Abstract
Background:
Approximately 29–38% of all positive surgical margins (PSMs) at radical prostatectomy (RP) involve the apex. The prognostic significance of apical PSM remains unclear. We therefore compared the long-term oncologic outcomes of men with apical PSMs to those with negative PSMs, apical and other PSMs, and other PSMs at RP.
Methods:
The SEARCH (Shared Equal Access Regional Cancer Hospital) database was used to identify 4031 men with prostate cancer (PCa) managed with RP with complete pathologic grade and stage data. Margin status was categorized as negative, apex only, or other positive. Multivariable Cox regression models adjusted for pathologic stage and grade were developed to test the relationship between margin status and biochemical recurrence (BCR), metastases and PCa death.
Results:
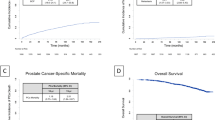
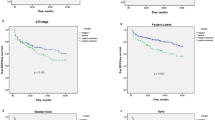
In the final cohort, 34.3% had PSMs, whereas 65.7% had negative margins. Univariable analysis showed that compared with negative margins, apex-only PSM was associated with BCR (hazard ratio (HR): 1.4 [1.1–1.8]), but not metastases or PCa death, whereas apex and other PSMs were associated with BCR (HR: 3.3 [2.8–4]) and metastases (HR: 1.8 [1.02–3.1]) but not PCa death. Nonapical PSMs were associated with BCR (HR: 2.7 [2.4–3.1]), metastases (1.7 [1.2–2.5)] and PCa death (1.8 [1.05–3]). On multivariable analysis, apex-only, apex and other, and nonapical PSMs were associated with BCR but margin status was not associated with metastases or PCa death.
Conclusions:
In a large cohort of men undergoing RP, those with PSMs at the prostatic apex had lower BCR, metastases, or PCa death compared with those with PSMs at other locations. When adjusted for pathologic stage and grade, however, PSMs were associated with BCR but not long-term oncologic outcomes. These data confirm that men with apex-only PSMs may not be ideal candidates for adjuvant therapy after RP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 4 print issues and online access
$259.00 per year
only $64.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Haas GP, Delongchamps N, Brawley OW, Wang CY, de la Roza G . The worldwide epidemiology of prostate cancer: perspectives from autopsy studies. Can J Urol 2008; 15: 3866–3871.
Siegel R, Naishadham D, Jemal A . Cancer statistics, 2013. CA Cancer J Clin 2013; 63: 11–30.
Ward JF, Zincke H, Bergstralh EJ, Slezak JM, Myers RP, Blute ML . The impact of surgical approach (nerve bundle preservation versus wide local excision) on surgical margins and biochemical recurrence following radical prostatectomy. J Urol 2004; 172 (4 Pt 1): 1328–1332.
Wright JL, Dalkin BL, True LD, Ellis WJ, Stanford JL, Lange PH et al. Positive surgical margins at radical prostatectomy predict prostate cancer specific mortality. J Urol 2010; 183: 2213–2218.
Izard JP, Salazar MA, Chatterjee S, Lin DW, Wright JL . Positive surgical margins at radical prostatectomy: population-based averages within PSA and Gleason strata. Can Urol Assoc J 2013; 7: E561–E566.
Eastham JA, Kuroiwa K, Ohori M, Serio AM, Gorbonos A, Maru N et al. Prognostic significance of location of positive margins in radical prostatectomy specimens. Urology 2007; 70: 965–969.
Mithal P, Howard LE, Aronson WJ, Terris MK, Cooperberg MR, Kane CJ et al. Positive surgical margins in radical prostatectomy patients do not predict long-term oncological outcomes: results from the Shared Equal Access Regional Cancer Hospital (SEARCH) cohort. BJU Int 2016; 117: 244–248.
Chalfin HJ, Dinizo M, Trock BJ, Feng Z, Partin AW, Walsh PC et al. Impact of surgical margin status on prostate-cancer-specific mortality. BJU Int 2012; 110: 1684–1689.
Rouanne M, Rode J, Campeggi A, Allory Y, Vordos D, Hoznek A et al. Long-term impact of positive surgical margins on biochemical recurrence after radical prostatectomy: ten years of follow-up. Scand J Urol 2014; 48: 131–137.
Secin FP, Serio A, Bianco FJ Jr, Karanikolas NT, Kuroiwa K, Vickers A et al. Preoperative and intraoperative risk factors for side-specific positive surgical margins in laparoscopic radical prostatectomy for prostate cancer. Eur Urol 2007; 51: 764–771.
Eastham JA, Kattan MW, Riedel E, Begg CB, Wheeler TM, Gerigk C et al. Variations among individual surgeons in the rate of positive surgical margins in radical prostatectomy specimens. J Urol 2003; 170 (6, Part 1): 2292–2295.
Atug F, Castle EP, Srivastav SK, Burgess SV, Thomas R, Davis R . Positive surgical margins in robotic-assisted radical prostatectomy: impact of learning curve on oncologic outcomes. Eur Urol 2006; 49: 866–871.
