Abstract
Objective
To test our hypothesis that an innovative method of early palliative care called “Baby, Attachment, Comfort Interventions” reduces psychological distress in parents of neonates with congenital heart disease.
Study design
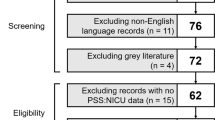
Prospective cohort study of parents of neonates with congenital heart disease. Distress was evaluated at admission and discharge using Neonatal Unit Parental Stressor Scale and Depression Anxiety Stress Index-21. Control parents received standard of care. Intervention parents received interdisciplinary interventions aimed at improving neonatal comfort and parenting experience.
Results
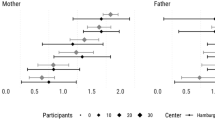
Seventy-seven parents participated. Stress decreased in the intervention group (26 parents) but not in the control group (51 parents). There was no decrease in anxiety or depression in either group.
Conclusion
Early palliative care reduces stress in parents of neonates with congenital heart disease. Further work is needed to address depression/anxiety in this group of high-risk parents.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Woolf‐King SE, Anger A, Arnold EA, Weiss SJ, Teitel D. Mental health among parents of children with critical congenital heart defects: a systematic review. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2017; 2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5523775/. Accessed 5 Nov 2018.
Woolf‐King SE, Arnold E, Weiss S, Teitel D. “There’s no acknowledgement of what this does to people”: a qualitative exploration of mental health among parents of children with critical congenital heart defects. J Clin Nurs. 2018;27:2785–94.
Doherty N, McCusker CG, Molloy B, Mulholland C, Rooney N, Craig B, et al. Predictors of psychological functioning in mothers and fathers of infants born with severe congenital heart disease. J Reprod Infant Psychol. 2009;27:390–400.
Diffin J, Spence K, Naranian T, Badawi N, Johnston L. Stress and distress in parents of neonates admitted to the neonatal intensive care unit for cardiac surgery. Early Hum Dev. 2016;103:101–7.
Sood E, Karpyn A, Demianczyk AC, Ryan J, Delaplane EA, Neely T, et al. Mothers and fathers experience stress of congenital heart disease differently: recommendations for pediatric critical care. Pedia Crit Care Med. 2018;19:626–34.
Lawoko S, Soares JJF. Psychosocial morbidity among parents of children with congenital heart disease: a prospective longitudinal study. Heart Lung. 2006;35:301–14.
Franck LS, McQuillan A, Wray J, Grocott MPW, Goldman A. Parent stress levels during children’s hospital recovery after congenital heart surgery. Pedia Cardiol. 2010;31:961–8.
Solberg Ø, Dale MTG, Holmstrøm H, Eskedal LT, Landolt MA, Vollrath ME. Long-term symptoms of depression and anxiety in mothers of infants with congenital heart defects. J Pedia Psychol. 2011;36:179–87.
Miles MS, Funk SG, Kasper MA. The neonatal intensive care unit environment: sources of stress for parents. AACN Clin Issues Crit Care Nurs. 1991;2:346–54.
Cleveland LM. Parenting in the neonatal intensive care unit. J Obstet Gynecol Neonatal Nurs. 2008;37:666–91.
Bertaud S, Lloyd DFA, Laddie J, Razavi R. The importance of early involvement of paediatric palliative care for patients with severe congenital heart disease. Arch Dis Child. 2016;101:984–7.
Rychik J, Donaghue DD, Levy S, Fajardo C, Combs J, Zhang X, et al. Maternal psychological stress after prenatal diagnosis of congenital heart disease. J Pediatr. 2013;162:302–307. e1
Helfricht S, Latal B, Fischer JE, Tomaske M, Landolt MA. Surgery-related posttraumatic stress disorder in parents of children undergoing cardiopulmonary bypass surgery: a prospective cohort study. Pedia Crit Care Med. 2008;9:217–23.
Uzark K, Jones K. Parenting stress and children with heart disease. J Pedia Health Care. 2003;17:163–8.
Melnyk BM, Feinstein NF, Alpert-Gillis L, Fairbanks E, Crean HF, Sinkin RA, et al. Reducing premature infants’ length of stay and improving parents’ mental health outcomes with the Creating Opportunities for Parent Empowerment (COPE) neonatal intensive care unit program: a randomized, controlled trial. Pediatrics. 2006;118:e1414–1427.
Browne JV, Talmi A. Family-based intervention to enhance infant-parent relationships in the neonatal intensive care unit. J Pedia Psychol. 2005;30:667–77.
Ravn IH, Smith L, Smeby NA, Kynoe NM, Sandvik L, Bunch EH, et al. Effects of early mother-infant intervention on outcomes in mothers and moderately and late preterm infants at age 1 year: a randomized controlled trial. Infant Behav Dev. 2012;35:36–47.
