Abstract
Objective
To determine whether maternal disclosure of HIV serostatus is associated with uptake of perinatal HIV transmission prevention interventions.
Study design
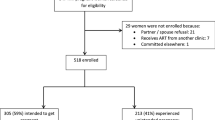
Retrospective cohort study of women living with HIV enrolled in a perinatal HIV clinic. Women who disclosed their HIV serostatus to sexual partner(s) prior to delivery were compared to non-disclosers. Multivariable logistic regression was performed.
Results
Of 209 women, 71.3% (N = 149) disclosed. Non-disclosers were more likely to attend <10 prenatal visits, demonstrated worse antiretroviral therapy adherence, required more time to achieve virologic suppression, and were less likely to have an undetectable viral load. On multivariable analyses, disclosure status did not remain associated with these factors. However, compared to non-disclosers, disclosers had lower odds of preterm delivery (OR: 0.43, 95% CI: 0.19–0.94) and greater odds of postpartum visit attendance (aOR: 5.10, 95% CI: 1.65–15.72).
Conclusions
Non-disclosure of HIV status to sexual partner(s) during pregnancy may be a risk factor for preterm birth and poorer postpartum visit attendance.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Whitmore S, Zhang X, Taylor A, Blair J. Estimated number of infants born to HIV-infected women in the United States and five dependent areas, 2006. J Acquir Immun Defic Syndr. 2011;57:218–22.
Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for use of antiretroviral drugs in pregnant HIV-1-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States 2016. http://aidsinfo.nih.gov/contentfiles/lvguidelines/PerinatalGL.pdf. Accessed 7 and 28 June 2016.
Sperling R, Shapiro D, Coombs R, Todd J, Herman S, McSherry G, et al. Maternal viral load, zidovudine treatment, and the risk of transmission of human immunodeficiency virus type 1 from mother to infant. Pediatric AIDS Clinical Trials Group Protocol 076 Study Group. New Engl J Med. 1996;335:1621–9.
Cooper E, Charurat M, Mofenson L, Hanson I, Pitt J, Diaz C, et al. Combination antiretroviral strategies for the treatment of pregnant HIV-2 infected women and prevention of perinatal HIV-1 transmission. J Acquir Immune Defic Syndr. 2002;29:484–94.
Townsend C, Cortina-Borja M, Peckham C, de Ruiter A, Lyall H, Tookey P. Low rates of mother-to-child transmission of HIV following effective pregnancy interventions in the United Kingdom and Ireland, 2000-2006. AIDS. 2008;22:973–81.
Kuhn L, Abrams E, Matheson P, Thomas P, Lambert G, Bamji M, et al. Timing of maternal-infant HIV transmission: associations between intrapartum factors and early polymerase chain reaction results. New York City Perinatal HIV Transmission Collaborative Study Group. AIDS. 1997;11:429–35.
Kuhn L, Steketee R, Weedon J, Abrams E, Lambert G, Bamji M, et al. Distinct risk factors for intrauterine and intrapartum human immunodeficiency virus transmission and consequences for disease progression in infected children. Perinatal AIDS Collaborative Transmission Study. J Infect Dis. 1999;179:52–8.
Warszawski J, Tubiana R, LeChenadec J, Blanche S, Teglas J, Dollfus C, et al. Mother-to-child HIV transmission despite antiretroviral therapy in the ANRS French Perinatal Cohort. AIDS. 2008;22:289–99.
Magder L, Mofenson L, Paul M, Zorrilla C, Blattner W, Tuomala R, et al. RIsk factors for in utero and intrapartum transmission of HIV. J Acquir Immun Defic Syndr. 2005;38:87–95.
Jasseron C, Mandelbrot L, Dollfus C, Trocme N, Tubiana R, Teglas J, et al. Non-disclosure of a pregnant woman’s HIV status to her partner is associated with non-optimal prevention of mother-to-child transmission. AIDS Behav. 2013;17:488–97.
Carter M, Kraft J, Hatfield-Timajchy K, Snead M, Ozeryansky L, Fasula A, et al. The reproductive health behaviors of HIV-infected young women in the United States: a literature review. AIDS Patient Care STDS. 2013;27:669–80.
Nacius LA, Levison J, Minard CG, Fasser C, Davila JA. Serodiscordance and disclosure among HIV-positive pregnant women in the Southwestern United States. AIDS Patient Care STDS. 2013;27:242–7.
Adams J, Brady K, Michael Y, Yehia B, Momplaisir F. Postpartum engagement in HIV care: an important predictor of long-term retention in care and viral suppression. Clin Infect Dis. 2015;61:1880–7.
