Abstract
Recently, low serum uric acid (SUA) levels and high SUA levels, have emerged as risk factors for cardiovascular disease, as well as for the incidence of acute kidney injury and chronic kidney disease (CKD). However, the effect of low SUA on the progression of CKD remains unclear. To evaluate the association between SUA and renal prognosis in patients with immunoglobulin A nephropathy (IgAN), one of the most common causes of CKD, we retrospectively followed 1218 patients who were diagnosed with primary IgAN by kidney biopsy between October 1979 and December 2010. Patients were divided into three groups on the basis of SUA level tertiles: low (L group), middle (M group) and high (H group) tertiles (<6.1, 6.1–7.0, and >7.0 mg dl−1, respectively, for men and <4.4, 4.4–5.3, and >5.3 mg dl−1, respectively, for women). The risk factors for developing end-stage renal disease (ESRD) were estimated using a Cox proportional hazards model. After a median follow-up of 5.1 years, 142 patients (11.7%) developed ESRD. The hazard ratio (95% confidence interval) showed a J-shaped trend with the tertiles in both men (1.18 (0.55–2.54), 1.00 (reference), and 1.80 (1.01–3.10) in L, M and H groups, respectively) and women (2.73 (1.10–6.76), 1.00 (reference) and 2.49 (1.16–5.34) in L, M and H groups, respectively). Notably, low SUA was significantly associated with incident ESRD in women. This finding suggests that SUA has a J-shaped association with ESRD in patients with IgAN, especially women.
Similar content being viewed by others
Introduction
Immunoglobulin A nephropathy (IgAN) is the most common form of glomerulonephritis worldwide. Patients with IgAN show various clinical manifestations, including isolated hematuria, gross hematuria, nephrotic syndrome, hypertension and progressive kidney failure. The prognosis of IgAN has been reported by many investigators, and ~15–40% of patients progress to end-stage renal disease (ESRD) over 10–20 years.1, 2 The prognostic factors that have been reported include proteinuria, decreased estimated glomerular filtration rate (eGFR) at diagnosis, hypertension and pathological severity, and several risk prediction models have been proposed and validated.3, 4, 5
A high serum uric acid (SUA) level is known to be an important risk factor in several clinical settings, such as hypertension,6 metabolic syndrome,7 cardiovascular disease,8, 9 new-onset kidney disease10 and the progression of chronic kidney disease (CKD).11 Another recent study has suggested that high SUA levels and concurrent metabolic acidosis might be associated with all-cause mortality in the general population.12 With regard to patients with IgAN, there are also several studies demonstrating that high SUA is an independent risk factor for ESRD.13, 14, 15 In those studies, tubulointerstitial injuries, vascular injuries and glomerulosclerosis have been proposed as possible mechanisms of kidney dysfunction caused by high SUA.13, 14, 15 In addition, in previous experimental studies, uric acid has been found to stimulate vascular smooth muscle cell proliferation by activating mitogen-activated protein kinases and stimulating cyclooxygenase-2 and platelet-derived growth factor synthesis, which may lead to the progression of atherosclerosis and CKD.16
In contrast, some studies have reported that low SUA, in addition to high SUA, may be a risk factor for cardiovascular mortality in the general population, CKD patients and hemodialysis patients.17, 18, 19 In those studies, the free radical scavenging effects of SUA and the association between lower SUA levels and lower antioxidant capacities have been discussed.17, 18, 19 Recently, a possible association between low SUA and acute/chronic kidney dysfunction has also been reported.20, 21 Kanda et al.20 have demonstrated the unfavorable effect of low SUA on kidney function decline in the general population, and Otomo et al.21 have reported the development of acute kidney injury in both male and female hospitalized patients. However, the association between low SUA and the progression of IgAN has not been investigated to date. In this study, we evaluated the association between SUA and the development of ESRD in patients with IgAN by using a large-scale retrospective cohort.
Methods
Study design and population
This study was a retrospective cohort study using the IgAN data set from 7 institutions (Kyushu University Hospital, Japanese Red Cross Fukuoka Hospital, Hamanomachi Hospital, Munakata Medical Association Hospital, Japan Seafarers Relief Association Moji Ekisaikai Hospital, Japanese Red Cross Karatsu Hospital and Hakujyuji Hospital). A total of 1640 patients were diagnosed with primary IgAN by percutaneous kidney biopsy between October 1979 and December 2010. Henoch–Schönlein purpura nephritis, lupus nephritis and glomerulonephritis associated with liver diseases were not included in this study. We also excluded 177 patients whose biopsy specimens contained fewer than 10 glomeruli and 245 patients without available clinical measurements. Therefore, a total of 1218 patients were enrolled. This study was performed in accordance with the principles of the Declaration of Helsinki and with the approval of the Clinical Research Ethics Committee of the Kyushu University Hospital Institutional Review Board (approval ID 469-04). The ethics committees of all participating institutions granted approval to waive the requirement for written, informed consent because of the retrospective nature of the present study.