Kaaresen PI, Rønning JA, Ulvund SE, Dahl LB. A randomized, controlled trial of the effectiveness of an early-intervention program in reducing parenting stress after preterm birth. Pediatrics. 2006;118:e9–19.
Chertok IRA, McCrone S, Parker D, Leslie N. Review of interventions to reduce stress among mothers of infants in the NICU. Adv Neonatal Care. 2014;14:30–7.
Lisanti AJ, Vittner D, Medoff-Cooper B, Fogel J, Wernovsky G, Butler S. Individualized family-centered developmental care: an essential model to address the unique needs of infants with congenital heart disease. J Cardiovasc Nurs. 2018;34:85–93.
Kang TI, Munson D, Hwang J, Feudtner C. Integration of palliative care into the care of children with serious illness. Pedia Rev. 2014;35:318–26.
Carter BS. Pediatric palliative care in infants and neonates. Children. 2018;5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5835990/. Accessed 5 Apr 2019.
Parravicini E. Neonatal palliative care. Curr Opin Pediatr. 2017;29:135–40.
Mazwi ML, Henner N, Kirsch R. The role of palliative care in critical congenital heart disease. Semin Perinatol. 2017;41:128–32.
Ferrell BR, Twaddle ML, Melnick A, Meier DE. National consensus project clinical practice guidelines for quality palliative care guidelines, 4th ed. J Palliat Med. 2018. [Epub ahead of print].
Hancock H, Pituch K, Uzark K, Bhat P, Fifer C, Silveira M, et al. A randomised trial of early palliative care for maternal stress in infants prenatally diagnosed with single-ventricle heart disease. Cardiol Young. 2018;28:561–70. https://digitalcommons.wustl.edu/open_access_pubs/6728.
Parravicini E, Lorenz JM. Neonatal outcomes of fetuses diagnosed with life-limiting conditions when individualized comfort measures are proposed. J Perinatol. 2014;34:483–7.
Neonatal Comfort Care Program. http://www.neonatalcomfortcare.com/. (2019).
Jenkins KJ. Risk adjustment for congenital heart surgery: the RACHS-1 method. Semin Thorac Cardiovasc Surg Pedia Card Surg Annu. 2004;7:180–4.
Medicine COFAN and SOAAP. Prevention and management of procedural pain in the neonate: an update. Pediatrics. 2016;137:e20154271.
Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav Res Ther. 1995;33:335–43.
Reid T, Bramwell R, Booth N, Weindling AM. A new stressor scale for parents experiencing neonatal intensive care: the NUPS (Neonatal Unit Parental Stress) scale. J Reprod Infant Psychol. 2007;25:66–82.
Sinclair SJ, Siefert CJ, Slavin-Mulford JM, Stein MB, Renna M, Blais MA. Psychometric evaluation and normative data for the depression, anxiety, and stress scales-21 (DASS-21) in a nonclinical sample of U.S. adults. Eval Health Prof. 2012;35:259–79.
Henderson J. It’s like going home to emptiness.” Becoming a mother and providing mother’s milk to premature infants in the neonatal intensive care unit, a latina mother’s perspective. 2015.
Fischer AL, Butz C, Nicholson L, Blankenship A, Dyke P, Cua CL. Caregiver anxiety upon discharge for neonates with congenital heart disease. Congenit Heart Dis. 2012;7:41–5.
Parravicini E, Daho’ M, Foe G, Steinwurtzel R, Byrne M. Parental assessment of comfort in newborns affected by life-limiting conditions treated by a standardized neonatal comfort care program. J Perinatol. 2018;38:142–7.
CDC. Data and statistics on congenital heart defects. Centers for Disease Control and Prevention. 2019. https://www.cdc.gov/ncbddd/heartdefects/data.html.
Guzman GG. Household income: 2017. Suitland, MD: US Census Bureau; 2018.
Bureau UC. Educational Attainment in the United States. Bureau UC; 2018. https://www.census.gov/data/tables/2018/demo/education-attainment/cps-detailed-tables.html.
Acknowledgements
The authors thank the Neonatal Comfort Care Program team for their participation in and support of this study.
Author information
Authors and Affiliations
Contributions
KPC, EP, and RS designed the study, collected the data, and wrote the manuscript. LB and SS managed, entered, and analyzed the data.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Callahan, K., Steinwurtzel, R., Brumarie, L. et al. Early palliative care reduces stress in parents of neonates with congenital heart disease: validation of the “Baby, Attachment, Comfort Interventions”. J Perinatol 39, 1640–1647 (2019). https://doi.org/10.1038/s41372-019-0490-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-019-0490-y