Abstract
Telavancin is a dual action, bactericidal lipoglycopeptide. Its in vitro activity was compared with vancomycin and linezolid against 392 Gram-positive isolates from cancer patients. MIC90 values (μg ml−1) for telavancin, vancomycin and linezolid were determined for methicillin-susceptible Staphylococcus aureus (MSSA), methicillin-resistant S. aureus (MRSA), methicillin-susceptible (MS), methicillin-resistant (MR), coagulase-negative staphylococci (CoNS), viridans group streptococci (VGS), Streptococcus pneumoniae, Bacillus species, Corynebacterium species and Micrococcus species. Telavancin had potent activity against β-hemolytic streptococci and Staphylococcus lugdunensis. Whereas 100% of MRSA and 98% of MSSA had vancomycin MICs ⩾1.0 μg ml−1 (minimum inhibitory concentrations (MICs) at which poor clinical responses have been reported), the highest telavancin MIC was 0.38 μg ml−1. For CoNS, 95% of MS and 100% of MR isolates had vancomycin MICs ⩾1.0 μg ml−1, whereas the highest telavancin MIC was 0.38 μg ml−1. Furthermore, 48% of VGS had vancomycin MICs ⩾1.0 μg ml−1, whereas the highest telavancin MIC was 0.064 μg ml−1. A similar pattern was noticed for S. lugdunensis, Bacillus species, Corynebacterium species and β-hemolytic streptococci. These data suggest that telavancin and linezolid have potent activity against most Gram-positive organisms that cause infections in cancer patients. Consequently, they may be considered as alternatives to vancomycin, especially in institutions wherein a substantial proportion of infections are caused by organisms with vancomycin MICs ⩾1.0 μg ml−1.
Similar content being viewed by others
Introduction
Infections occur frequently in cancer patients, especially in those with hematologic malignancies and profound neutropenia, but also in patients with solid tumors and with adequate neutrophil counts. Although geographic and institutional variations are known, Gram-positive organisms remain the predominant pathogens in this setting globally.1, 2 Staphylococcus species (coagulase-negative staphylococci (CoNS), Staphylococcus aureus) are isolated most often, but a wide spectrum of Gram-positive bacteria such as Enterococcus spp., viridans group streptococci, β-hemolytic streptococci, Bacillus spp., Corynebacterium spp. and Micrococcus spp., are not uncommon.3, 4 Organisms such as Listeria monocytogenes, Rhodococcus equi and Stomatococcus mucilaginosus are less common, but important pathogens. Occasionally, vancomycin-resistant organisms such as Leuconostoc spp., Lactobacillus spp. and Pediococcus spp. are also encountered.
For decades, vancomycin has been the agent of choice for the treatment of documented Gram-positive infections in neutropenic cancer patients, and has also been recommended by many as empiric therapy, when Gram-positive infections are strongly suspected.5, 6 These recommendations may now be outdated at several institutions owing to changing susceptibilities and other issues with vancomycin. Many centers are reporting declining vancomycin activity (the minimum inhibitory concentration (MIC) creep), tolerance (MBC ⩾32 times the MIC), and lack of bactericidal activity, especially among staphylococcal isolates.7, 8, 9 Clinical failures have been reported in staphylococcal infections caused by isolates with vancomycin MICs of 1.0–2.0 μg ml−1, regarded as vancomycin susceptible.10 Reports such as these have become frequent, and have led to the lowering of vancomycin-susceptibility/-resistance breakpoints for S. aureus by the Clinical Laboratory Standards Institute (CLSI).11 A recently published meta-analysis showed that infections caused by S. aureus isolates with vancomycin MICs of >1.5 μg ml−1 were associated with increased mortality irrespective of the source of infection or the MIC-testing method.12 Other studies have shown that MICs performed using the E-test method are more reliable for predicting treatment response compared with other susceptibility testing methods, although the E-test is considered by some to slightly overestimate the MICs.13 Consequently, clinical laboratories are now being asked to consider using E-test MIC determination for all MRSA bloodstream isolates.12, 13 Guidelines for the treatment of MRSA infections recommend that clinical response should determine the administration of vancomycin for isolates with a vancomycin MIC of ⩽2.0 μg ml−1 whereas, for isolates with a vancomycin MIC >2.0 μg ml−1, an alternative to vancomycin should be used.14 Agents such as linezolid and daptomycin are considered alternatives but clinical data for these agents in cancer patients is minimal and each agent is associated with some limitations. Telavancin, a novel, dual action lipoglycopeptide, is reported to be rapidly bactericidal against Gram-positive cocci.15, 16 We believe that this agent might be a potential alternative to vancomycin in neutropenic cancer patients. Consequently, we compared it’s in vitro activity to vancomycin and linezolid against recent clinical isolates obtained from cancer patients being treated at our institution (a comprehensive cancer center).
