Abstract
Introduction:
Biomarkers and physiomarkers may be useful adjunct tests for sepsis detection in neonatal intensive care unit (NICU) patients. We studied whether measuring plasma cytokines at the time of suspected sepsis could identify patients with bacteremia in centers in which patients were undergoing continuous physiomarker screening using a heart rate characteristics (HRC) index monitor.
Results:
Six cytokines were higher in Gram-negative bacteremia (GNB) than in Gram-positive bacteremia or candidemia (GPBC). A cytokine score using thresholds for granulocyte colony–stimulating factor (G-CSF), interleukin (IL)-6, IL-8, and tumor necrosis factor (TNF)-α had 100% sensitivity and 69% positive predictive value (PPV) for GNB. A single cytokine marker, IL-6 < 130 pg/ml, had 100% sensitivity and 52% PPV for sepsis ruled out (SRO). The average HRC index was abnormal in this cohort of patients with clinical suspicion of sepsis and did not discriminate between the final sepsis designations.
Discussion:
In summary, in NICU patients with suspected late-onset sepsis, plasma cytokines can identify those with SRO and those with GNB, potentially aiding in decisions regarding therapy.
Methods:
Seven cytokines were measured in 226 plasma samples from patients >3 d old with sepsis suspected based on clinical signs, abnormal HRC index, or both. Cases were classified as SRO, clinical sepsis (CS), GPBC, or GNB.
Similar content being viewed by others
Main
Infants in the neonatal intensive care unit (NICU) are highly susceptible to late-onset sepsis, with rates as high as 25% among preterm very-low-birth-weight infants. This is an important public health problem because mortality and morbidity are substantial (1), and survivors are at increased risk for neurodevelopmental impairment (2). The standard paradigm for diagnosing and treating late-onset sepsis is to perform a blood culture and initiate empiric two-antibiotic therapy after an infant displays signs possibly attributable to sepsis. With this approach, mortality is high, particularly in cases of Gram-negative septicemia. Discovering ways to detect sepsis in its early phases and to tailor antibiotic therapy to the likely causative organism could improve outcomes. On the other hand, avoidance of unnecessary antibiotic therapy is also a worthy goal. To this end, biomarkers and physiomarkers associated with neonatal sepsis have been investigated.
Cytokines have been proposed as promising biomarkers because some of them rise very early in the course of bacteremia (3) and thus are more sensitive for detecting the early phase of sepsis than acute-phase proteins such as C-reactive protein (CRP) (4). This was demonstrated by Kuster et al. in a prospective study of preterm infants in which blood levels of interleukin (IL)-6 and IL-1 receptor antagonist (IL-1ra) rose 1–2 d before the clinical presentation of blood culture–proven sepsis (5). Performing routine biomarker screening of asymptomatic NICU patients is not practicable, yet waiting for overt signs of sepsis to develop can lead to unfavorable outcomes. To address this problem, our group developed a system for continuous physiomarker (heart rate characteristics (HRC)) screening for sepsis in NICU patients.
Abnormal HRC have been identified in NICU patients with sepsis and often occur prior to clinical deterioration (6,7,8). Bacteremia can trigger a systemic inflammatory response with release of cytokines and subsequent physiologic changes in multiple organs including the heart. Two such changes identified in septic neonates are decreased beat-to-beat variability and repetitive transient decelerations in heart rate (9) similar to the changes seen in fetuses in the settings of asphyxia or chorioamnionitis (10,11). Our group has shown in a rodent model that pathogen toxins induce heart rate decelerations and decreased variability, in part through increased production of cytokines such as tumor necrosis factor (TNF)-α. In NICU patients, abnormal HRC associated with sepsis are not apparent to clinicians using conventional cardiorespiratory monitoring, prompting development of a monitor that detects HRC predictive of impending clinical deterioration. Through analysis of electrocardiogram data from hundreds of preterm infants, an HRC index was derived that incorporates decreased variability and decelerations to calculate the fold increase in risk that a patient will be diagnosed with sepsis in the next 24 h (7,8,12,13,14). After testing and validating the HRC index for sepsis detection, the impact of continuous HRC index monitoring on outcomes of very-low-birth-weight preterm infants was tested in a randomized clinical trial of 2,989 patients in eight centers, completed in 2010. This trial showed a significant decrease in mortality in preterm infants whose HRC index was continuously displayed to clinicians (15).
