Abstract
Background
Exposure to polycyclic aromatic hydrocarbons (PAHs) is a potential risk factor for asthma prevalence. This study aims to explore whether PAHs exposure is associated with childhood asthma by altering microbial diversity and metabolic profiles.
Methods
Thirty children with asthma and 30 children as control in Nanjing, China were recruited. Urinary 1-hydroxypyrene (1-OHPyr) level was determined by UPLC–Orbitrap–MS as a PAHs exposure biomarker. Logistic regression was conducted to investigate the association between 1-OHPyr and childhood asthma. Microbial diversity was analyzed by 16S rRNA gene sequencing. Metabolic profiles were obtained by UPLC–Orbitrap–MS methods. Differential microbiota and metabolites were screened and selected as response biomarkers or intermediates. Mediation analysis was conducted to assess the association between PAHs and asthma mediated by intermediates.
Results
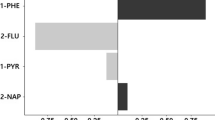
Participating children with and without asthma aged 6.43 ± 2.23 years. The urinary 1-OHPyr level ranged from 0.10 to 1.51 μmol/mol (creatinine corrected) in the participants. The urinary 1-OHPyr level was associated with childhood asthma (OR = 7.21, 95% CI: 1.03–50.42 per 1 μmol/mol unit). Microbial diversity was decreased in the group with asthma and there was a significant shift in the abundance of Proteobacteria (at the phylum level), Veillonella and Prevotella (at the genus level). The enrichment pathway analysis showed that differentially expressed metabolites were involved in purine metabolism, amino acid metabolism, and lipid and fatty acid metabolism. The urinary 1-OHPyr level was associated with the abundance of Actinomyces sp. oral clone IO076 and 7-methylguanine that showed a mediation effect on the association between urinary 1-OHPyr levels and childhood asthma by mediation analysis.
Conclusions
Urinary 1-OHPyr exposure was associated with childhood asthma, microbial diversity, and metabolic profiles. Microbial diversity and metabolic profiles may be intermediates as response biomarkers to PAHs exposure in childhood asthma. Further research is needed to confirm these study results and determine the underlying mechanism.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
National Cooperation Group on Childhood Asthma. [A nationwide survey in China on prevalence of asthma in 0-14 year-old children]. wu han shi yi xue ke yan. 1995;17:31–32. (in Chinese)
National Cooperation Group on Childhood Asthma. [A nationwide survey in China on prevalence of asthma in urban children]. Chin J Pediatr. 2003;41:123–7. (in Chinese)
National Cooperation Group on Childhood Asthma. [Third nationwide survey of childhood asthma in urban areas of China]. Chin J Pediatr. 2013;51:729–35. (in Chinese)
Mukherjee AB, Zhang ZJ. Allergic asthma: influence of genetic and environmental factors. J Biol Chem. 2011;286:32883–9.
Saulyte J, Regueira C, Montes-Martínez A, Khudyakov P, Takkouche B. Active or passive exposure to tobacco smoking and allergic rhinitis, allergic dermatitis, and food allergy in adults and children: a systematic review and meta-analysis. PLoS Med. 2014;11:e1001611.
Stein RT, Sherrill D, Morgan WJ, Holberg CJ, Halonen M, Taussig LM, et al. Respiratory syncytial virus in early life and risk of wheeze and allergy by age 13 years. Lancet. 1999;354:541–5.
Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014;383:1581–92.
Brunst KJ, Ryan PH, Brokamp C, Bernstein D, Reponen T, Lockey J, et al. Timing and duration of traffic-related air pollution exposure and the risk for childhood wheeze and asthma. Am J Respir Crit Care Med. 2015;192:421–7.
Miller RL, Garfinkel R, Lendor C, Hoepner L, Li Z, Romanoff L, et al. Polycyclicaromatic hydrocarbon metabolite levels and pediatric allergy and asthma in an inner-city cohort. Pediatr Allergy Immunol. 2010;21:260–7.
Gale S, Noth EM, Mann JK, Balmes JR, Hammond SK, Tager IB. Polycyclic aromatic hydrocarbon exposure and wheeze in a cohort of children with asthma in Fresno, CA. J Exposure Sci Environ Epidemiol. 2012;22:386–92.
Rogula-Kozłowska W, Kozielska B, Klejnowski K. Concentration, origin and health hazard from fine particle-bound PAH at three characteristic sites in Southern Poland. Bull Environ Contam Toxicol. 2013;91:349–55.
Al-Daghri NM, Alokail MS, Abd-Alrahman SH, Draz HM, Yakou SM, Clerici M. Polycyclic aromatic hydrocarbon exposure and pediatric asthma in children: a case-control study. Environ Health. 2013;12:1.
Karimi P, Peters KO, Bidad K, Strickland PT. Polycyclic aromatic hydrocarbons and childhood asthma. Eur J Epidemiol. 2015;30:91–101.
