Abstract
In this study, we describe three unrelated Japanese patients with hearing loss and symphalangism who were diagnosed with proximal symphalangism (SYM1), atypical multiple synostosis syndrome (atypical SYNS1) and stapes ankylosis with broad thumb and toes (SABTT), respectively, based on the clinical features. Surgical findings in the middle ear were similar among the patients. By next-generation and Sanger sequencing analyses, we identified two novel mutations, c.559C>G (p.P178A) and c.682T>A (p.C228S), in the SYM1 and atypical SYNS1 families, respectively. No pathogenic changes were found in the protein-coding regions, exon–intron boundaries or promoter regions of the NOG, GDF5 or FGF9 genes in the SABTT family. Such negative molecular data suggest there may be further genetic heterogeneity underlying SYNS1, with the involvement of at least one additional gene. Stapedotomy resulted in good hearing in all patients over the long term, indicating no correlation between genotype and surgical outcome. Given the overlap of the clinical features of these syndromes in our patients and the molecular findings, the diagnostic term ‘NOG-related-symphalangism spectrum disorder (NOG-SSD)’ is advocated and an unidentified gene may be responsible for this disorder.
Similar content being viewed by others
Introduction
Proximal symphalangism (SYM1) with conductive hearing loss was first described in 1960 by Vesell.1 In 1999, Gong et al.2 found that mutation in the NOG gene was responsible for SYM1. This gene encodes a secreted protein, noggin, a bone morphogenetic protein antagonist essential for normal bone and joint development in humans and mice.3 NOG gene mutations leading to aberrant functions of the noggin protein have been found in some syndromes involving digital anomalies, including SYM1,1 multiple synostosis syndrome (SYNS1),4 facioaudiosymphalangism,5 tarsal–carpal coalition syndrome,6, 7 stapes ankylosis with broad thumb and toes (SABTT)8 and brachydactyly type B2.9 Because these syndromes share several overlapping features, it is sometimes difficult to reach an exact diagnosis. Given the overlapping clinical features and shared genetic cause of these syndromes with symphalangism, the collective term NOG-related symphalangism spectrum disorder (NOG-SSD) was proposed by Potti et al.10 in 2011. Following this proposed terminology, the same mutation in the NOG gene was reported in these overlapping syndromes with symphalangism.2, 11 In addition to NOG mutations, mutations in growth differentiation factor-5 (GDF5) on chromosome 20q11.2 or in fibroblast growth factor 9 (FGF9) on chromosome 13q12 have been found in patients with SYNS1.12, 13 However, as the GDF5 protein interacts with the NOG protein,14, 15 the diagnostic category of NOG-SSD does appear to be promising.
In this study, we present the clinical findings, including surgical results for hearing loss, and the molecular findings of the NOG, GDF5 and FGF9 genes for three unrelated Japanese patients clinically diagnosed with SYM1, SYNS1 or SABTT. Our results are consistent with the advocated disease category of NOG-SSD.
Patients and methods
Three affected patients from unrelated families were investigated. The patients’ clinical histories, including hearing loss and symphalangism, were taken and physical examinations, including otoscopy, hearing tests and computed tomography of the temporal bones, were conducted. All patients were examined for the presence of conductive hearing loss, symphalangism, hyperopia, broad thumbs or great toes, syndactyly and fusion of vertebrae. Hearing level was defined as the average of the hearing threshold at 0.5, 1.0, 2.0 and 4.0 kHz determined by pure-tone audiometry. Stapedius reflex tests were performed using standard audiometric procedures and equipment. High-resolution temporal bone computed tomography scans were performed to identify middle or inner ear malformations. All patients underwent radiographic scans to identify possible fusion of the bones in the hands or feet. Stapes surgery was performed in three patients to restore hearing loss.
Before enrollment, all patients provided written informed consent. The research protocol was approved by the Ethical Review Board of the University of the Ryukyus, Japan.