Further refinement is essential for optimizing biomarker and physiomarker screening for sepsis in NICU patients. We undertook this study for two purposes: (i) to determine if cytokine screening could discriminate between patients with sepsis ruled out and those with clinical or blood culture–positive sepsis, and (ii) to determine the relationship between abnormal HRC index and elevated cytokine levels in NICU patients with clinically suspected late-onset sepsis.
Results
Study sample
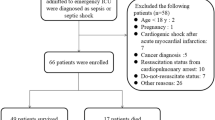
A total of 226 plasma samples were obtained near the time of blood culture from 163 patients. Gestational age was 28.7 ± 4.7 wk, and birth weight was 1,311 ± 861 g (mean ± SD). Based on retrospective chart review, major signs or findings leading to blood culture were grouped as follows: gastrointestinal (feeding intolerance, ileus, necrotizing enterocolitis interocolitis, peritonitis), respiratory (apnea, acute respiratory distress), central nervous system (CNS; temperature instability, lethargy, irritability), skin (cellulitis, wound infection), abnormal blood test (hyperglycemia, acidosis, abnormal white blood cell count, bandemia, thrombocytopenia), abnormal HRC index without other signs, and miscellaneous or not specified. In 10 of 226 cases, the blood culture was obtained because of abnormal HRC index alone. In the remaining cases, the major reason for blood culture was designated as gastrointestinal (67 cases), respiratory (67), CNS(29), skin (12), laboratory findings alone (16), and miscellaneous or not specified (25).
Samples were classified as sepsis ruled out (SRO, n = 98), clinical sepsis (CS, n = 95), Gram-positive bacteremia or candidemia (GPBC, n = 24), or Gram-negative bacteremia (GNB, n = 9). Organisms in the positive blood cultures were coagulase-negative staphylococcus species (n = 16), Staphylococcus aureus (4), Enterococcus fecalis (3), Escherichia coli (3), Klebsiella species (3), Pseudomonas aeruginosa (1), Enterobacter cloacae (1), Raoultella ornithinolytica (1), and Candida species (2). One sample yielded two organisms (coagulase-negative staphylococcus species and Candida).
Cytokines
Six of the seven cytokines (all except IL-1 receptor antagonist) were significantly higher in patients with CS as compared with those with SRO, whereas only one cytokine (interferon γ-inducible protein-10 (IP-10)) was significantly higher in GPBC as compared with SRO ( Figure 1 ). Samples associated with GNB had significantly higher levels of six cytokines (all except IP-10) as compared with those associated with GPBC (all P< 0.05). There were no significant differences in any cytokine in patients with CS vs. GPBC.
Plasma cytokine levels are higher in NICU patients with Gram-negative bacteremia (GNB). Seven cytokines were analyzed in 226 plasma samples from NICU patients >3 d old with suspected sepsis, subsequently classified as sepsis ruled out (SRO, n = 98), clinical sepsis (CS, n = 95), Gram-positive bacteremia or candidemia (GPBC, n = 24), or GNB, n = 9. Depicted are pg/ml amounts of (top row) IL-6, TNF-α, G-CSF, IL-8, (bottom row) IL-10, IL-1ra, and IP-10, as indicated on the y-axis. *P < 0.05 vs. SRO; **P < 0.05 GNB vs. GPBC. G-CSF, granulocyte colony–stimulating factor; IL, interleukin; IL-1ra, IL-1 receptor antagonist; IP, inducible protein; NICU, neonatal intensive care unit; TNF-α, tumor necrosis factor-α.
Hierarchical cluster analysis of cytokines from the 33 plasma samples associated with a positive blood culture showed two distinct clusters of cytokine profiles. Gram-negative organisms were substantially enriched in the cluster of samples with the highest cytokine levels, whereas samples associated with other organisms exhibited lower cytokine levels ( Figure 2 ). Thresholds for each cytokine were established to identify all cases of GNB. Although approaches that result in empirical sensitivities of 100% necessarily overestimate performance, this is a reasonable way to identify optimal thresholds and combinations of cytokines in data with a large separation among groups. All possible combinations of the seven cytokines were tested to determine the optimum combination for identifying all GNB cases. The 127 combinations had 100% sensitivity (by design), with positive predictive values (PPVs) ranging from 5 to 69% (median = 53%). There were eight combinations that achieved the maximum performance of 69% PPV, and only one of these combinations included as few as four cytokines. Based on this analysis, the following four cytokines and thresholds were used to generate a cytokine score: granulocyte colony–stimulating factor (G-CSF; 1,000 pg/ml), IL-6 (400 pg/ml), IL-8 (200 pg/ml), and TNF-α (32 pg/ml). Assigning a 1 or 0 based on these thresholds, a cytokine score of 4 had 100% sensitivity and negative predictive value for identifying patients with GNB, with 69% PPV ( Table 1 ).
