Abstract
Objective:
Necrotizing enterocolitis (NEC) remains a major cause of neonatal morbidity and mortality. Some infants recover uneventfully with medical therapy whereas others develop severe disease (that is, NEC requiring surgery or resulting in death). Repeated attempts to identify clinical parameters that would reliably identify infants with NEC most likely to progress to severe disease have been unsuccessful. We hypothesized that comprehensive prospective data collection at multiple centers would allow us to develop a model which would identify those babies at risk for progressive NEC.
Study Design:
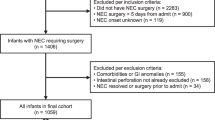
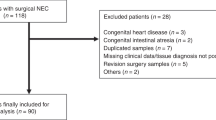
This prospective, observational study was conducted at six university children's hospitals. Study subjects were neonates with suspected or confirmed NEC. Comprehensive maternal and newborn histories were collected at the time of enrollment, and newborn clinical data were collected prospectively, thereafter. Multivariate logistic regression analysis was used to develop a predictive model of risk factors for progression.
Result:
Of 455 neonates analyzed, 192 (42%) progressed to severe disease, and 263 (58%) advanced to full feedings without operation. The vast majority of the variables studied proved not to be associated with progression to severe disease. A total of 12 independent predictors for progression were identified, including only 3 not previously described: having a teenaged mother (odds ratio, OR, 3.14; 95% confidence interval, CI, 1.45 to 6.96), receiving cardiac compressions and/or resuscitative drugs at birth (OR, 2.51; 95% CI, 1.17 to 5.48), and having never received enteral feeding before diagnosis (OR, 2.41; 95% CI, 1.08 to 5.52).
Conclusion:
Our hypothesis proved false. Rigorous prospective data collection of a sufficient number of patients did not allow us to create a model sufficiently predictive of progressive NEC to be clinically useful. It appears increasingly likely that further analysis of clinical parameters alone will not lead to a significant improvement in our understanding of NEC. We believe that future studies must focus on advanced biologic parameters in conjunction with clinical findings.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Blakely ML, Tyson JE, Lally KP, McDonald S, Stoll BJ, Stevenson DK et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis or isolated intestinal perforation in extremely low birth weight infants: Outcomes through 18 Months adjusted age. Pediatrics 2006; 117 (1): e680–e687.
Moss RL, Dimmitt RA, Barnhart DC, Sylvester KG, Brown RL, Powell DM et al. Laparotomy versus peritoneal drainage for necrotizing enterocolitis and perforation. N Engl J Med 2006; 354: 2225–2234.
Schulzke SM, Deshpande GC, Patole SK . Neurodevelopmental outcomes of very low-birth-weight infants with necrotizing enterocolitis. Arch Pediatr Adolesc Med 2007; 161: 583–590.
Hintz SR, Kendrick DE, Stoll BJ, Vohr BR, Fanaroff AA, Donovan EF et al. Neurodevelopmental and growth outcomes of extremely low birth weight infants after necrotizing enterocolitis. Pediatrics 2003; 115: 696–703.
Adams-Chapman I, Stoll BJ . Neonatal infection and long-term neurodevelopmental outcome in the preterm infant. Curr Opin Infect Dis 2006; 19 (3): 290–297.
Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L et al. Neonatal necrotizing enterocolitis: Therapeutic decisions based upon clinical staging. Ann Surg 1978; 187: 1–7.
Agresti A . Analysis of Categorical Data, 2nd edn. Wiley: New York, 2002.
SAS Institute Inc. SAS/STAT® User's Guide, Vols. 1, 2 and 3 SAS Institute Inc.: Cary, NC, 2002.
Nagelkerke NJD . A note on a general definition of the coefficient of determination. Biometrika 1991; 78: 691–692.
Hoy CM . The role of infection in necrotizing enterocolitis. Rev Med Microbiol 2001; 12 (3): 121–129.
Chan KL, Saing H, Yung RW, Yeung YP, Tsoi NS . The study of pre-antibiotic bacteriology in 125 patients with necrotizing enterocolitis. Acta Paediatr Suppl 1994; 396: 45–48.
Claud EC, Walker WA . Hypothesis: inappropriate colonization of the premature intestine can cause necrotizing enterocolitis. FASEB J 2001; 15: 1398–1403.
Balance WA, Dahms BB, Shenker N, Kliegman RM . Pathology of neonatal necrotizing enterocolitis: a ten year experience. J Pediatr 1990; 117 (1Pt2): s6–13.
Uauy RD, Fanaroff AA, Korones SB, Phillips EA, Phillips JB, Wright LL . Necrotizing enterocolitis in very low birth weight infants: biodemographic and clinical correlates. National Institutes of Health and Human Development Neonatal Research Network. J Pediatr 1991; 119 (4): 630–663.
McCormack CJ, Emmens RW, Putnam TC . Evaluation of factors in high risk neonatal necrotizing enterocolitis. J Pediatr Surg 1987; 22 (6): 488–491.
National Center for Health Statistics. Division of Vital statistics. Births: Preliminary Data for 2005 http://www.cdc.gov/nhs.
Stoll BJ . Epidemiology of necrotizing enterocolitis. Clin Perinatol 1994; 21: 205–218.
Lin PW, Stoll BJ . Necrotizing enterocolitis. Lancet 2006; 368: 1271–1283.
Holman RC, Stoll BJ, Curns AT, Yorita KL, Steiner CA, Schonberger LB . Necrotising enterocolitis hospitalisations among neonates in the United States. Paediatr Perinat Epidemiol 2006; 20 (6): 498–506.
Marchildon MB, Buck BE, Abdenour G . Necrotizing enterocolitis in the unfed infant. J Pediatr Surg 1982; 17 (5): 620–624.
