Abstract
Background
Recent evidence indicates that insulin resistance (IR) in obesity may develop independently in different organs, representing different etiologies toward type 2 diabetes and other cardiometabolic diseases. The aim of this study was to investigate whether IR in the liver and IR in skeletal muscle are associated with distinct metabolic profiles.
Methods
This study includes baseline data from 634 adults with overweight or obesity (BMI ≥ 27 kg/m2) (≤65 years; 63% women) without diabetes of the European Diogenes Study. Hepatic insulin resistance index (HIRI) and muscle insulin sensitivity index (MISI), were derived from a five-point OGTT. At baseline 17 serum metabolites were identified and quantified by nuclear-magnetic-resonance spectroscopy. Linear mixed model analyses (adjusting for center, sex, body mass index (BMI), waist-to-hip ratio) were used to associate HIRI and MISI with these metabolites. In an independent sample of 540 participants without diabetes (BMI ≥ 27 kg/m2; 40–65 years; 46% women) of the Maastricht Study, an observational prospective population-based cohort study, 11 plasma metabolites and a seven-point OGTT were available for validation.
Results
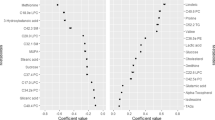
Both HIRI and MISI were associated with higher levels of valine, isoleucine, oxo-isovaleric acid, alanine, lactate, and triglycerides, and lower levels of glycine (all p < 0.05). HIRI was also associated with higher levels of leucine, hydroxyisobutyrate, tyrosine, proline, creatine, and n-acetyl and lower levels of acetoacetate and 3-OH-butyrate (all p < 0.05). Except for valine, these results were replicated for all available metabolites in the Maastricht Study.
Conclusions
In persons with obesity without diabetes, both liver and muscle IR show a circulating metabolic profile of elevated (branched-chain) amino acids, lactate, and triglycerides, and lower glycine levels, but only liver IR associates with lower ketone body levels and elevated ketogenic amino acids in circulation, suggestive of decreased ketogenesis. This knowledge might enhance developments of more targeted tissue-specific interventions to prevent progression to more severe disease stages.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kelly T, Yang W, Chen CS, Reynolds K, He J. Global burden of obesity in 2005 and projections to 2030. Int J Obes. 2008;32:1431–7.
Hruby A, Manson JE, Qi L, Malik VS, Rimm EB, Sun Q, et al. Determinants and consequences of obesity. Am J Public Health. 2016;106:1656–62.
Primeau V, Coderre L, Karelis AD, Brochu M, Lavoie ME, Messier V, et al. Characterizing the profile of obese patients who are metabolically healthy. Int J Obes. 2011;35:971–81.
Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006;444:840–6.
Shulman GI. Ectopic fat in insulin resistance, dyslipidemia, and cardiometabolic disease. N Engl J Med. 2014;371:1131–41.
Stinkens R, Goossens GH, Jocken JW, Blaak EE. Targeting fatty acid metabolism to improve glucose metabolism. Obes Rev. 2015;16:715–57.
Rask-Madsen C, Kahn CR. Tissue-specific insulin signaling, metabolic syndrome, and cardiovascular disease. Arterioscler Thromb Vasc Biol. 2012;32:2052–9.
Yu H, Zhou D, Jia W, Guo Z. Locating the source of hyperglycemia: liver versus muscle. J Diabetes. 2012;4:30–6.
Zheng J, Woo SL, Hu X, Botchlett R, Chen L, Huo Y, et al. Metformin and metabolic diseases: a focus on hepatic aspects. Front Med. 2015;9:173–86.
Blanco-Rojo R, Alcala-Diaz JF, Wopereis S, Perez-Martinez P, Quintana-Navarro GM, Marin C, et al. The insulin resistance phenotype (muscle or liver) interacts with the type of diet to determine changes in disposition index after 2 years of intervention: the CORDIOPREV-DIAB randomised clinical trial. Diabetologia. 2016;59:67−76.
Otten J, Stomby A, Waling M, Isaksson A, Soderstrom I, Ryberg M, et al. A heterogeneous response of liver and skeletal muscle fat to the combination of a Paleolithic diet and exercise in obese individuals with type 2 diabetes: a randomised controlled trial. Diabetologia. 2018;61:1548–59.