Hierarchical cluster analysis of cytokine levels in all 33 cases of blood culture–positive sepsis. Plasma cytokine levels were normalized to thresholds that identified all cases of Gram-negative bacteremia (set to zero in the color scale, depicted in black). Numbers between the scale and the cluster diagram indicate log 10-transformed thresholds for each cytokine set to identify all cases of Gram-negative bacteremia. Cytokine levels relative to this threshold are depicted in shades of red (higher) and green (lower). Analysis of all 33 cases of septicemia revealed clustering of Gram-negative organisms among the samples with the highest cytokine levels.
Four samples with a cytokine score of 4 were not associated with GNB, and in each case the patient was very ill. One patient had E. coli pneumonia, and the other three had severe gastrointestinal pathology (two cases of severe necrotizing enterocolitis and one case of gastric perforation with peritonitis).
Using the same strategy as that described for GNB, we tested cytokine thresholds (individual and combination) for identifying the 98 cases of SRO. The best-performing individual cytokine was IL-6 < 130 pg/ml, which gave 100% sensitivity and 52% PPV for SRO ( Table 2 ). Adding any other cytokine to IL-6, alone or in combination, did not result in a higher PPV.
CRP
CRP was measured in 177 of the 226 samples (78%). There were similar proportions of samples with CRP available for analysis in the four groups SRO, CS, GPBC, and GNB (75–82%). CRP was significantly correlated with each of the seven cytokines studied (IL-6 r = 0.52, G-CSF r = 0.50, IL-10 r = 0.46, IL-8 r = 0.39, IP-10 r = 0.39, TNF-α r = 0.29, IL-1ra r = 0.21, all P < 0.01). There was no significant correlation of CRP with the HRC index. CRP was significantly higher in CS, GPBC, and GNB than in SRO, but not in GNB vs. GPBC ( Figure 3 ). A CRP of >6.2 mg/dl, set to be 100% sensitive for GNB, had only 16% PPV for GNB at the time of blood culture ( Table 1 ).
C-reactive protein (left) and cytokine score (right) in cases of suspected late-onset sepsis. A total of 226 plasma samples from NICU patients >3 d old with suspected sepsis were analyzed for cytokines; 177 of these were analyzed for CRP. Samples were classified as indicated in Figure 1. Samples were assigned a cytokine score of 0–4 using thresholds for G-CSF, IL-6, IL-8, and TNF-α. *P < 0.05 vs. SRO, **P < 0.05 GNB vs. GPBC. CRP, C-reactive protein; G-CSF, granulocyte colony–stimulating factor; GNB, Gram-negative bacteremia; GPBC, Gram-positive bacteremia or candidemia; IL, interleukin; NICU, neonatal intensive care unit; SRO, sepsis ruled out; TNF-α, tumor necrosis factor-α.
HRC Index
The HRC index was continuously monitored in all patients at Center A and in very-low-birth-weight infants at Center B. Of the 226 samples for cytokine analysis, 188 had an associated HRC index available for analysis. For the other samples, either the patient was at Center B and not very low birth weight, or the HRC index was not available near the time of sample acquisition.
The HRC index was most correlated with plasma levels of IL-8 and IL-1ra (IL-8 r = 0.20, P = 0.004; IL-1ra r = 0.30, P< 0.0001) but less so with the other five cytokines (P value range from 0.06 for IL-6 to 0.97 for TNF-α) and with the cytokine score (P = 0.18). The average HRC index was 2.14 and was not significantly different in patients with SRO, CS, GPBC, or GNB (all P > 0.05). HRC index >2 had 43% sensitivity for GNB and HRC index <1 had 35% sensitivity for SRO ( Tables 1 and 2 ). Because 79 samples were obtained from infants whose HRC index was displayed to clinicians, which may have impacted decisions about obtaining blood cultures and duration of antibiotic therapy, we separately analyzed the 147 samples from patients whose HRC index was not displayed to clinicians. Again, we did not find significant differences among the groups (data not shown).