Results
The comparative in vitro activities of telavancin, vancomycin and linezolid against 392 isolates representing at least 15 bacterial species are presented in Table 1.
Staphylococci
Of the 84 coagulase-negative staphylococcal isolates tested, 7, all Staphylococcus lugdunensis, were identified down to species level. All seven were inhibited by 0.25 μg ml−1 of telavancin which had lower MICs than vancomycin (MIC range, 0.75–1.5 μg ml−1) and linezolid (MIC range, 0.38–0.75 μg ml−1). Only one isolate was inhibited by <1.0 μg ml−1 of vancomycin. Of the remaining 77 CoNS isolates, 55 (71%) were MR. All 22 MS isolates were inhibited by ⩽0.38 μg ml−1 of telavancin (MIC range, 0.06–0.38 μg ml−1). In contrast, 21 of 22 isolates (95%) had vancomycin MICs of ⩾1.0 μg ml−1 (range, 0.75–3.0 μg ml−1). All 22 were inhibited by ⩽1.5 μg ml−1 of linezolid (range, 0.5–1.5 μg ml−1). Similarly, in all 55 MR-CoNS isolates were inhibited by ⩽0.38 μg ml−1 of telavancin (range, 0.125–0.38 μg ml−1), whereas all 55 (100%) had vancomycin MICs of >1 μg ml−1 (range, 1.5–4.0 μg ml−1). Fifty of these isolates (91%) were inhibited by ⩽1.5 μg ml−1 of linezolid (range, 0.38–1.5 μg ml−1). The five remaining isolates revealed high levels of linezolid resistance, with MICs of ⩾256 μg ml−1 for each isolate.
Of the 106 S. aureus isolates tested, 56(53%) were MSSA. All 56 were inhibited by ⩽0.38 μg ml−1 of telavancin (range, 0.25–0.38 μg ml−1), whereas all 56 had vancomycin MICs of ⩾1.0 μg ml−1 (range, 1.0–1.5 μg ml−1). The MIC90 for linezolid against these isolates was 1.5 μg ml−1 (range, 0.75–2.0 μg ml−1). All 50 MRSA isolates were inhibited by ⩽0.38 μg ml−1 of telavancin (range, 0.064–0.38 μg ml−1), whereas 49 (98%) of these isolates had vancomycin MICs of ⩾1.0 μg ml−1 (range, 0.19–2 μg ml−1). All MRSA isolates were inhibited by ⩽2.0 μg ml−1 of linezolid (range, 0.75–2.0 μg ml−1).
Streptococci
Telavancin exhibited potent activity against viridans group streptococci, inhibiting all 27 isolates at ⩽0.064 μg ml−1 (range, 0.016–0.064 μg ml−1). Vancomycin inhibited 50% of these isolates at ⩽0.75 μg ml−1, and all 27 at ⩽1.5 μg ml−1 (range, 0.38–1.5 μg ml−1). The MIC90 for linezolid for these isolates was 1.5 μg ml−1 (range, 0.75–2.0 μg ml−1). Ten Streptococcus pneumoniae isolates were available for testing. Telavancin had the lowest MICs, inhibiting all ten at ⩽0.064 μg ml−1 (range, 0.012–0.064 μg ml−1). All pneumococcal isolates were also susceptible to vancomycin and linezolid. A total of 26 β-hemolytic streptococci (2-Group A; 11-Group B; 13-Group G) were tested. Telavancin exhibited potent activity against these organisms, inhibiting all 26 at 0.25 μg ml−1. All isolates were susceptible to linezolid and vancomycin as well, but these agents were less potent.