Aebi-Popp K, Kouyos R, Bertisch B, Staehelin C, Rudin C, Hoesli I, et al. Postnatal retention in HIV care: insight from the Swiss HIV Cohort Study over a 15-year observational period. HIV Med. 2016;17:280–88.
Swain C-A, Smith L, Nash D, Pulver W, Gordon D, Bian F, et al. Postpartum Human Immunodeficiency Virus care among women diagnosed during pregnancy. Obstet Gynecol. 2016;128:44–51.
Mandelbrot L, Tubiana R, LeChenadec J, Dollfus C, Faye A, Pannier E, et al. No perinatal HIV-1 transmission from women with effective antiretroviral therapy starting before conception. Clin Infect Dis. 2015;61:1715–25.
Onono M, Cohen C, Jerop M, Bukusi E, Turan J. HIV serostatus and disclosure: implications for infant feeding practice in rural south Nyanza, Kenya. BMC Public Health. 2014;14:1–9.
Medley A, Garcia-Moreno C, McGill S, Maman S. Rates, barriers and outcomes of HIV serostatus disclosure among women in developing countries: implications for prevention of mother-to-child transmission programmes. Bull World Health Organ. 2004;82:299–307.
Sendo E, Cherie A, Ekrku T. DIsclosure experience to partner and its effect on intention to utilize prevention of mother to child transmission service among HIV positive pregnant women attending antenatal care in Addis Ababa, Ethiopia. BMC Public Health. 2013;13:1–7.
Spangler S, Onono M, Bukusi E, Cohen C, Turan J. HIV-positive status disclosure and use of essential PMTCT and maternal health services in rural Kenya. J Acquir Immun Defic Syndr. 2014;67:S235–42.
Borders A, Grobman W, Amsden L, Holl J. Chronic stress and low birth weight neonates in a low-income population of women. Obstet Gynecol. 2007;109:331–8.
Chen M, Grobman W, Gollan J, Borders A. The use of psychosocial stress scales in preterm birth research. Am J Obstet Gynecol. 2011;205:402–34.
Bofill L, Waldrop-Valverde D, Metsch L, Pereyra M, Kolber MA. Demographic and psychosocial factors associated with appointment attendance among HIV-positive outpatients. AIDS Care. 2011;23:1219–25.
Kalichman SC, DiMarco M, Austin J, Luke W, DiFonzo K. Stress, social support, and HIV-status disclosure to family and friends among HIV-positive men and women. J Behav Med. 2003;26:315–32.
Turan JM, Nyblade L. HIV-related stigma as a barrier to achievement of global PMTCT and maternal health goals: a review of the evidence. AIDS Behav. 2013;17:2528–39.
Vyavaharkar M, Moneyham L, Corwin S, Tavakoli A, Saunders R, Annang L. HIV-disclosure, social support, and depression among HIV-infected African American women living in the rural southeastern United States. AIDS Educ Prev. 2011;23:78–90.
Miller ES, Yee LM, Dorman RM, McGregor DV, Sutton SH, Garcia PM, Wisner KL. Is maternal disclosure of HIV serostatus associated with a reduced risk of postpartum depression? Am J Obstet Gynecol. 2016; 215:521.e1-5.
Brittain K, Mellins C, Phillips T, Zerbe A, Abrams E, Myer L, et al. Social support, stigma and antenatal depression among HIV-infected pregnant women in South Africa. AIDS Behav. 2017; 21:274-82.
Turan B, Stringer K, Onono M, Bukusi E, Weiser S, Cohen C, et al. Linkage to HIV care, postpartum depression, and HIV-related stigma in newly diagnosed pregnant women living with HIV in Kenya: a longitudinal observational study. BMC Pregnancy Childbirth. 2014;14:1–10.
Hatcher A, Woollett N, Pallitto C, Mokoatle K, Stockl H, MacPhail C, et al. Bidirectional links between HIV and intimate partner violence in pregnancy: implications for prevention of mother-to-child transmission. J Int AIDS Soc. 2014;17:19233.
Shamu S, Zarowsky C, Shefer T, Temmerman M, Abrahams N. Intimate partner violence after disclosure of HIV test results among pregnant women in Harare, Zimbabwe. PLoS ONE. 2014;9:e109447.
Maman S, Groves A, McNaughton Reyes H, Moodley D. Diagnosis and disclosure of HIV status: Implications for women’s risk of physical partner violence in the postpartum period. J Acquir Immun Defic Syndr. 2016;72:546–51.
Funding
LMY and ESM were supported by the NICHD K12 HD050121-11 and K12 HD050121-09, respectively.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Yee, L.M., McGregor, D.V., Sutton, S.H. et al. Association between maternal HIV disclosure and risk factors for perinatal transmission. J Perinatol 38, 639–644 (2018). https://doi.org/10.1038/s41372-018-0066-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-018-0066-2