Discussion
Use of biomarker and physiomarker screening for late-onset sepsis in NICU patients has potential for improving outcomes by shortening the time from onset of infection to institution of appropriate antibiotic therapy. In this study of patients with clinically suspected sepsis, we discovered a four-cytokine combination that identified all patients with GNB and an IL-6 threshold that identified all patients with SRO. Cytokines performed less well for identifying patients with Gram-positive bacteremia. The average HRC index was abnormal in this cohort of patients with clinical suspicion of sepsis and did not discriminate between the final sepsis designations.
A number of studies in NICU patients have shown that measuring more than one biomarker has additional value over a single analyte in identifying patients with sepsis (4,16,17,18,19,20). Our study is the first, to our knowledge, to identify a cytokine combination with good diagnostic accuracy for GNB, likely due to our larger sample size. By including four analytes to assign a cytokine score, G-CSF, IL-6, IL-8, and TNF-α, we were able to identify all cases of GNB with a false-positive rate of 31%. Higher cytokine levels have been reported in plasma of adults with Gram-negative as compared with Gram-positive bacteremia (21,22,23). Endotoxin on Gram-negative organisms induces greater cytokine production by leukocytes as compared with toxins on Gram-positive bacteria (24), likely accounting, at least in part, for the higher incidence of septic shock, multiorgan dysfunction, and death in patients with Gram-negative septicemia. Early identification of patients infected with Gram-negative organisms, through cytokine screening at the time of blood culture, could lead to more timely initiation of broad-spectrum antibiotic combinations to more rapidly clear these highly virulent pathogens from the bloodstream and might also identify patients for adjunct therapies to combat the detrimental effects of cytokine overproduction. A biomarker screen for a high morbidity and high mortality condition such as sepsis should ideally have 100% sensitivity and negative predictive value, and we set our cytokine thresholds to achieve this, which incurs a high false-positive rate if a single cytokine is measured. We found that the single best cytokine for detecting all cases of GNB (IL-6 at >400 pg/ml) had only 38% PPV, whereas the highest PPV of 69% was achieved with a 4-cytokine combination, thus limiting the number of false-positive tests, which would result in overtreatment of some patients. Of note, all four patients in this study with a cytokine score of 4 without GNB were seriously ill, one with Gram-negative pneumonia and three with severe gastrointestinal pathology.
In addition to early identification of the highest-risk septic patients, another important goal in biomarker screening is the ability to rule out sepsis in patients with nonspecific signs. Empiric antibiotic therapy for “sepsis rule-outs” is exceedingly common in NICU patients in spite of increasing evidence of adverse effects of antibiotic overuse (25). IL-6 has been identified as a promising biomarker in other studies of neonates with suspected sepsis (4,26), and we also found that, of the seven cytokines we analyzed, IL-6 had the best diagnostic accuracy. In fact, no cytokine combination had better performance than IL-6 alone at identifying patients undergoing blood culture in whom sepsis was subsequently ruled out. With only 52% positive predictive value (i.e., 48% of samples with IL-6 < 130 pg/ml occurring in patients with a subsequent diagnosis of either clinical or blood culture–positive sepsis), this test would likely not be useful to clinicians for making a decision not to initiate antibiotic therapy in a patient with significant sepsis-like signs. In a patient with equivocal signs, however, a low plasma level of IL-6 might serve as a useful adjunct test to reinforce a clinician’s decision not to initiate antibiotic therapy, or to limit duration of antibiotics. It is unlikely that cytokine screening will ever achieve 100% positive predictive accuracy for ruling out sepsis in NICU patients because many cases of clinical sepsis or Gram-positive (particularly coagulase-negative staphylococcus) bacteremia may not induce a robust systemic inflammatory response.
Although we assayed cytokines only at the time of blood culture, other studies have shown that additional measurements of biomarkers a day later can increase the diagnostic accuracy of these assays (4,5,27). This is especially true of acute-phase proteins such as CRP, which rises 6–12 h after cytokines are released in the circulation as part of the host response to bacteremia. We found that a CRP threshold set to detect all cases of GNB at the time of blood culture had a very low PPV as compared with individual cytokines. Although follow-up assays such as CRP may be useful for decisions about early discontinuation of antibiotics, highly sensitive assays available “on demand” at the time of blood culture are essential for initial therapeutic decisions.