NOG genotyping
Next-generation sequencing
Genomic DNA was extracted from whole blood using a QIAamp DNA Blood Mini Kit (Qiagen, Hilden, Germany). Targeted resequencing of the NOG gene, including the promoter region, was performed by next-generation sequencing following long and accurate PCR. The NOG genomic region, spanning 6.5 kb (including a 3.5-kb upstream region), was amplified by long-range PCR with the primer pair 5′-GTCCAAAGGTGTTGGAGTTGATTTCAG-3′ and 5′-AGGCTGTGAGCCTTGTTGATTCCAAG-3′. The amplicon was then purified and fragmented using a Covaris sonicator (Covaris, Woburn, MA, USA). The fragmented DNA was end-repaired and ligated with an adapter for next-generation sequencing. The target DNA was sequenced with a GS Junior System (Roche, Basel, Switzerland).
Sanger sequencing
To confirm the coding sequences and substitutions, the NOG gene was Sanger sequenced using three primer pairs (primer sequences are available on request) in six subjects. PCR was performed as follows: initial denaturation at 94 °C for 5 min; 35 cycles of 94 °C for 40 s, 64 °C for 40 s, and 72 °C for 1 min; and a final extension at 72 °C for 5 min. PCRs were run using a programmable thermal cycler (Verti 96-Well Thermal Cycler; Applied Biosystems, Foster City, CA, USA). PCR products were purified using a Wizard SV Gel and PCR Clean-Up System (Promega, Madison, WI, USA) and directly sequenced using an ABI PRISM 3130xl Genetic Analyzer (Applied Biosystems). The sequences obtained were aligned and compared using the BLAST program with known human genome sequences available in the GenBank database.
PCR–restriction fragment length polymorphism analysis of NOG mutations in control subjects
We surveyed the substitutions c.559C>G (p.P178A) and c.682T>A (p.C228A) in 200 healthy unrelated Japanese individuals used as controls. The genotypes of the c.559C>G (p.P178A) and c.682T>A (p.C228A) substitutions were detected by digestion of the PCR product with the restriction enzymes BtgI and HpyCH4V (both from New England Biolabs, Ipswich, MA, USA), respectively.
In silico analysis of substitutions
The Double Prediction Method16 was used for predicting the secondary structure of the proteins. To analyze the pathological effect of coding variants on protein function in each substitution, four different prediction programs were used: SIFT (http://sift.jcvi.org),17 PolyPhen-2 (http://genetics.bwh.harvard.edu/pph2/),18 PROVEAN (http://provean.jcvi.org)19 and Mutation Taster.20
Results
Case presentation
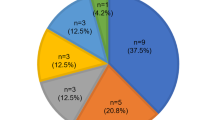
Table 1 presents a summary of the clinical findings of the three patients (1 man and 2 women; age range, 19–31 years). Patients 1 and 2, whose hearing loss appeared in childhood, wore hearing aids in both ears at the first visit to our hospital. All three patients had no history of ear disease-related hearing loss, such as chronic otitis media or cholesteatoma, and had similar otologic examination results. They had conductive hearing loss in both ears (Figure 3): bone conduction levels in both ears were almost normal and air conduction hearing levels ranged from 70 to 35 dB. They had a type A tympanogram, absence of the stapedius reflex and a normal eardrum under microscopic observation. Computed tomography scan showed no apparent ossicle malformation in either ear in any patient.
Patient 1 (patient III-2 in family 1)
A 22-year-old Japanese woman (III-2) was referred to our institution at age 16 years because of hearing loss since early childhood. The family pedigree is illustrated in Figure 1a. Her facial appearance is shown in Figures 2a and b. Her hands showed cutaneous syndactyly between the second and third digits and symphalangism in both distal interphalangeal joints of the fifth fingers (Figures 4a and b). Her feet also showed symphalangism in the third to fifth toes and short first toes of both feet (Figures 5a and b). Symphalangism in both little fingers and short proximal phalanges in both first toes were observed on X-ray examination (Figures 4b and 5b). Ophthalmologic examination displayed no abnormal findings such as hyperopia or strabismus. No facial dysmorphism was observed (Figures 2a and b). She underwent exploratory tympanotomy of the left ear at the age of 16 years that revealed ankylosis of the stapes footplate without incus fixation and congenital malformation of the ossicles. Stapedotomy was performed using a Teflon piston. Her postoperative hearing threshold improved to 25 dB in the left ear (Figure 3b) and has been stable for ⩾5 years after the surgery. A diagnosis of SYM1 was made based on the clinical findings.