Enterococci
Thirty two Enterococcus faecalis-isolates were tested and were found to be susceptible to all three agents. Telavancin inhibited all 32 isolates at <0.38 μg ml−1, (which is below the Food and Drug Administration (FDA)-susceptibility breakpoint of ⩽1.0 μg ml−1), vancomycin at 3.0 μg ml−1, and linezolid at 4.0 μg ml−1. All 32 Enterococcus faecium isolates were resistant to vancomycin (VRE-MICs >256 μg ml−1). Linezolid inhibited 25 isolates (78%) at<4.0 μg ml−1 (range, 1.5–128.0 μg ml−1). Although telavancin had lower MICs for these isolates than vancomycin (range, 1.0–16.0 μg ml−1), only one isolate was inhibited by⩽1.0 μg ml−1.
Other Gram-positive organisms
Telavancin had potent in vitro activity against Bacillus spp., Corynebacterium spp. and Micrococcus spp. All Corynebacterium spp. (38 isolates) and all Micrococcus spp. (10 isolates) were also susceptible to vancomycin and linezolid. All 24 Bacillus spp. isolates were inhibited by <1.5 μg ml−1 of linezolid. However only 10 (31%) were inhibited by <1.0 μg ml−1 of vancomycin (range, 0.25–8.0 μg ml−1). Telavancin had potent activity against the two Listeria monocytogenes isolates and one Rhodococcus equi isolate available for testing. Linezolid and vancomycin were less active.
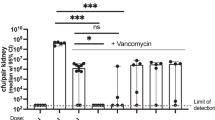
Although the significance of isolates with vancomycin MICs of ⩾1.0 μg ml−1 has only been established for S. aureus, and has not been established for telavancin, we determined the proportion of all species tested that had MICs ⩾1.0 μg ml−1 for both agents. These results are shown in Table 2. We excluded the 32 VRE isolates from this calculation, leaving a total of 360 isolates. Of these, 292 (81%) had vancomycin MICs ⩾1.0 μg ml−1, including 95% of MS-CoNS isolates, and 100% of MR- CoNS, 86% of S. lugdunensis, 100% of MSSA and 98% of MRSA isolates respectively. The highest telavancin MIC for these isolates was 0.38 μg ml−1. Additionally, 67% of Bacillus species, 50% of Corynebacterium species, 85% of β-hemolytic streptococci and 48% of viridans group streptococci also had vancomycin MICs ⩾1.0 μg ml−1. In contrast, only two isolates, both Bacillus spp., had telavancin MICs ⩾1.0 μg ml−1.
Discussion
Gram-positive organisms remain the predominant bacterial pathogens in cancer patients although some institutions are reporting a resurgence of Gram-negative infections.1, 2 Currently, ∼80% of bacteremias (including central line-associated bloodstream infections) and ∼50% of infections at all sites, have a Gram-positive component. CoNS are isolated most often, followed by S. aureus, viridans group streptococci and Enterococcus spp.17 Other Gram-positive organisms (Bacillus spp., Corynebacterium spp., Listeria monocytogenes, Rhodococcus equi, Micrococcus spp. and Stomatococcus mucilaginosus) are isolated with varying frequency. Consequently, empiric antimicrobial therapy in febrile neutropenic patients needs to provide coverage not just against staphylococci and streptococci, but against a much wider spectrum of Gram-positive pathogens. Additionally, many of the organisms listed above are resistant to the fluroquinolones and β-lactams, agents that are often used for the prevention and treatment of infections in cancer patients.