We performed this cytokine study in the course of a randomized clinical trial of physiomarker (HRC index) screening of NICU patients. The advantage of HRC index monitoring is that, unlike biomarker blood tests, it is a continuous, noninvasive measurement that can alert clinicians to physiologic changes associated with sepsis-like illness, sometimes prior to onset of clinical deterioration (6,7,8,12,28,29). In this study, we found that the HRC index was correlated with two cytokines but not with the final designation of sepsis ruled in or out. This is likely due in large part to the fact that we studied patients who had already progressed to having signs of sepsis, with an average HRC index of >2, as compared with a mean overall HRC index in preterm NICU patients of <1 (6). In some cases, such as the example shown in Figure 4a , a rise in the HRC index over the patient’s baseline together with elevated cytokines and CRP occurred in the setting of bacteremia. A rise in the HRC index can be associated with nonseptic conditions such as acute respiratory decompensation or severe apnea, as shown in Figure 4b . Further studies are needed to determine whether addition of a biomarker screen at the time of a rise in the HRC index over the patient’s baseline could assist in decisions about evaluation for sepsis or initiation or discontinuation of empiric antibiotic therapy.
Examples of heart rate characteristics (HRC) index, cytokine score, and C-reactive protein (CRP) in NICU patients with suspected late-onset sepsis. (a) A 29-wk infant underwent a sepsis workup on day 8 (vertical line) due to a rising HRC index and apnea. The HRC index is depicted by the wavy horizontal line 5 d before and after the blood culture, at which time the HRC index was 1.3 (solid circle). The cytokine score at the time of blood culture was elevated at 4 of 4 (asterisk) and CRP was elevated at 6.2 mg/dl (open circle). The blood culture was positive for Klebsiella oxytoca. (b) A 27 wk infant with chronic lung disease underwent a sepsis workup on day 59 (vertical line) due to acute respiratory deterioration. The HRC index was rising at the time of blood culture (solid circle), but the cytokine score was low (asterisk) and the C-reactive protein was low (open circle). Sepsis was ruled out. NICU, neonatal intensive care unit.
In clinical practice, sepsis-like signs, a rising HRC index, or a combination of the two may prompt clinicians to initiate antibiotic therapy until sepsis is ruled out with negative cultures. Cytokine screening may be useful for reducing antibiotic exposure in patients with a low index of suspicion for sepsis, and also for identifying the highest-risk group of septic patients, those with GNB, thus ensuring earlier institution of effective antibiotics and adjunct sepsis therapies to improve outcomes.
Methods
Plasma Collection
We collected remnant plasma from NICU patients >3 d old undergoing blood culture for suspected sepsis. Patients of all gestational ages were included. Samples were collected over an 18-mo period at two centers (University of Virginia, “Center A”, and Wake Forest University, “Center B”). Birth weight, gestational age, duration of antibiotic therapy, and blood culture results were recorded. Retrospective chart review was performed by a single neonatologist at each institution to determine the major reasons for obtaining a blood culture. Samples were classified as SRO (negative blood culture and antibiotics for <5 d), CS (negative blood culture but antibiotics continued ≥5 d), GPBC (a positive blood culture for Gram-positive bacteria or Candida in a patient with signs of sepsis), or GNB (a positive blood culture for Gram-negative bacteria in a patient with signs of sepsis). The decision to continue antibiotics for ≥5 d in the face of a negative blood culture or a single positive blood culture for coagulase-negative Staphylococcus was left to clinical judgment of the attending neonatologists at each institution. All patient information was deidentified, and the institutional review boards of each institution approved collection of remnant plasma samples with waiver of consent.
Plasma samples were obtained from EDTA-containing tubes that had been obtained for complete blood count at or near (within 6 h of) the time of blood culture. Following storage at 4°C for <24 h, blood was centrifuged and plasma stored at −80°C until batch analysis for cytokines.
Cytokine and CRP Analysis
Seven cytokines were measured using a multiplex antibody-coated bead array with dual-laser fluorometric detection (Milliplex; Millipore, Billerica, MA). Analytes included IL-6, IL-8, IL-10, IL-1ra, IP-10, TNF-α, and G-CSF. Samples were diluted 1:4 and assayed in duplicate according to the manufacturer’s instructions. Limit of detection was 3.2 pg/ml. Samples that were above or below the limit of detection were assigned the upper or lower limit of detection.
CRP was measured by immunoassay at the time of blood culture at Center B and at the end of the study, if sufficient plasma remained after cytokine testing, at Center A.