Views and radiographs of the patients’ hands. (a, b) Patient 1, (c, d) patient 2 and (e, f) patient 3. (a, c, e) Views of hands and (b, d, f) radiographs of hands. Black arrows indicate symphalangism in (a) the distal interphalangeal joint and (c, d) proximal interphalangeal joint of the fifth fingers. Black arrowheads indicate cutaneous syndactyly. White arrowheads indicate short fifth fingers (brachydactyly).
Views and radiographs of the feet of the patients. (a, b) Patient 1, (c, d) patient 2 and (e, f) patient 3. (a, c, e) Views of feet and (b, d, f) radiographs of feet. Black arrows indicate short first toes. White arrows indicate symphalangism. Arrowheads indicate short proximal phalanges (hypoplasia).
Patient 2 (patient III-1 in family 2)
A 19-year-old Japanese man (III-1) was referred to us because of bilateral hearing loss since early childhood. His family pedigree is illustrated in Figure 1b. His hands showed symphalangism in both proximal interphalangeal joints of the fifth fingers (Figure 4c). Physical and X-ray examination of the feet revealed symphalangism in the fifth toes of both feet (Figures 5c and d). X-ray of the cervical vertebrae revealed fusion of C6–C7 without reduced motion of the neck. He wore glasses for bilateral hyperopia. Dysmorphology examination showed a hemicylindrical nose, hypoplastic nasal alae and thin upper vermilion (Figures 2c and d).
Exploratory tympanotomy in the left ear was performed at age 19 years and revealed ankylosis of the stapes footplate. Only slight immobility without malformation of the incus was detected and was considered acceptable. Stapedotomy was performed using a Teflon piston. His postoperative hearing threshold improved to 25 dB in the operated ear (Figure 3d) and his hearing level has remained stable for more than 2 years after surgery. A diagnosis of SYNS1 was made based on the clinical findings.
Patient 3 (patient II-5 in family 3)
A 31-year-old Japanese woman (II-5) was referred to our hospital at age 9 years because of hearing loss since early childhood. The family pedigree is illustrated in Figure 1c. Her facial appearance is shown in Figures 2e and f. Her son has conductive hearing loss without symphalangism or hyperopia. Physical examination of the hands revealed symphalangism in both proximal interphalangeal joints of the fifth fingers (Figure 4e), whereas both feet had symphalangism in the third to fifth toes (Figure 5e). Symphalangism and short intermediate phalanges in both fifth fingers were confirmed by X-ray examination (Figures 4f and 5f). Ophthalmologic examination revealed hyperopia. No facial dysmorphism was observed. Exploratory tympanotomy was performed in the left ear at age 9 years and 5 months later in her right ear. Ankylosis of the stapes footplate without incus fixation and malformation of the ossicles were evident in both ears. Stapedotomy was performed using a Teflon piston in both ears. Her postoperative hearing threshold in the left and right ears improved to 17 and 27 dB, respectively (Figure 3f), and her hearing level has been stable for 22 years after surgery. The diagnosis was SABTT based on the clinical findings.
Genetic analysis
Family 1
Next-generation sequence analysis revealed the presence of a heterozygous substitution in the NOG gene, c.559C>G (p.P178A) (Figure 6). The c.559C>G substitution in patient 1 (III-2) was confirmed by direct sequence analysis (Figure 6c). This substitution was not found in 200 controls.
NOG gene sequencing profiles for the patients. (a, b) Integrative genomics viewer images of next-generation sequencing analysis of the NOG gene. (c–f) Sanger sequencing diagram for the (c, d) patients and (e, f) wild types. (a, c) Patient with the c.559C>G (p.P178A) mutation and (b, d) patient with the c.682T>A (p.C228A) mutation. Arrows indicate the variant nucleotide.