Vickers A, Bianco F, Cronin A, Eastham J, Klein E, Kattan M et al. The learning curve for surgical margins after open radical prostatectomy: implications for margin status as an oncological end point. J Urol 2010; 183: 1360–1365.
Tan PH, Cheng L, Srigley JR, Griffiths D, Humphrey PA, van der Kwast TH et al. International Society of Urological Pathology (ISUP) Consensus Conference on handling and staging of radical prostatectomy specimens. Working group 5: surgical margins. Mod Pathol 2011; 24: 48–57.
Karakiewicz PI, Eastham JA, Graefen M, Cagiannos I, Stricker PD, Klein E et al. Prognostic impact of positive surgical margins in surgically treated prostate cancer: multi-institutional assessment of 5831 patients. Urology 2005; 66: 1245–1250.
Pfitzenmaier J, Pahernik S, Tremmel T, Haferkamp A, Buse S, Hohenfellner M . Positive surgical margins after radical prostatectomy: do they have an impact on biochemical or clinical progression? BJU Int 2008; 102: 1413–1418.
Boorjian SA, Karnes RJ, Crispen PL, Carlson RE, Rangel LJ, Bergstralh EJ et al. The impact of positive surgical margins on mortality following radical prostatectomy during the prostate specific antigen era. J Urol 2010; 183: 1003–1009.
Hong YM, Hu JC, Paciorek AT, Knight SJ, Carroll PR . Impact of radical prostatectomy positive surgical margins on fear of cancer recurrence: Results from CaPSURE™. Urol Oncol 2010; 28: 268–273.
Grossfeld GD, Chang JJ, Broering JM, Miller DP, Yu J, Flanders SC et al. Impact of positive surgical margins on prostate cancer recurrence and the use of secondary cancer treatment: data from the CaPSURE database. J Urol 2000; 163: 1171–1177.
Cao D, Humphrey PA, Gao F, Tao Y, Kibel AS . Ability of linear length of positive margin in radical prostatectomy specimens to predict biochemical recurrence. Urology 2011; 77: 1409–1414.
Stephenson AJ, Wood DP, Kattan MW, Klein EA, Scardino PT, Eastham JA et al. Location, extent and number of positive surgical margins do not improve accuracy of predicting prostate cancer recurrence after radical prostatectomy. J Urol 2009; 182: 1357–1363.
Fesseha T, Sakr W, Grignon D, Banerjee M, Wood DP Jr, Pontes JE . Prognostic implications of a positive apical margin in radical prostatectomy specimens. J Urol 1997; 158: 2176–2179.
Kausik SJ, Blute ML, Sebo TJ, Leibovich BC, Bergstralh EJ, Slezak J et al. Prognostic significance of positive surgical margins in patients with extraprostatic carcinoma after radical prostatectomy. Cancer 2002; 95: 1215–1219.
Pettus JA, Weight CJ, Thompson CJ, Middleton RG, Stephenson RA . Biochemical failure in men following radical retropubic prostatectomy: impact of surgical margin status and location. J Urol 2004; 172: 129–132.
Vis AN, Schröder FH, van der Kwast TH . The actual value of the surgical margin status as a predictor of disease progression in men with early prostate cancer. Eur Urol 2006; 50: 258–265.
May M, Brookman-May S, Weissbach L, Herbst H, Gilfrich C, Papadopoulos T et al. Solitary and small (</=3 mm) apical positive surgical margins are related to biochemical recurrence after radical prostatectomy. Int J Urol 2011; 18: 282–289.
Shikanov S, Song J, Royce C, Al-Ahmadie H, Zorn K, Steinberg G et al. Length of positive surgical margin after radical prostatectomy as a predictor of biochemical recurrence. J Urol 2009; 182: 139–144.
Emerson RE, Koch MO, Jones TD, Daggy JK, Juliar BE, Cheng L . The influence of extent of surgical margin positivity on prostate specific antigen recurrence. J Clin Pathol 2005; 58: 1028–1032.
Marks RA, Koch MO, Lopez-Beltran A, Montironi R, Juliar BE, Cheng L . The relationship between the extent of surgical margin positivity and prostate specific antigen recurrence in radical prostatectomy specimens. Hum Pathol 2007; 38: 1207–1211.
Shikanov S, Marchetti P, Desai V, Razmaria A, Antic T, Al-Ahmadie H et al. Short (=1 mm) positive surgical margin and risk of biochemical recurrence after radical prostatectomy. BJU Int 2013; 111: 559–563.
Udo K, Cronin AM, Carlino LJ, Savage CJ, Maschino AC, Al-Ahmadie HA et al. Prognostic impact of subclassification of radical prostatectomy positive margins by linear extent and Gleason grade. J Urol 2013; 189: 1302–1307.
Katz R, Salomon L, Hoznek A, de la Taille A, Antiphon P, Abbou CC . Positive surgical margins in laparoscopic radical prostatectomy: the impact of apical dissection, bladder neck remodeling and nerve preservation. J Urol 2003; 169: 2049–2052.