Baird WM, Hooven LA, Mahadevan B. Carcinogenic polycyclic aromatic hydrocarbon-DNA adducts and mechanism of action. Environ Mol Mutagenesis. 2015;45:106–14.
Korashy HM, El-Kadi AOS. The role of aryl hydrocarbon receptor in the pathogenesis of cardiovascular diseases. Drug Metab Rev. 2006;38:411–50.
Wormley DD, Ramesh A, Hood DB. Environmental contaminant–mixture effects on CNS development, plasticity, and behavior. Toxicol Appl Pharmacol. 2004;197:49–65.
Wang IJ, Karmaus WJ, Yang CC. Polycyclic aromatic hydrocarbons exposure, oxidative stress, and asthma in children. Int Arch Occup Environ Health. 2017;90:297–303.
Kanoh T, Suzuki T, Ishimori M, Ikeda S, Ohasawa M, Ohkuni H, et al. Adjuvant activities of pyrene, anthracene, fluoranthene and benzo(a)pyrene in production of anti-IgE antibody to Japanese cedar pollen allergen in mice. J Clin Lab Immunol. 1996;48:133–47.
Ewa B, Danuta MŠ. Polycyclic aromatic hydrocarbons and PAH-related DNA adducts. J Appl Genet. 2017;58:321–30.
Herbstman JB, Tang D, Zhu D, Qu L, Sjödin A, Li Z, et al. Prenatal exposure to polycyclic aromatic hydrocarbons, benzo[a]pyrene-DNA adducts, and genomic DNA methylation in cord blood. Environ Health Perspect. 2012;120:733–8.
Vineis P, van Veldhoven K, Chadeau-Hyam M, Athersuch TJ. Advancing the application of omics-based biomarkers in environmental epidemiology. Environ Mol Mutagen. 2013;54:461–7.
Wang BH, Yao MF, Lv LX, Ling ZX, Li LJ. The human microbiota in health and disease. Eng Prc. 2017;3:71–82.
Björkstén B, Sepp E, Julge K, Voor T, Mikelsaar M. Allergy development and the intestinal microflora during the first year of life. J Allergy Clin Immunol. 2001;108:516–20.
Dzidic M, Abrahamsson TR, Artacho A, Björkstén B, Collado MC, Mira A, et al. Aberrant IgA responses to the gut microbiota during infancy precede asthma and allergy development. J Allergy Clin Immunol. 2017;139:1017–25.
Defois C, Ratel J, Denis S, Batut B, Beugnot R, Peyretaillade E, et al. Environmental pollutant benzo[a]pyrene impacts the volatile metabolome and transcriptome of the human gut microbiota. Front Microbiol. 2017;8:1562.
Sowada J, Lemoine L, Schön K, Hutzler C, Luch A, Tralau T. Toxification of polycyclic aromatic hydrocarbons by commensal bacteria from human skin. Arch Toxicol. 2017;91:2331–41.
Roslund MI, Rantala S, Oikarinen S, Puhakka R, Hui N, Parajuli A, et al. Endocrine disruption and commensal bacteria alteration associated with gaseous and soil PAH contamination among daycare children. Environ Int. 2019;130:104894.
Peng B, Li H, Peng XX. Functional metabolomics: from biomarker discovery to metabolome reprogramming. Protein Cell. 2015;6:628–37.
Moorthy B, Chu C, Carlin DJ. Polycyclic aromatic hydrocarbons: from metabolism to lung cancer. Toxicol Sci. 2015;145:5–15.
Chen CS, Yuan TH, Shie RH, Wu KY, Chan CC. Linking sources to early effects by profiling urine metabolome of residents living near oil refineries and coal-fired power plants. Environ Int. 2017;102:87–96.
Zhang SY, Shao D, Liu H, Feng J, Feng B, Song X, et al. Metabolomics analysis reveals that benzo[a]pyrene, a component of PM2.5, promotes pulmonary injury by modifying lipid metabolism in a phospholipase A2-dependent manner in vivo and in vitro. Redox Biol. 2017;13:459–69.
Verma N, Pink M, Boland S, Rettenmeier AW, Schmitz-Spanke S. Benzo[a]pyrene-induced metabolic shift from glycolysis to pentose phosphate pathway in the human bladder cancer cell line RT4. Sci Rep. 2017;7:9773.
Cao S, Wang L, Zhang Z, Chen F, Wu Q, Li L. Sulforaphane-induced metabolomic responses with epigenetic changes in estrogen receptor positive breast cancer cells. FEBS Open Bio. 2018;8:2022–34.
Fourth National Report on Human Exposure to Environmental Chemicals, Updated Tables. CDC Centers for Disease Control and Prevention, USA. 2018: 592.
Reinke SN, Gallart-Ayala H, Gómez C, Checa A, Fauland A, Naz S, et al. Metabolomics analysis identifies different metabotypes of asthma severity. Eur Respir J. 2017;49:1601740.