Klein MS, Shearer J. Metabolomics and type 2 diabetes: translating basic research into clinical application. J Diabetes Res. 2016;2016:3898502.
Pallares-Mendez R, Aguilar-Salinas CA, Cruz-Bautista I, Del Bosque-Plata L. Metabolomics in diabetes, a review. Ann Med. 2016;48:89–102.
Palmer ND, Okut H, Hsu FC, Ng MCY, Chen YI, Goodarzi MO, et al. Metabolomics identifies distinctive metabolite signatures for measures of glucose homeostasis: the Insulin Resistance Atherosclerosis Family Study (IRAS-FS). J Clin Endocrinol Metab. 2018;103:1877–88.
van der Kolk BW, Vogelzangs N, Jocken JWE, Valsesia A, Hankemeier T, Astrup A, et al. Plasma lipid profiling of tissue-specific insulin resistance in human obesity. Int J Obes. 2019;43:989−98.
Larsen TM, Dalskov S, van Baak M, Jebb S, Kafatos A, Pfeiffer A, et al. The diet, obesity and genes (diogenes) dietary study in eight European countries—a comprehensive design for long-term intervention. Obes Rev. 2010;11:76–91.
Schram MT, Sep SJ, van der Kallen CJ, Dagnelie PC, Koster A, Schaper N, et al. The Maastricht Study: an extensive phenotyping study on determinants of type 2 diabetes, its complications and its comorbidities. Eur J Epidemiol. 2014;29:439–51.
Abdul-Ghani MA, Matsuda M, Balas B, DeFronzo RA. Muscle and liver insulin resistance indexes derived from the oral glucose tolerance test. Diabetes Care. 2007;30:89–94.
Wurtz P, Kangas AJ, Soininen P, Lawlor DA, Davey Smith G, Ala-Korpela M. Quantitative serum nuclear magnetic resonance metabolomics in large-scale epidemiology: a primer on -omic technologies. Am J Epidemiol. 2017;186:1084–96.
Laffel L. Ketone bodies: a review of physiology, pathophysiology and application of monitoring to diabetes. Diabetes Metab Res Rev. 1999;15:412–26.
Soeters MR, Sauerwein HP, Faas L, Smeenge M, Duran M, Wanders RJ, et al. Effects of insulin on ketogenesis following fasting in lean and obese men. Obesity. 2009;17:1326–31.
Cobb J, Eckhart A, Perichon R, Wulff J, Mitchell M, Adam KP, et al. A novel test for IGT utilizing metabolite markers of glucose tolerance. J Diabetes Sci Technol. 2015;9:69–76.
Suhre K, Meisinger C, Doring A, Altmaier E, Belcredi P, Gieger C, et al. Metabolic footprint of diabetes: a multiplatform metabolomics study in an epidemiological setting. PLoS One. 2010;5:e13953.
Wurtz P, Makinen VP, Soininen P, Kangas AJ, Tukiainen T, Kettunen J, et al. Metabolic signatures of insulin resistance in 7098 young adults. Diabetes. 2012;61:1372–80.
Vice E, Privette JD, Hickner RC, Barakat HA. Ketone body metabolism in lean and obese women. Metabolism. 2005;54:1542–5.
Mahendran Y, Vangipurapu J, Cederberg H, Stancakova A, Pihlajamaki J, Soininen P, et al. Association of ketone body levels with hyperglycemia and type 2 diabetes in 9398 Finnish men. Diabetes. 2013;62:3618–26.
Pietilainen KH, Naukkarinen J, Rissanen A, Saharinen J, Ellonen P, Keranen H, et al. Global transcript profiles of fat in monozygotic twins discordant for BMI: pathways behind acquired obesity. PLoS Med. 2008;5:e51.
Newgard CB, An J, Bain JR, Muehlbauer MJ, Stevens RD, Lien LF, et al. A branched-chain amino acid-related metabolic signature that differentiates obese and lean humans and contributes to insulin resistance. Cell Metab. 2009;9:311–26.