Until recently, vancomycin was considered to be the agent of choice for the treatment of Gram-positive infections in patients with cancer.5 In fact, previous iterations of the Infectious Diseases Society of America (IDSA) guidelines for the management of febrile neutropenic patients recommend the use of vancomycin when such infections are documented.18 These guidelines also outlined several indications for the empiric use of vancomycin. However, over the past 8–10 years, several reports have been published documenting vancomycin failures in staphylococcal infections caused by organisms considered to be susceptible to it, but with MICs ⩾1.0 μg ml−1.7, 10 Institutions worldwide, including our own, have documented an upward MIC creep with organisms such as S. aureus still being susceptible based on the revised CLSI-breakpoints, but having MICs of 1.0 μg ml−1 or more.7, 9, 17 Diminished vancomycin bactericidal activity has been documented against such isolates. These reports have raised concerns that vancomycin may no longer be the agent of choice for the treatment of infections caused by such isolates, especially in neutropenic patients in whom bactericidal agents are generally preferred.19 Because of these concerns, we conducted a retrospective review of MRSA bloodstream infections in cancer patients treated at our institution between January 2001 and June 2009 and found a high treatment failure rate (52%) for vancomycin.20 An independent predictor of infection–related mortality was infection by MRSA isolates with MICs of >2.0 μg ml−1. Based on this experience, we have developed clinical practice guidelines that recommend the use of alternative agents (for example, daptomycin or linezolid) when such infections are encountered in our patients. However, both these agents are associated with limitations, leaving room for the development and evaluation of other agents. Linezolid is bacteriostatic, and is associated with myelotoxicity particularly with prolonged usage, making it less than ideal in patients with hematologic malignancies and recipients of hematopoietic stem cell transplantation. There have also been reports of increasing resistance to linezolid often associated with increased usage.21 Although daptomycin does not have these limitations, it is inactivated by pulmonary surfactant. A substantial proportion of neutropenic patients (25–35%) develop pulmonary infiltrates precluding the use of daptomycin.
Unlike other studies evaluating the in vitro activity of telavancin, our study tested isolates obtained exclusively from patients with cancer, a substantial proportion of which were neutropenic. Our data demonstrate that at our institution, the majority of staphylococcal isolates and a substantial proportion of other Gram-positive isolates have vancomycin MICs ⩾1.0 μg ml−1. Our data also demonstrate that telavancin and linezolid have potent in vitro activity against most Gram-positive organisms that cause infections in neutropenic patients, including those with vancomycin MICs ⩾1.0 μg ml−1.15, 16 Telavancin inhibited all isolates with vancomycin MICs of ⩾1.0 μg ml−1 at a concentration of 0.38 μg ml−1. These findings are in line with those published by other investigators against isolates from the United States, Europe, Latin America and the Asia–Pacific region.16, 22, 23 It has potent in vitro activity against streptococci, Bacillus species and Corynebacterium species. It also has better activity than vancomycin against S. lugdunensis which has recently emerged as a significant pathogen in both immunocompetent and immunosuppressed patients.24 Additionally, telavancin has been shown to possess superior activity compared with vancomycin against multidrug-resistant S. aureus in a range of in vitro biofilm models suggesting that it might be potentially useful in the treatment of biofilm-mediated infections.25 Although not particularly active by itself against Enterococcus species that are vancomycin resistant (primarily E.faecium), telavancin possesses synergistic activity when combined with rifampin against E. faecium isolates resistant to both linezolid and vancomycin.26
Telavancin has been extensively evaluated for the treatment of complicated skin and skin structure infections and in 2009 received approval for this indication by the US Food and Drug Administration (FDA).27 It has also been evaluated for the treatment of adult patients with hospital-acquired and ventilator-associated bacterial pneumonia (HABP/VABP) and received FDA approval for this indication (HABP/VABP caused by susceptible strains of S.aureus when alternative agents are not suitable) in June 2013.28 Telavancin has been shown to be superior to vancomycin for the treatment of MRSA and glycopeptides-intermediate S. aureus in immune-compromised/neutropenic murine bacteremia models.29, 30 Although not formally evaluated in neutropenic patients, we believe that with its potent in vitro activity against a wide spectrum of Gram-positive pathogens, its dual mechanism of action (inhibition of bacterial cell wall synthesis and disruption of cell membrane function), and its rapid bactericidal activity, it has a potential play in the treatment of Gram-positive infections in neutropenic patients. Telavancin does have adverse effects including QTc prolongation, infusion-related reactions, and worsening of renal function particularly in patients with pre-existing moderate to severe renal impairment. Its use during pregnancy needs to be avoided unless the potential benefits outweigh the potential risk to the fetus. Nevertheless, with the increasing frequency of some neoplasms in an ageing population, and the use of hematopoietic stem cell transplantation for several indications, we believe that clinical evaluation of telavancin for the treatment of selected infections in neutropenic patients is warranted.