Yu M, Cui FX, Jia HM, Zhou C, Yang Y, Zhang HW, et al. Aberrant purine metabolism in allergic asthma revealed by plasma metabolomics. J Pharm Biomed Anal. 2016;120:181–9.
Orhan H, Vermeulen NP, Tump C, Zappey H, Meerman JH. Simultaneous determination of tyrosine, phenylalanine and deoxyguanosine oxidation products by liquid chromatography-tandem mass spectrometry as non-invasive biomarkers for oxidative damage. J Chromatogr B Anal Technol Biomed Life Sci. 2004;799:245–54.
Shaikh SR, Fessler MB, Gowdy KM. Role for phospholipid acyl chains and cholesterol in pulmonary infections and inflammation. J Leukoc Biol. 2016;100:985–97.
Marseglia L, D’Angelo G, Manti S, Salpietro C, Arrigo T, Barberi I. et al. Melatonin and atopy: role in atopic dermatitis and asthma. Int J Mol Sci. 2014;15:13482–93.
Hansen AM, Mathiesen L, Pedersen M, Knudsen LE. Urinary 1-hydroxypyrene (1-HP) in environmental and occupational studies-a review. Int J Hyg Environ Health. 2008;211:471–503.
Chotirmall SH, Gellatly SL, Budden KF, Mac Aogain M, Shukla SD, Wood DL, et al. Microbiomes in respiratory health and disease: an Asia-Pacific perspective. Respirology. 2017;22:240–50.
Hilty M, Burke C, Pedro H, Cardenas P, Bush A, Bossley C, et al. Disordered microbial communities in asthmatic airways. PLoS One. 2010;5:e8578.
Thorsen J, Rasmussen MA, Waage J, Mortensen M, Brejnrod A, Bønnelykke K, et al. Infant airway microbiota and topical immune perturbations in the origins of childhood asthma. Nat Commun. 2019;10:5001.
Larsen JM. The immune response to Prevotella bacteria in chronic inflammatory disease. Immunology. 2017;151:363–74.
Ege MJ, Mayer M, Schwaiger K, Mattes J, Pershagen G, van Hage M, et al. Environmental bacteria and childhood asthma. Allergy. 2012;67:1565–71.
Bourguignon N, Isaac P, Alvarez H, Amoroso MJ, Ferrero MA. Enhanced polyaromatic hydrocarbon degradation by adapted cultures of actinomycete strains. J Basic Microbiol. 2014;54:1288–94.
Nissen JD, Lykke K, Bryk J, Stridh MH, Zaganas I, Skytt DM, et al. Expression of the human isoform of glutamate dehydrogenase, hGDH2, augments TCA cyclecapacity and oxidative metabolism of glutamate during glucose deprivation in astrocytes. Glia. 2017;65:474–88.
Ducker GS, Rabinowitz JD. One-carbon metabolism in health and disease. Cell Metab. 2017;25:27–42.
Wishnok JS, Tannenbaum SR, Stillwell WG, Glogowski JA, Leaf CD. Urinary markers for exposures to alkylating or nitrosating agents. Environ Health Perspect. 1993;99:155–9.
Perera F, Tang WY, Herbstman J, Tang D, Levin L, Miller R, et al. Relation of DMA methylation of 5’-CpGisland of ACSL3 to transplacental exposure to airborne polycyclic aromatic hydrocarbons and childhood asthma. PLoS One. 2009;4:e4488.
De Bont R, van Larebeke N. Endogenous DNA damage in humans: a review of quantitative data. Mutagenesis. 2004;19:169–85.
Funding
This work was supported by the National Natural Science Foundation of China (82073630, 81728018, and 81530088), Natural Science Foundation of Jiangsu Province (BK20161571), Natural Science Foundation of the Higher Education Institution of Jiangsu Province (16KJA330002), and the open project of the key laboratory of Modern Toxicology of Ministry Education Nanjing Medical University (NMUAMT201802). The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Conceptualization: LL and QW; formal analysis: JH and YB; funding acquisition: FC and QW; investigation: JH; resources: YB, ZZ, FC, and LL; and writing original draft: QW.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval and consent to participate
The Nanjing Medical University Clinical Research Ethics Committee, Nanjing, China, reviewed and approved the protocols of this study. Written informed consent was obtained from the participants’ parents for the use of samples in this study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
About this article
Cite this article
Hu, J., Bao, Y., Huang, H. et al. The preliminary investigation of potential response biomarkers to PAHs exposure on childhood asthma. J Expo Sci Environ Epidemiol 32, 82–93 (2022). https://doi.org/10.1038/s41370-021-00334-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41370-021-00334-4
Keyword
This article is cited by
-
Urine 2-hydroxyphenanthrene is associated with current asthma: evidence from NHANES 2007–2012
International Archives of Occupational and Environmental Health (2023)
-
Source identification and risk assessment of polycyclic aromatic hydrocarbons (PAHs) in air and dust samples of Lahore City
Scientific Reports (2022)
-
PAH-induced metabolic changes related to inflammation in childhood asthma
Environmental Science and Pollution Research (2022)