Ploussard G, Drouin SJ, Rode J, Allory Y, Vordos D, Hoznek A et al. Location, extent, and multifocality of positive surgical margins for biochemical recurrence prediction after radical prostatectomy. World J Urol 2014; 32: 1393–1400.
Roder MA, Kawa S, Scheike T, Toft BG, Hansen JB, Brasso K et al. Non-apical positive surgical margins after radical prostatectomy for pT2 prostate cancer is associated with the highest risk of recurrence. J Surg Oncol 2014; 109: 818–822.
Ohori M, Abbas F, Wheeler TM, Kattan MW, Scardino PT, Lerner SP . Pathological features and prognostic significance of prostate cancer in the apical section determined by whole mount histology. J Urol 1999; 161: 500–504.
Ayala AG, Ro JY, Babaian R, Troncoso P, Grignon DJ . The prostatic capsule: does it exist? Its importance in the staging and treatment of prostatic carcinoma. Am J Surg Pathol 1989; 13: 21–27.
Kordan Y, Salem S, Chang SS, Clark PE, Cookson MS, Davis R et al. Impact of positive apical surgical margins on likelihood of biochemical recurrence after radical prostatectomy. J Urol 2009; 182: 2695–2701.
Stephenson AJ, Eggener SE, Hernandez AV, Klein EA, Kattan MW, Wood DP Jr et al. Do margins matter? The influence of positive surgical margins on prostate cancer-specific mortality. Eur Urol 2014; 65: 675–680.
Boorjian SA, Tollefson MK, Rangel LJ, Bergstralh EJ, Karnes RJ . Clinicopathological predictors of systemic progression and prostate cancer mortality in patients with a positive surgical margin at radical prostatectomy. Prostate Cancer Prostatic Dis 2012; 15: 56–62.
Thompson IM, Valicenti RK, Albertsen P, Davis BJ, Goldenberg SL, Hahn C et al. Adjuvant and salvage radiotherapy after prostatectomy: AUA/ASTRO Guideline. J Urol 2013; 190: 441–449.
Bolla M, van Poppel H, Tombal B, Vekemans K, Da Pozzo L, de Reijke TM et al. Postoperative radiotherapy after radical prostatectomy for high-risk prostate cancer: long-term results of a randomised controlled trial (EORTC trial 22911). Lancet 2012; 380: 2018–2027.
Thompson IM, Tangen CM, Paradelo J, Lucia MS, Miller G, Troyer D et al. Adjuvant radiotherapy for pathological T3N0M0 prostate cancer significantly reduces risk of metastases and improves survival: long-term followup of a randomized clinical trial. J Urol 2009; 181: 956–962.
Wiegel T, Bartkowiak D, Bottke D, Bronner C, Steiner U, Siegmann A et al. Adjuvant radiotherapy versus wait-and-see after radical prostatectomy: 10-year follow-up of the ARO 96-02/AUO AP 09/95 trial. Eur Urol 2014; 66: 243–250.
Cao D, Kibel AS, Gao F, Tao Y, Humphrey PA . The gleason score of tumor at the margin in radical prostatectomy is predictive of biochemical recurrence. Am J Surg Pathol 2010; 34: 994–1001.
Choo MS, Cho SY, Ko K, Jeong CW, Lee SB, Ku JH et al. Impact of positive surgical margins and their locations after radical prostatectomy: comparison of biochemical recurrence according to risk stratification and surgical modality. World J Urol 2014; 32: 1401–1409.
Sammon JD, Trinh QD, Sukumar S, Ravi P, Friedman A, Sun M et al. Risk factors for biochemical recurrence following radical perineal prostatectomy in a large contemporary series: a detailed assessment of margin extent and location. Urol Oncol 2013; 31: 1470–1476.
Vrang ML, Roder MA, Vainer B, Christensen IJ, Gruschy L, Brasso K et al. First Danish single-institution experience with radical prostatectomy: impact of surgical margins on biochemical outcome. Scand J Urol Nephrol 2012; 46: 172–179.
Blute ML, Bostwick DG, Bergstralh EJ, Slezak JM, Martin SK, Amling CL et al. Anatomic site-specific positive margins in organ-confined prostate cancer and its impact on outcome after radical prostatectomy. Urology 1997; 50: 733–739.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Wadhwa, H., Terris, M., Aronson, W. et al. Long-term oncological outcomes of apical positive surgical margins at radical prostatectomy in the Shared Equal Access Regional Cancer Hospital cohort. Prostate Cancer Prostatic Dis 19, 423–428 (2016). https://doi.org/10.1038/pcan.2016.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pcan.2016.45
This article is cited by
-
Diagnostic potential of radiological apical tumor involvement
Journal of Robotic Surgery (2022)
-
Preoperative staging using magnetic resonance imaging and risk of positive surgical margins after prostate-cancer surgery
Prostate Cancer and Prostatic Diseases (2019)
-
Positive margin length and highest Gleason grade of tumor at the margin predict for biochemical recurrence after radical prostatectomy in patients with organ-confined prostate cancer
Prostate Cancer and Prostatic Diseases (2018)