HRC Monitoring
The FDA-cleared HRC index monitor (HeRO; Medical Predictive Science, Charlottesville, VA) takes electrocardiogram data from existing ICU monitors and calculates the standard deviation of normal R wave to R wave intervals, sample entropy, and sample asymmetry. These three characteristics are used to generate the HRC index, the fold increase in risk that a patient will be diagnosed with sepsis in the next 24 h (6,12). The HeRO monitor continuously displays the HRC index, which is calculated every hour and reflects heart rate variability and decelerations over the previous 12 h. For the purpose of this study, maximum HRC index in the 12 h preceding blood culture was recorded.
Plasma samples for this study were collected during a randomized clinical trial in which very-low-birth-weight infants were randomized to having their HRC index displayed to clinicians or not displayed. HRC index data for this study were collected after completion of the randomized clinical trial. Patients >1,500 g birth weight had their HRC index visible to clinicians at Center A but not at Center B. Clinicians were educated about HRC in sepsis, but no course of action was prescribed for abnormal HRC index.
Statistical Analysis
Cytokines, CRP, and HRC index in the four groups SRO, CS, GPBC, and GNB were compared by Kruskal–Wallis analysis followed by Dunn’s multiple comparison tests. Correlation of HRC index and individual cytokines was assessed using Spearman correlation coefficients (GraphPad Prism version 4, San Diego, CA). P < 0.05 was considered statistically significant.
Hierarchical cluster analysis was performed on the seven cytokines in samples associated with a positive blood culture. For each cytokine, thresholds were established to give 100% sensitivity and negative predictive value for GNB. A separate analysis was performed to determine thresholds with 100% sensitivity and negative predictive value for SRO. Using these thresholds, we used MATLAB Bioinformatics Toolbox(MathWorks, Natick, MA) to test all 127 possible cytokine combinations for their positive predictive value for either GNB or SRO. Starting with two cytokines, it was determined whether one, the other, both, or neither were significantly associated with the outcome. We eliminated “neither,” so after the first step (22) – 1 possible combinations were tested. This process was repeated for each cytokine for a total of (27) – 1 or 127 combinations tested.
Statement of Financial Support
This work was supported by the following funding sources: NICHD 051609 (to K.D.F.), NIGMS 064640 (to J.R.M.), the Wallace H. Coulter Foundation Translational Research Award, and University of Virginia Children’s Hospital.
References
Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics 2002;110(2 Pt 1):285–91.
Stoll BJ, Hansen NI, Adams-Chapman I, et al. National Institute of Child Health and Human Development Neonatal Research Network. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA 2004;292:2357–65.
Ng PC, Lam HS . Biomarkers for late-onset neonatal sepsis: cytokines and beyond. Clin Perinatol 2010;37:599–610.
Ng PC, Cheng SH, Chui KM, et al. Diagnosis of late onset neonatal sepsis with cytokines, adhesion molecule, and C-reactive protein in preterm very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 1997;77:F221–7.
Küster H, Weiss M, Willeitner AE, et al. Interleukin-1 receptor antagonist and interleukin-6 for early diagnosis of neonatal sepsis 2 days before clinical manifestation. Lancet 1998;352:1271–7.
Griffin MP, Lake DE, Bissonette EA, Harrell FE Jr, O’Shea TM, Moorman JR . Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics 2005;116:1070–4.
Griffin MP, Lake DE, Moorman JR . Heart rate characteristics and laboratory tests in neonatal sepsis. Pediatrics 2005;115:937–41.
Griffin MP, O’Shea TM, Bissonette EA, Harrell FE Jr, Lake DE, Moorman JR . Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr Res 2003;53:920–6.
Griffin MP, Scollan DF, Moorman JR . The dynamic range of neonatal heart rate variability. J Cardiovasc Electrophysiol 1994;5:112–24.
Salafia CM, Ghidini A, Sherer DM, Pezzullo JC . Abnormalities of the fetal heart rate in preterm deliveries are associated with acute intra-amniotic infection. J Soc Gynecol Investig 1998;5:188–91.
Cao H, Lake DE, Ferguson JE 2nd, Chisholm CA, Griffin MP, Moorman JR . Toward quantitative fetal heart rate monitoring. IEEE Trans Biomed Eng 2006;53:111–8.
Griffin MP, Moorman JR . Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics 2001;107:97–104.