Materials and methods
Organisms
The organisms obtained for this study were from clinical cultures submitted to our institutional microbiology laboratory, from patients with various hematologic malignancies and solid tumors, treated between 2012 and 2013. The organisms were obtained for in vitro testing after approval of this study by the Institution Review Board (IRB). To avoid duplication, only one isolate per patient per episode of infection was tested. The majority of these isolates (>85%) were from blood culture specimens. A few were from other significant clinical sites such as cerebrospinal fluid, wounds and pleural or synovial fluid.
Susceptibility testing
Susceptibility testing was performed using the E-test methodology in accordance with CLSI guidelines (25). Appropriate control strains (S. aureus ATCC 29213 and Enterococcus faecalis ATCC 29212) were used to ensure the accuracy and validity of our results. Drug concentrations that inhibited growth of 50 and 90% of isolates (MIC50 and MIC90 values, respectively) were calcd only if ⩾10 isolates of a particular species were available for testing. When fewer than 10 isolates were available, MIC ranges were reported.
References
Klastersky, J. et al. Bacteraemia in febrile neutropenic cancer patients. Int. J. Antimicrob. Agents. 30 (Suppl 1), S51–S59 (2007).
Montassier, E., Batard, E., Gastinne, T., Potel, G. & de La Cochetiere, M. F. Recent changes in bacteremia in patients with cancer: a systematic review of epidemiology and antibiotic resistance. Eur. J. Clin. Microbiol. Infect. Dis. 32, 841–850 (2013).
Han, X. Y., Kamana, M. & Rolston, K. V. Viridans streptococci isolated by culture from blood of cancer patients: clinical and microbiologic analysis of 50 cases. J. Clin. Microbiol. 44, 160–165 (2006).
Shelburne, S. A. 3rd, Tarrand, J. & Rolston, K. V. Review of streptococcal bloodstream infections at a comprehensive cancer care center, 2000–2011. J. Infect. 66, 136–146 (2013).
Moellering, R. C. Jr. Vancomycin: a 50-year reassessment. Clin. Infect. Dis. 42 (Suppl 1), S3–S4 (2006).
Freifeld, A. G. et al. Clinical practice guideline for the use of antimicrobial agents in neutropenic patients with cancer: 2010 update by the infectious diseases society of america. Clin. Infect. Dis. 52, e56–e93 (2011).
Steinkraus, G., White, R. & Friedrich, L. Vancomycin MIC creep in non-vancomycin-intermediate Staphylococcus aureus (VISA), vancomycin-susceptible clinical methicillin-resistant S. aureus (MRSA) blood isolates from 2001-05. J. Antimicrob. Chemother. 60, 788–794 (2007).
Safdar, A. & Rolston, K. V. Vancomycin tolerance, a potential mechanism for refractory gram-positive bacteremia observational study in patients with cancer. Cancer 106, 1815–1820 (2006).
Pillai, S. K. et al. Development of reduced vancomycin susceptibility in methicillin-susceptible Staphylococcus aureus. Clin. Infect. Dis. 49, 1169–1174 (2009).
Sakoulas, G. et al. Relationship of MIC and bactericidal activity to efficacy of vancomycin for treatment of methicillin-resistant Staphylococcus aureus bacteremia. J. Clin. Microbiol. 42, 2398–2402 (2004).
CLSI.. Performance Standards for antimicrobial susceptibility testing. CLSI approved standard M100-S20, CLSI: Wayne, PA, USA, (2010).
van Hal, S. J., Lodise, T. P. & Paterson, D. L. The clinical significance of vancomycin minimum inhibitory concentration in Staphylococcus aureus infections: a systematic review and meta-analysis. Clin. Infect. Dis. 54, 755–771 (2012).
Hsu, D. I. et al. Comparison of method-specific vancomycin minimum inhibitory concentration values and their predictability for treatment outcome of meticillin-resistant Staphylococcus aureus (MRSA) infections. Int. J. Antimicrob. Agents. 32, 378–385 (2008).
Liu, C. et al. Clinical practice guidelines by the infectious diseases society of america for the treatment of methicillin-resistant Staphylococcus aureus infections in adults and children: executive summary. Clin. Infect. Dis. 52, 285–292 (2011).
Hope, R., Chaudhry, A., Adkin, R. & Livermore, D. M. In vitro activity of telavancin and comparators against selected groups of Gram-positive cocci. Int. J. Antimicrob. Agents. 41, 213–217 (2013).