Wang TJ, Larson MG, Vasan RS, Cheng S, Rhee EP, McCabe E, et al. Metabolite profiles and the risk of developing diabetes. Nat Med. 2011;17:448–53.
Pedersen HK, Gudmundsdottir V, Nielsen HB, Hyotylainen T, Nielsen T, Jensen BA, et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature. 2016;535:376–81.
Mardinoglu A, Gogg S, Lotta LA, Stancakova A, Nerstedt A, Boren J, et al. Elevated plasma levels of 3-hydroxyisobutyric acid are associated with incident type 2 diabetes. EBioMedicine. 2018;27:151–5.
Giesbertz P, Daniel H. Branched-chain amino acids as biomarkers in diabetes. Curr Opin Clin Nutr Metab Care. 2016;19:48–54.
Herman MA, She P, Peroni OD, Lynch CJ, Kahn BB. Adipose tissue branched chain amino acid (BCAA) metabolism modulates circulating BCAA levels. J Biol Chem. 2010;285:11348–56.
Lackey DE, Lynch CJ, Olson KC, Mostaedi R, Ali M, Smith WH, et al. Regulation of adipose branched-chain amino acid catabolism enzyme expression and cross-adipose amino acid flux in human obesity. Am J Physiol Endocrinol Metab. 2013;304:E1175–87.
She P, Van Horn C, Reid T, Hutson SM, Cooney RN, Lynch CJ. Obesity-related elevations in plasma leucine are associated with alterations in enzymes involved in branched-chain amino acid metabolism. Am J Physiol Endocrinol Metab. 2007;293:E1552–63.
Shimomura Y, Obayashi M, Murakami T, Harris RA. Regulation of branched-chain amino acid catabolism: nutritional and hormonal regulation of activity and expression of the branched-chain alpha-keto acid dehydrogenase kinase. Curr Opin Clin Nutr Metab Care. 2001;4:419–23.
Burrill JS, Long EK, Reilly B, Deng Y, Armitage IM, Scherer PE, et al. Inflammation and ER stress regulate branched-chain amino acid uptake and metabolism in adipocytes. Mol Endocrinol. 2015;29:411–20.
Badoud F, Lam KP, DiBattista A, Perreault M, Zulyniak MA, Cattrysse B, et al. Serum and adipose tissue amino acid homeostasis in the metabolically healthy obese. J Proteome Res. 2014;13:3455–66.
Saad MJ, Santos A, Prada PO. Linking gut microbiota and inflammation to obesity and insulin resistance. Physiology. 2016;31:283–93.
Wurtz P, Soininen P, Kangas AJ, Ronnemaa T, Lehtimaki T, Kahonen M, et al. Branched-chain and aromatic amino acids are predictors of insulin resistance in young adults. Diabetes Care. 2013;36:648–55.
Seibert R, Abbasi F, Hantash FM, Caulfield MP, Reaven G, Kim SH. Relationship between insulin resistance and amino acids in women and men. Physiol Rep. 2015;3:5.
Adeva-Andany M, Souto-Adeva G, Ameneiros-Rodriguez E, Fernandez-Fernandez C, Donapetry-Garcia C, Dominguez-Montero A. Insulin resistance and glycine metabolism in humans. Amino Acids. 2018;50:11–27.
Floegel A, Stefan N, Yu Z, Muhlenbruch K, Drogan D, Joost HG, et al. Identification of serum metabolites associated with risk of type 2 diabetes using a targeted metabolomic approach. Diabetes. 2013;62:639–48.
Sparks JD, Sparks CE, Adeli K. Selective hepatic insulin resistance, VLDL overproduction, and hypertriglyceridemia. Arterioscler Thromb Vasc Biol. 2012;32:2104–12.
Magkos F, Patterson BW, Mohammed BS, Klein S, Mittendorfer B. Women produce fewer but triglyceride-richer very low-density lipoproteins than men. J Clin Endocrinol Metab. 2007;92:1311–8.
Wang X, Magkos F, Mittendorfer B. Sex differences in lipid and lipoprotein metabolism: it’s not just about sex hormones. J Clin Endocrinol Metab. 2011;96:885–93.