Book LS, Herbst JJ, Jung AL . Comparison of fast and slow feeding rate schedules to the development of necrotizing enterocolitis. J Pediatr 1976; 89 (3): 463–466.
Rayyis SF, Ambalavaanan N, Wright L, Carlo WA . Randomized trial of slow versus fast feed advancements on the incidence of necrotizing enterocolitis in very low birth weight infants. J Pediatr 1999; 134 (3): 293–297.
Salhotra A, Ramji S . Slow versus fast enteral feed advancements in very low birth weight infants. A randomized controlled trial. Indian Pediatr 2004; 41: 435–441.
Caple J, Armentrout D, Huseby V, Halbardier B, Garcia J, Sparks JW et al. Randomized controlled trial of slow versus rapid feeding volume advancement in preterm infants. Pediatrics 2004; 114: 1597–1600.
Flidel-Rimon O, Friedman S, Lev E, Juster-Reicher A, Amitay M, Shinwell ES . Early enteral feeding and nosocomial sepsis in very low birthweight infants. Arch Dis Child Fetal Neonatal Ed 2004; 89: F289–F292.
Berseth CL, Bisquera JA, Paje VU . Prolonging small feeding volumes early in life decreases the incidence of necrotizing enterocolitis in very low birth weight infants. Pediatrics 2003; 111 (3): 529–534.
Kliegman RM . Experimental validation of neonatal feeding practices. Commentary. Pediatrics 1999; 103: 492–493.
Dunn L, Hulman S, Weiner J, Kliegman R . Beneficial effects of early hypocaloric enteral feeding on neonatal gastrointestinal function: preliminary report of a randomized trial. J Pediatr 1988; 112 (4): 622–629.
Forchiello ML, Walker WA . The effect of protective nutrients on mucosal defense in the immature intestine. Acta Paediatr 2005; 94 (s449): 74–83.
Schanler RJ, Schulman RJ, Lau C, Smith OE, Heitkemper M . Feeding strategies for premature infants: Randomized trial of gastrointestinal priming and tube-feeding method. Pediatrics 1999; 103: 434–439.
Tyson JE, Kennedy KA . Trophic feeding for parenterally fed infants. Cochrane Database of Systematic Reviews 2005; Issue 3. Art. No. CD000504. doi:10.1002/14651858.CD000504.pub2.
Kennedy KA, Tyson JE, Chamnanvanikij S . Early versus delayed initiation of progressive enteral feedings for parenterally fed low birth weight or preterm infants (Cochrane Review). Cochrane Database Syst Rev 2008; (2): CD001970; PMID: 18425878].
Kennedy KA, Tyson JE, Chamnanvanakij S . Rapid versus slow rate of advancement of feedings for promoting growth and preventing necrotizing enterocolitis in parentally fed low-birth-weight infants (Cochrane Review). Cochrane Database Syst Rev 2008; (2): CD001241; PMID: 18425870. [Review] [3 refs] [Journal Article. Review] Cochrane Database of Systematic Reviews. (2): CD001241, 2000. UI: 10796423
Rothman D, Udall JN, Pang KY et al. The effect of short-term starvation on mucosal barrier function in the newborn rabbit. Pediatr Res 1985; 19 (7): 727–731.
Burrin DG, Stoll B, Jiang R, Chang X, Hartmann B, Holst JJ et al. Minimal enteral nutrient requirements for intestinal growth in neonatal piglets: how much is enough? Am J Clin Nutr 2000; 71 (6): 1603–1610.
Acknowledgements
This study was supported in part by the Gerber Foundation and the Glaser Pediatric Research Network, an affiliate of the Elizabeth Glaser Pediatric AIDS Foundation.
The following persons and institutions have participated in this study: Bruna Banyas, RN, BSN, Monica Konstantino, RN, BSN, Joann Poulsen, RN, and Jan Taft, RN, BSN, Yale-New Haven Hospital; Geneva Shores, RN and Pam Gordon, RN, Texas Children's Hospital; Janet Mooney, RN, Department of Pediatrics, UCLA; Keniki McNeil, RN, Stanford University and Lucille Packard Children's Hospital; Carol Sweeney, BSN, Michael Wake, BA, and Laura Boger, BA, Children's Hospital, Boston; Marcia Wertz, RN, University of California Children's Hospital, San Francisco; Cami Martin, MD, Beth Israel Deaconess Medical Center, Boston. Moss, Kalish, Duggan, Johnston, Brandt, Dunn, Ehrenkranz, Jaksic, Nobuhara, Simpson, McCarthy and Sylvester have no financial disclosures to make regarding the contents and results of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moss, R., Kalish, L., Duggan, C. et al. Clinical parameters do not adequately predict outcome in necrotizing enterocolitis: a multi-institutional study. J Perinatol 28, 665–674 (2008). https://doi.org/10.1038/jp.2008.119
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jp.2008.119
Keywords
This article is cited by
-
A quality improvement initiative to standardize time to initiation of enteral feeds after non-surgical necrotizing enterocolitis using a consensus-based guideline
Journal of Perinatology (2022)
-
Machine learning-based risk factor analysis of necrotizing enterocolitis in very low birth weight infants
Scientific Reports (2022)
-
Characteristics and outcomes of a multi-institution cohort of infants with necrotizing enterocolitis totalis
Journal of Perinatology (2022)
-
Early versus late-onset necrotizing enterocolitis in very low birth infants in the neonatal intensive care unit
Pediatric Surgery International (2022)
-
Earlier re-initiation of enteral feeding after necrotizing enterocolitis decreases recurrence or stricture: a systematic review and meta-analysis
Journal of Perinatology (2020)