Griffin MP, O’Shea TM, Bissonette EA, Harrell FE Jr, Lake DE, Moorman JR . Abnormal heart rate characteristics are associated with neonatal mortality. Pediatr Res 2004;55:782–8.
Moorman JR, Lake DE, Griffin MP . Heart rate characteristics monitoring for neonatal sepsis. IEEE Trans Biomed Eng 2006;53:126–32.
Moorman J, Carlo WA, Kattwinkel J, et al. Mortality reduction by heart rate characteristics monitoring in very low birthweight neonates: a randomized trial. J Pediatr 2011; 159: 900–6; e-pub ahead of print.
Horisberger T, Harbarth S, Nadal D, Baenziger O, Fischer JE . G-CSF and IL-8 for early diagnosis of sepsis in neonates and critically ill children - safety and cost effectiveness of a new laboratory prediction model: study protocol of a randomized controlled trial [ISRCTN91123847]. Crit Care 2004;8:R443–50.
Berner R, Niemeyer CM, Leititis JU, et al. Plasma levels and gene expression of granulocyte colony-stimulating factor, tumor necrosis factor-alpha, interleukin (IL)-1beta, IL-6, IL-8, and soluble intercellular adhesion molecule-1 in neonatal early onset sepsis. Pediatr Res 1998;44:469–77.
Ng PC, Ang IL, Chiu RW, et al. Host-response biomarkers for diagnosis of late-onset septicemia and necrotizing enterocolitis in preterm infants. J Clin Invest 2010;120:2989–3000.
Kingsmore SF, Kennedy N, Halliday HL, et al. Identification of diagnostic biomarkers for infection in premature neonates. Mol Cell Proteomics 2008;7:1863–75.
Sherwin C, Broadbent R, Young S, et al. Utility of interleukin-12 and interleukin-10 in comparison with other cytokines and acute-phase reactants in the diagnosis of neonatal sepsis. Am J Perinatol 2008;25:629–36.
Engervall P, Andersson B, Björkholm M . Clinical significance of serum cytokine patterns during start of fever in patients with neutropenia. Br J Haematol 1995;91:838–45.
Engel A, Mack E, Kern P, Kern WV . An analysis of interleukin-8, interleukin-6 and C-reactive protein serum concentrations to predict fever, gram-negative bacteremia and complicated infection in neutropenic cancer patients. Infection 1998;26:213–21.
Kragsbjerg P, Holmberg H, Vikerfors T . Dynamics of blood cytokine concentrations in patients with bacteremic infections. Scand J Infect Dis 1996;28:391–8.
Akira S, Takeda K . Toll-like receptor signalling. Nat Rev Immunol 2004;4:499–511.
Cotton CM . Early, prolonged use of postnatal antibiotics increased the risk of necrotising enterocolitis. Arch Dis Child Educ Pract Ed 2010;95:94.
Gonzalez BE, Mercado CK, Johnson L, Brodsky NL, Bhandari V . Early markers of late-onset sepsis in premature neonates: clinical, hematological and cytokine profile. J Perinat Med 2003;31:60–8.
Arnon S, Litmanovitz I, Regev R, Lis M, Shainkin-Kestenbaum R, Dolfin T . The prognostic virtue of inflammatory markers during late-onset sepsis in preterm infants. J Perinat Med 2004;32:176–80.
Griffin MP, Lake DE, O’Shea TM, Moorman JR . Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr Res 2007;61:222–7.
Fairchild KD, O’Shea TM . Heart rate characteristics: physiomarkers for detection of late-onset neonatal sepsis. Clin Perinatol 2010;37:581–98.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raynor, L., Saucerman, J., Akinola, M. et al. Cytokine screening identifies NICU patients with Gram-negative bacteremia. Pediatr Res 71, 261–266 (2012). https://doi.org/10.1038/pr.2011.45
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2011.45
This article is cited by
-
Diagnosis of neonatal sepsis: the past, present and future
Pediatric Research (2022)
-
Vital signs as physiomarkers of neonatal sepsis
Pediatric Research (2022)
-
Introducing heart rate variability monitoring combined with biomarker screening into a level IV NICU: a prospective implementation study
European Journal of Pediatrics (2022)
-
Inflammatory cytokine response and reduced heart rate variability in newborns with hypoxic-ischemic encephalopathy
Journal of Perinatology (2017)
-
Cytokine profiling in healthy children shows association of age with cytokine concentrations
Scientific Reports (2017)