Family 2
Molecular analyses were performed in patient 2 (III-1) and his parents (II-3, II-4). Next-generation sequencing analysis revealed the presence of a heterozygous substitution of the NOG gene, c.682T>A (p.C228A) (Figure 6). The c.682T>A substitution was identified in the father (II-3) and son (III-1) but not in the mother (II-4). The heterozygous c.682T>A substitution was confirmed by direct sequence analysis (Figure 6d). This substitution was not found in 200 controls.
Family 3
Molecular analyses were performed in patient 3 (II-5) and her son (III-1). Next-generation sequence analysis and direct sequence analysis of the NOG, GDF5 and FGF9 genes showed no pathogenic mutations in patient 3 (II-4) or her son (III-1) (data not shown).
Analysis of the secondary structure of the NOG protein
We identified two novel mutations, c.559C>G (p.P178A) and c.682T>A (p.C228S), in two of our patients, respectively. The secondary structure of the NOG protein was predicted to be altered from a random coil to an α-helix between A187 and E188 by the mutation of p.P187A (Figures 7a and b), leading to an extended strand between C184 and S185 (Figure 7b). The secondary structure of the mutated NOG protein p.C228S was altered from an extended strand to a random coil between S226 and E227 (Figures 7c and d). These conformational changes may inhibit dimer formation or interaction with other transforming growth factor-β family members, possibly leading to the clinical features constituting the proposed disease category of NOG-SSD.
Prediction of the secondary structure of NOG protein. (a, b) Wild-type P187 and P187A and (c, d) wild-type C228 and C228S. Arrows indicate targeted amino acids. c, random coil; DPM, double prediction method;16 e, extended strand; h, α-helix; t, β-turn.
In silico substitution analysis
The four prediction methods used to evaluate the potential impact of amino acid substitutions on the structure and function of the noggin precursor protein revealed that both mutations affected protein function, except for PolyPhen2 for P187A (Table 2).
Discussion
NOG mutations and diseases
We performed molecular investigation of three patients who showed overlapping clinical features of hearing loss and symphalangism. Next-generation and Sanger sequencing analyses revealed two novel mutations, c.559C>G (p.P178A) and c.682T>A (p.C228S), in the SYM1 and atypical SYNS1 families, respectively. These mutations have not been described previously and were not found in 200 controls. The predicted secondary structures of these mutated proteins were different from those of the wild-type protein. The NOG region amino acid 178 is located in the dimerization domain.9 The two novel substitutions of p.P187A and p.C228S affect the dimerization of the NOG protein. SIFT, PROVEAN and Mutation Taster, but not PolyPhen-2, predicted that both substitutions affect protein function. For mutation p.P187A, a different amino acid change at the same position, P187S, has also been reported as a pathological mutation disrupting the dimerization of the NOG protein in a patient with proximal symphalangism.9 The noggin protein contains seven cysteine residues within the carboxyl terminal region, matching the pattern found in the Kunitz-type protease inhibitor superfamily.21 The cysteine-rich Kunitz domain can mediate specific interaction with another protein by forming disulfide bonds between cysteine residues. The cysteine knot motif of the C-terminal domain of noggin was disrupted and noggin failed to function when these sites were mutated because of damage to the formation of disulfide bonds in noggin dimerization.22, 23 These data suggest that the two novel substitutions c.559C>G (p.P178A) and c.682T>A (p.C228S) are pathological.