Muniyappa R, Tella SH, Sortur S, Mszar R, Grewal S, Abel BS, et al. Predictive accuracy of surrogate indices for hepatic and skeletal muscle insulin sensitivity. J Endocr Soc. 2019;3:108–18.
Acknowledgements
The present study and the work of NV were supported through a grant from the Maastricht University Medical Center+. The Diogenes Study was supported by the European Commission, Food Quality, and Safety Priority of the Sixth Framework Program (FP6-2005-513946). The Maastricht Study was supported by the European Regional Development Fund via OP-Zuid, the Province of Limburg, the Dutch Ministry of Economic Affairs (grant 31O.041), Stichting De Weijerhorst (Maastricht, the Netherlands), the Pearl String Initiative Diabetes (Amsterdam, the Netherlands), the Cardiovascular Center (CVC, Maastricht, the Netherlands), Cardiovascular Research Institute Maastricht (CARIM, Maastricht, the Netherlands), School for Public Health and Primary Care (CAPHRI, Maastricht, the Netherlands), School for Nutrition, Toxicology and Metabolism (NUTRIM, Maastricht, the Netherlands), Stichting Annadal (Maastricht, the Netherlands), Health Foundation Limburg (Maastricht, the Netherlands) and by unrestricted grants from Janssen-Cilag B.V. (Tilburg, the Netherlands), Novo Nordisk Farma B.V. (Alphen aan den Rijn, the Netherlands), and Sanofi-Aventis Netherlands B.V. (Gouda, the Netherlands). The study sponsors were not involved in the design of the study; the collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
AV is full-time employee at Nestlé Institute of Health Sciences SA. WHMS reports having received research support from several food companies, such as Nestlé, DSM, Unilever, Nutrition et Sante, and Danone as well as Pharmaceutical companies, such as GSK, Novartis, and Novo Nordisk; he is an unpaid scientific advisor for the International Life Science Institute, ILSI Europe. AA reports grants and personal fees from McCain Foods, personal fees from Dutch Beer Knowledge Institute, the Netherlands, personal fees from Gelesis, personal fees from Novo Nordisk, Denmark, outside the submitted work, and royalties received for the book first published in Danish as Verdens Bedste Kur (Politiken; Copenhagen, Denmark), and subsequently published in Dutch as Het beste dieet ter wereld (Kosmos Uitgevers; Utrecht/Antwerpen, the Netherlands), in Spanish as Plan DIOGENES para el control del peso. La dieta personalizada inteligente (Editorial Evergra ́ficas; Léon, Spain), and in English as World’s Best Diet (Penguin, Australia). EEB receives grant support from food industry, such as DSM, Danone, Friesland Campina, Avebe, and Sensus, partly within the context of public–private consortia and has received funding from pharmaceutical companies like Novartis. She is involved in several task forces/expert groups related to the International Life Science Institute, ILSI Europe. All other authors report no possible conflicts of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Vogelzangs, N., van der Kallen, C.J.H., van Greevenbroek, M.M.J. et al. Metabolic profiling of tissue-specific insulin resistance in human obesity: results from the Diogenes study and the Maastricht Study. Int J Obes 44, 1376–1386 (2020). https://doi.org/10.1038/s41366-020-0565-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-020-0565-z
This article is cited by
-
Body composition and body fat distribution in tissue-specific insulin resistance and in response to a 12-week isocaloric dietary macronutrient intervention
Nutrition & Metabolism (2024)
-
Hepatic insulin resistance and muscle insulin resistance are characterized by distinct postprandial plasma metabolite profiles: a cross-sectional study
Cardiovascular Diabetology (2024)
-
Metabolic phenotyping in people living with obesity: Implications for dietary prevention
Reviews in Endocrine and Metabolic Disorders (2023)
-
Precision nutrition for targeting pathophysiology of cardiometabolic phenotypes
Reviews in Endocrine and Metabolic Disorders (2023)
-
A 12-week consumer wearable activity tracker-based intervention reduces sedentary behaviour and improves cardiometabolic health in free-living sedentary adults: a randomised controlled trial
Journal of Activity, Sedentary and Sleep Behaviors (2022)