Mendes, R. E., Sader, H. S., Farrell, D. J. & Jones, R. N. Worldwide appraisal and update (2010) of telavancin activity tested against a collection of Gram-positive clinical pathogens from five continents. Antimicrob. Agents. Chemother. 56, 3999–4004 (2012).
Rolston, K. V., Kapadia, M., Tarrand, J., Coyle, E. & Prince, R. A. Spectrum of gram-positive bacteraemia and in vitro activities of daptomycin, linezolid and vancomycin against organisms isolated from cancer patients. Int. J. Antimicrob. Agents. 41, 516–520 (2013).
Hughes, W. T. et al. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin. Infect. Dis. 34, 730–751 (2002).
Finberg, R. W. et al. The importance of bactericidal drugs: future directions in infectious disease. Clin. Infect. Dis. 39, 1314–1320 (2004).
Mahajan, S. N. et al. Characteristics and outcomes of methicillin-resistant staphylococcus aureus bloodstream infections in patients with cancer treated with vancomycin: 9-year experience at a comprehensive cancer center. Oncologist 17, 1329–1336 (2012).
Gu, B., Kelesidis, T., Tsiodras, S., Hindler, J. & Humphries, R. M. The emerging problem of linezolid-resistant Staphylococcus. J. Antimicrob. Chemother. 68, 4–11 (2013).
Mendes, R. E., Sader, H. S., Farrell, D. J. & Jones, R. N. Telavancin activity tested against a contemporary collection of Gram-positive pathogens from USA Hospitals (2007-2009). Diagn. Microbiol. Infect. Dis. 72, 113–117 (2012).
Mendes, R. E., Sader, H. S., Farrell, D. J. & Jones, R. N. Update on the telavancin activity tested against European staphylococcal clinical isolates (2009-2010). Diagn. Microbiol. Infect. Dis. 71, 93–97 (2011).
Klotchko, A., Wallace, M. R., Licitra, C. & Sieger, B. Staphylococcus lugdunensis: an emerging pathogen. South. Med. J. 104, 509–514 (2011).
Smith, K., Gemmell, C. G. & Lang, S. Telavancin shows superior activity to vancomycin with multidrug-resistant Staphylococcus aureus in a range of in vitro biofilm models. Eur. J. Clin. Microbiol. Infect. Dis. 32, 1327–1332 (2013).
Pankey, G. A. & Ashcraft, D. S. In Vitro Synergy of telavancin and rifampin against enterococcus faecium resistant to both linezolid and vancomycin. Ochsner J. 13, 61–65 (2013).
Stryjewski, M. E. et al. Telavancin versus vancomycin for the treatment of complicated skin and skin-structure infections caused by gram-positive organisms. Clin. Infect. Dis. 46, 1683–1693 (2008).
Rubinstein, E. et al. Telavancin versus vancomycin for hospital-acquired pneumonia due to gram-positive pathogens. Clin. Infect. Dis. 52, 31–40 (2011).
Hegde, S. S., Difuntorum, S., Skinner, R., Trumbull, J. & Krause, K. M. Efficacy of telavancin against glycopeptide-intermediate Staphylococcus aureus in the neutropenic mouse bacteraemia model. J. Antimicrob. Chemother. 63, 763–766 (2009).
Reyes, N. et al. Efficacy of telavancin in a murine model of bacteraemia induced by methicillin-resistant Staphylococcus aureus. J. Antimicrob. Chemother. 58, 462–465 (2006).
Acknowledgements
Funding for this study was provided by Theravance Incorporated.
Ethical approval
The University of Texas MD Anderson Cancer Center (Houston, Tx) Institutional review board LAB07-0690.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Rolston, K., Wang, W., Nesher, L. et al. In vitro activity of telavancin compared with vancomycin and linezolid against Gram-positive organisms isolated from cancer patients. J Antibiot 67, 505–509 (2014). https://doi.org/10.1038/ja.2014.30
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ja.2014.30
Keywords
This article is cited by
-
Antibacterial activity of recently approved antibiotics against methicillin-resistant Staphylococcus aureus (MRSA) strains: A systematic review and meta-analysis
Annals of Clinical Microbiology and Antimicrobials (2022)
-
In vitro activity of dalbavancin and five comparator agents against common and uncommon Gram-positive organisms isolated from cancer patients
The Journal of Antibiotics (2016)