Mutations in the NOG gene have been found in several syndromes, including SYM1,1 SYNS1,4 facioaudiosymphalangism,5 tarsal–carpal coalition syndrome,6, 7 SABTT8 and brachydactyly type B2,9 leading to the somewhat controversial proposal of the novel category NOG-SSD that combines the syndromes.10 Among our three patients, there is a marked overlap between the SYM1, atypical SYNS1 and SABTT syndromes with respect to the clinical features associated with joint-fusion syndromes (Table 3), supporting their assignment to the same spectrum with phenotypic variation. Further supporting evidence is that the same mutation of p.P35S in the NOG gene has been found in both tarsal–carpal coalition syndrome and SYM1.24 In the present study, variable phenotype expressivity was observed in each family, but our patients had overlapping symptoms with one another. In patient 1, we diagnosed the disorder as SYM1 because typical symptoms of SYM1 were displayed. In patient 2, we diagnosed atypical SYNS1 because the clinical features best matched the diagnostic criteria of SYNS1, although the patient was hyperopic. NOG mutations were found in both cases, lending support to the concept of NOG-SSD.
NOG-SSD may display locus heterogeneity, given that mutations in other genes such as GDF512, 25 and FGF913 have been reported in some families with the overlapping syndromes associated with symphalangism. In patient 3, because the diagnosis was typical SABTT, we examined the NOG gene, including its promoter region, by next-generation sequencing. However, no mutation was identified in the NOG gene or the promoter. We also examined the GDF5 and FGF9 genes in patient 3 by direct and next-generation sequencing, but found no pathological substitutions in the protein-coding regions, exon–intron boundaries or promoter regions of either gene. Such negative molecular data for family 3 indicate that there may be further genetic heterogeneity underlying SYNS1, with the involvement of at least one additional gene. In fact, two studies by Dawson et al.12 and van den Ende et al.26 found no mutations in either NOG or GDF5 in the patient with NOG-SSD. Moreover, they did not find any mutations in NOG, BMPR1B, GDF5 or FGF9 in a patient with a clinical phenotype showing features of SYNS1 or facioaudiosymphalangism, suggesting further genetic heterogeneity for these syndromes.
Surgery
In addition to stapes ankylosis, fixation of the short process of the incus in the fossa incudis has been reported in patients with NOG-SSD.8, 27, 28, 29, 30 In patient with incus fixation, incudal mobilization was required at the time of stapes surgery.8, 27, 28, 29, 30 In the present study, fixation of the incus was identified in patient 2, but because the immobility was considered acceptable, incudal mobilization was not performed and the outcome was hearing improvement with mild conductive hearing loss. Disappointing long-term results of stapes surgeries with proximal symphalangism syndrome have been reported.29, 31 The improved hearing threshold after stapes surgery deteriorates during the follow-up period because of a dislocated piston, a process considered to result from bony reclosure of the footplate.29, 31 Thus, partial stapedectomy or stapedectomy should be considered to prevent reclosure of the oval window.29, 31 In the present study, stapedotomy was performed in all patients and all retained good hearing over the long term (between 2 and >20 years). In view of our surgical outcomes, stapes surgery for conductive hearing loss in symphalangism spectrum disorder may be a good therapeutic option. Moreover, as the ossicular condition during surgery was not different among patients, there was no clear relationship between genotype and surgical outcome in our patients.
Conclusion
In three patients with overlapping clinical features of hearing loss and symphalangism, we identified two novel mutations, p.P187A and p.C228S, in the SYM1 and atypical SYNS1 families, respectively. The NOG gene mutations clearly give rise to a spectrum of clinical findings. The two novel NOG mutations identified lend support to the notion of NOG-related symphalangism spectrum disorder. We also found no pathogenic changes in the protein-coding regions, exon–intron boundaries or promoter regions of the NOG, GDF5 or FGF9 genes in the SABTT family, suggesting an unidentified gene may be responsible for this disorder. These two novel mutations and clinical manifestations in patients in this study will contribute to an understanding of NOG-SSD.
References
Vesell, E. S . Symphalangism, strabismus and hearing loss in mother and daughter. N. Engl. J. Med. 27, 839–842 (1960).
Gong, Y ., Krakow, D ., Marcelino, J ., Wilkin, D ., Chitayat, D ., Babul-Hirji, R . et al. Heterozygous mutations in the gene encoding noggin affect human joint morphogenesis. Nat. Genet. 21, 302–304 (1999).
