Abstract
Objective:
Alterations in inflammatory mediators are an important finding in neonates who develop bronchopulmonary dysplasia (BPD); however, there is a lack of research examining the relationship between multiple inflammatory mediators in premature neonates and the development of BPD. This study investigated whether the distribution of 12 inflammatory mediators detected in the tracheal aspirate (TA) of neonates within 24 h of birth could differentiate between neonates who did and who did not develop BPD.
Study design:
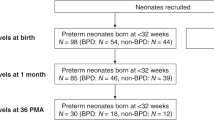
TA samples were collected from 27 very low birth weight neonates (BPD+=11), and the concentrations of 12 biomarkers associated with BPD were determined. Linear discriminant analysis (LDA) was used to classify neonates into two outcome groups.
Result:
LDA based on the 12 measured biomarkers displayed a significant level of discriminant function (P=0.007).
Conclusion:
Using linear discriminant analysis, predictive models of BPD can be generated. Our results suggest that multiple inflammatory mediators collected within 24 h of birth may be used to classify neonates into who will and who will not develop BPD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Jobe AH, Ikegami M . Prevention of bronchopulmonary dysplasia. Curr Opin Pediatr 2001; 13: 124–129.
Stoll BJ, Hansen NI, Bell EF, Shankaran S, Laptook AR, Walsh MC et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics 2010; 126: 443–456.
Speer CP . Inflammation and bronchopulmonary dysplasia: a continuing story. Semin Fetal Neonatal Med 2006; 11: 354–362.
Thompson A, Bhandari V . Pulmonary biomarkers of bronchopulmonary dysplasia. Biomark Insights 2008; 3: 361–373.
Bose CL, Dammann CE, Laughon MM . Bronchopulmonary dysplasia and inflammatory biomarkers in the premature neonate. Arch Dis Child Fetal Neonatal Ed 2008; 93: F455–F461.
Been JV, Debeer A, van Iwaarden JF, Kloosterboer N, Passos VL, Naulaers G et al. Early alterations of growth factor patterns in bronchoalveolar lavage fluid from preterm infants developing bronchopulmonary dysplasia. Pediatr Res 2010; 67: 83–89.
de Blic J, Midulla F, Barbato A, Clement A, Dab I, Eber E et al. Bronchoalveolar lavage in children. ERS Task Force on bronchoalveolar lavage in children. European Respiratory Society. Eur Respir J 2000; 15: 217–231.
Hand DJ . Discrimination and Classification. Wiley: New York, 1981.
Fitzpatrick AM, Higgins M, Holguin F, Brown LA, Teague WG . The molecular phenotype of severe asthma in children. J Allergy Clin Immunol 2010; 125: 851–857, e818.
Dawson B, Trapp RG . Basic & Clinical Biostatistics 4th ed McGraw-Hill: New York, 2004.
Ryan RM, Ahmed Q, Lakshminrusimha S . Inflammatory mediators in the immunobiology of bronchopulmonary dysplasia. Clin Rev Allergy Immunol 2008; 34: 174–190.
Merritt TA, Cochrane CG, Holcomb K, Bohl B, Hallman M, Strayer D et al. Elastase and alpha 1-proteinase inhibitor activity in tracheal aspirates during respiratory distress syndrome. Role of inflammation in the pathogenesis of bronchopulmonary dysplasia. J Clin Invest 1983; 72 (2): 656–666.
Acknowledgements
This study was supported in part by PHS Grant (TL1 RR025010) from the Clinical and Translational Science Award Program, National Institutes of Health, National Center for Research Resources (KRS) and the Childrens Healthcare of Atlanta Center for Developmental Lung Biology (TWG and LAB).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Schneibel, K., Fitzpatrick, A., Ping, XD. et al. Inflammatory mediator patterns in tracheal aspirate and their association with bronchopulmonary dysplasia in very low birth weight neonates. J Perinatol 33, 383–387 (2013). https://doi.org/10.1038/jp.2012.125
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2012.125
Keywords
This article is cited by
-
Association between probiotics and bronchopulmonary dysplasia in preterm infants
Scientific Reports (2021)
-
Increased serum Th2 chemokine levels are associated with bronchopulmonary dysplasia in premature infants
European Journal of Pediatrics (2019)
-
Respiratory consequences of prematurity: evolution of a diagnosis and development of a comprehensive approach
Journal of Perinatology (2015)
-
Exhaled breath condensate in intubated neonates- a window into the lung’s glutathione status
Respiratory Research (2014)