginners_with_SAS_Macro?sm=b.
Ting JY, Synnes A, Roberts A, Deshpandey A, Dow K, Yoon EW, et al. Association between antibiotic use and neonatal mortality and morbidities in very low-birth-weight infants without culture-proven sepsis or necrotizing enterocolitis. JAMA Pediatr. 2016;170:1181–7.
Newman TB, Puopolo KM, Wi S, Draper D, Escobar GJ. Interpreting complete blood counts soon after birth in newborns at risk for sepsis. Pediatrics. 2010;126:903–9.
Christensen RD, Yoder BA, Baer VL, Snow GL, Butler A. Early-onset neutropenia in small-for-gestational-age infants. Pediatrics. 2015;136:e1259–67.
Doron MW, Makhlouf RA, Katz VL, Lawson EE, Stiles AD. Increased incidence of sepsis at birth in neutropenic infants of mothers with preeclampsia. J Pediatr. 1994;125:452–8.
Teng RJ, Wu TJ, Garrison RD, Sharma R, Hudak ML. Early neutropenia is not associated with an increased rate of nosocomial infection in very low-birth-weight infants. J Perinatol. 2009;29:219–24.
Deshmukh HS, Liu Y, Menkiti OR, Mei J, Dai N, O’Leary CE, et al. The microbiota regulates neutrophil homeostasis and host resistance to Escherichia coli K1 sepsis in neonatal mice. Nat Med. 2014;20:524–30.
Acknowledgements
SM was supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH) grant (K23HD088753) and DDF by NICHD/NIH grant (T32HD060550).
Author information
Authors and Affiliations
Contributions
SJG contributed to study design and analytic plan, data collection, reviewed and revised the manuscript. MBD contributed to data collection and management, data analysis and interpretation, reviewed and revised the manuscript. DDF contributed to study design and analytic plan, data collection, reviewed and revised the manuscript. MRP contributed to data analysis and interpretation, reviewed and revised the manuscript. KMP contributed to study design and analytic plan, reviewed and revised the manuscript. SM conceptualized and designed the study, contributed to data collection and analysis, and drafted the first manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Garber, S.J., Dhudasia, M.B., Flannery, D.D. et al. Delivery-based criteria for empiric antibiotic administration among preterm infants. J Perinatol 41, 255–262 (2021). https://doi.org/10.1038/s41372-020-00784-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-020-00784-y
This article is cited by
-
Association of delivery risk phenotype with early-onset sepsis in preterm infants
Journal of Perinatology (2023)
-
Trends in prostate cancer mortality in the United States of America, by state and race, from 1999 to 2019: estimates from the centers for disease control WONDER database
Prostate Cancer and Prostatic Diseases (2023)
-
Early antibiotic exposure in very-low birth weight infants and infection risk at 3–7 days after birth
Journal of Perinatology (2023)
-
Noninfectious influencers of early-onset sepsis biomarkers
Pediatric Research (2022)
-
Utility of blood cultures in preterm infants born by cesarean delivery due to non-infectious maternal or fetal indications
Journal of Perinatology (2022)