Zimmerman, L. B ., De Jesus-Escobar, J. M . & Harland, R. M . The Spemann organizer signal noggin binds and inactivates bone morphogenetic protein 4. Cell 86, 599–606 (1996).
Maroteaux, P ., Bouvet, J. P . & Briard, M. L . Multiple synostosis disease. Nouv. Presse. Med. 1, 3041–3047 (1972).
Hurvitz, S. A ., Goodman, R. M ., Hertz, M, Katznelson, M. B . & Sack, Y . The facio-audio-symphalangism syndrome: report of a case and review of the literature. Clin. Genet. 28, 61–68 (1985).
Drawbert, J. P ., Stevens, D. B ., Cadle, R. G . & Hall, B. D . Tarsal and carpal coalition and symphalangism of the Fuhrmann type. Report of a family. J. Bone Joint Surg. Am 67, 884–889 (1985).
Gregersen, H. N . & Petersen, G. B . Congenital malformation of the feet with low body height. A new syndrome, caused by an autosomal dominant gene. Clin. Genet. 12, 255–262 (1977).
Teunissen, B . & Cremers, W. R . An autosomal dominant inherited syndrome with congenital stapes ankylosis. Laryngoscope 100, 380–384 (1990).
Lehmann, K ., Seemann, P ., Silan, F ., Goecke, T. O ., Irgang, S ., Kjaer, K. W . et al. A new subtype of brachydactyly type B caused by point mutations in the bone morphogenetic protein antagonist NOGGIN. Am. J. Hum. Genet. 81, 388–396 (2007).
Potti, T. A ., Petty, E. M . & Lesperance, M. M . A comprehensive review of reported heritable noggin-associated syndromes and proposed clinical utility of one broadly inclusive diagnostic term: NOG-related-symphalangism spectrum disorder (NOG-SSD). Hum. Mutat. 32, 877–886 (2011).
Dixon, M. E ., Armstrong, P ., Stevens, D. B . & Bamshad, M . Identical mutations in NOG can cause either tarsal/carpal coalition syndrome or proximal symphalangism. Genet. Med. 3, 349–353 (2001).
Dawson, K ., Seeman, P ., Sebald, E ., King, L ., Edwards, M ., Williams, J. 3rd et al. GDF5 is a second locus for multiple-synostosis syndrome. Am. J. Hum. Genet. 78, 708–712 (2006).
Wu, X. L ., Gu, M. M ., Huang, L ., Liu, X. S ., Zhang, H. X ., Ding, X. Y . et al. Multiple synostoses syndrome is due to a missense mutation in exon 2 of FGF9 gene. Am. J. Hum .Genet. 85, 53–63 (2009).
Chang, S. C ., Hoang, B ., Thomas, J. T ., Vukicevic, S ., Luyten, F. P ., Ryba, N. J . et al. Cartilage-derived morphogenetic proteins. New members of the transforming growth factor-beta superfamily predominantly expressed in long bones during human embryonic development. J. Biol. Chem. 269, 28227–28234 (1994).
Storm, E. E . & Kingsley, D. M GDF5 coordinates bone and joint formation during digit development. Dev. Biol. 209, 11–27 (1999).
Deleage, G . & Roux, B . An algorithm for protein secondary structure prediction based on class prediction. Protein Eng. 1, 284–294 (1987).
Ng, P. C . & Henikoff, S . Predicting deleterious amino acid substitutions. Genome Res. 11, 863–874 (2001).
Adzhubei, I. A ., Schmidt, S ., Peshkin, L ., Ramensky, V. E ., Gerasimova, A ., Bork, P . et al. A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Choi, Y ., Sims, G. E ., Murphy, S ., Miller, J. R . & Chan, A. P . Predicting the functional effect of amino acid substitutions and indels. PLoS ONE 7, e46688 (2012).
Schwarz, J. M ., Rödelsperger, C ., Schuelke, M . & Seelow, D . Mutation Taster evaluates disease-causing potential of sequence alterations. Nat. Methods 7, 575–576 (2010).
McDonald, N. Q . & Kwong, P. D . Does noggin head a new class of Kunitz domain? Trends Biochem. Sci. 18, 208–209 (1993).
Liu, W ., Ren, C ., Shi, J ., Feng, X ., He, Z ., Xu, L . et al. Characterization of the functionally related sites in the neural inducing gene noggin. Biochem. Biophys. Res. Commun. 270, 293–297 (2000).
Rudnik-Schöneborn, S ., Takahashi, T ., Busse, S ., Schmidt, T ., Senderek, J ., Eggermann, T . et al. Facioaudiosymphalangism syndrome and growth acceleration associated with a heterozygous NOG mutation. Am. J. Med. Genet. A 152A, 1540–1544 (2010).
Hirshoren, N ., Gross, M ., Banin, E ., Sosna, J ., Bargal, R . & Raas-Rothschild, A . P35S mutation in the NOG gene associated with Teunissen-Cremers syndrome and features of multiple NOG joint-fusion syndromes. Eur. J. Med. Genet. 51, 351–357 (2008).
Wang, X ., Xiao, F ., Yang, Q ., Liang, B ., Tang, Z ., Jiang, L . et al. A novel mutation in GDF5 causes autosomal dominant symphalangism in two Chinese families. Am. J. Med. Genet. A 140A, 1846–1853 (2006).
van den Ende, J. J ., Borra, V . & Van Hul, W . Negative mutation screening of the NOG, BMPR1B, GDF5, and FGF9 genes indicates further genetic heterogeneity of the facioaudiosymphalangism syndrome. Clin. Dysmorphol. 22, 1–6 (2013).
Thomeer, H. G ., Admiraal, R. J ., Hoefsloot, L ., Kunst, H. P . & Cremers, C. W . Proximal symphalangism, hyperopia, conductive hearing impairment, and the NOG gene: 2 new mutations. Otol. Neurotol. 32, 632–638 (2011).
Weekamp, H. H ., Kremer, H ., Hoefsloot, L. H ., Kuijpers-Jagtman, A. M ., Cruysberg, J. R . & Cremers, C. W . Teunissen-Cremers syndrome: a clinical, surgical, and genetic report. Otol. Neurotol. 26, 38–51 (2005).
Ensink, R. J ., Sleeckx, J. P . & Cremers, C. W . Proximal symphalangism and congenital conductive hearing loss: otologic aspects. Am. J. Otol. 20, 344–349 (1999).
Cremers, C ., Theunissen, E . & Kuijpers, W . Proximal symphalangia and stapes ankylosis. Arch. Otolaryngol. 111, 765–767 (1985).
Brown, D. J ., Kim, T. B ., Petty, E. M ., Downs, C. A ., Martin, D. M ., Strouse, P. J . et al. Characterization of a stapes ankylosis family with a NOG mutation. Otol. Neurotol. 24, 210–215 (2003).
Acknowledgements
This work was supported by the Japan Society for the Promotion of Science (JSPS) KAKENHI Grant-in-Aid for Scientific Research (C) No. 25462649.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ganaha, A., Kaname, T., Akazawa, Y. et al. Identification of two novel mutations in the NOG gene associated with congenital stapes ankylosis and symphalangism. J Hum Genet 60, 27–34 (2015). https://doi.org/10.1038/jhg.2014.97
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2014.97
This article is cited by
-
Identification of a novel nonsense NOG mutation in a patient with stapes ankylosis and symphalangism spectrum disorder
Human Genome Variation (2023)
-
Genetic and clinical phenotypic analysis of familial stapes sclerosis caused by an NOG mutation
BMC Medical Genomics (2020)
-
Identification of a novel mutation of NOG in family with proximal symphalangism and early genetic counseling
BMC Medical Genetics (2019)
-
Novel NOG (p.P42S) mutation causes proximal symphalangism in a four-generation Chinese family
BMC Medical Genetics (2019)
-
A novel nonsense mutation in the NOG gene causes familial NOG-related symphalangism spectrum disorder
Human Genome Variation (2016)