Kidney biopsy and pathological evaluations
Percutaneous kidney biopsy was performed under ultrasound guidance with an 18-gauge needle in all patients. For light microscopic observations, tissue sections were cut at a thickness of 2 μm and stained with hematoxylin and eosin, periodic acid Schiff, periodic acid methenamine silver and Masson’s trichrome stains. In immunofluorescence studies, we examined the specimens for IgG, IgA, IgM, complement (C) 3, C1q, fibrinogen and kappa/lambda light chains.
Pathological lesions were evaluated according to the Oxford classification system,22 and extracapillary proliferation was evaluated according to a previous report.23 The mesangial hypercellularity score (M) was defined as M0 if the score was <0.5 and as M1 if the score was ⩾0.5; endocapillary hypercellularity (E), segmental glomerulosclerosis (S) and extracapillary proliferation (Ex) were expressed as E0, S0 and Ex (0), respectively, if absent and as E1, S1 and Ex1 if present. Segmental glomerulosclerosis and tuft adhesions were analyzed together. Ex included both cellular and fibrocellular crescents. Tubular atrophy/interstitial fibrosis (T) was semi-quantitatively classified according to the percentage of the lesions in cortical area: T0 for 0–25%, T1 for 26–50%, and T2 for >50%.
Clinical parameters
Baseline clinical data were obtained from the medical records at the time of renal biopsy and included age, sex, body mass index (BMI), blood pressure, SUA, serum albumin, total cholesterol, triglycerides, serum creatinine and 24-h urinary protein excretion or urinary protein-to-creatinine ratio. Diabetes mellitus was defined as previously diagnosed or by the use of hypoglycemic agents. SUA, albumin, total cholesterol levels and triglycerides were determined enzymatically. Serum creatinine was measured by the Jaffe method until April 1988, and by the enzymatic method from May 1988 onward, at Kyushu University. At the other participating institutions, serum creatinine was measured by the Jaffe method until December 2000 and by the enzymatic method from January 2001. Serum creatinine values measured by the Jaffe method were converted to values for the enzymatic method by subtracting 0.207 mg dl−1. The eGFR in patients aged 18 years or older was calculated by using the following formula: eGFR (ml min−1 1.73 m−2)=194 × serum creatinine−1.094 × age−0.287 × 0.739 (if female).24 For patients younger than 18 years, we used the Schwartz formula for the calculation of eGFR.25, 26
Renal outcome
The primary end point was ESRD, which was defined as the initiation of renal replacement therapy; hemodialysis, peritoneal dialysis or kidney transplantation. The renal outcomes were derived from medical records or by telephone consultation with the clinics and hospitals or with the patients themselves, as described in our previous studies.4, 27
Statistical analyses
Data are presented as the mean and s.d., the median and interquartile range, or the percentage for categorical measures in patients, as appropriate. The studied patients were divided into three groups on the basis of SUA level tertiles; L group (low SUA), SUA <6.1 mg dl−1 for men and <4.4 mg dl−1 for women; M group (middle SUA), SUA 6.1–7.0 mg dl−1 for men and 4.4–5.3 mg dl−1 for women; and H group (high SUA), SUA >7.0 mg dl−1 for men and >5.3 mg dl−1 for women. To evaluate the relationship between low/high SUA and the risk of ESRD, we performed post hoc analyses using the Dunnett–Hsu test or χ2 test and M as a reference. The risk of progression to ESRD according to SUA levels was depicted by the Kaplan–Meier method and compared using a log-rank test. The hazard ratios (HRs) and 95% confidence intervals (CIs) of the progression of ESRD in three groups were estimated with a multivariable Cox proportional hazards model with backward selection. All statistical analyses were conducted using SAS software, version 9.2 (SAS Institute, Inc., Cary, NC, USA). A two-tailed P-value <0.05 was considered to be statistically significant in all analyses.
Results
Baseline characteristics of the studied patients according to SUA levels
The basic characteristics of the studied patients overall and for each sex are summarized in Table 1. The median age was 35 years (range, 23–47 years), the proportion of men was 45.0%, the urinary protein excretion was 0.8 (0.3–1.8) g per day, the eGFR was 78±31 ml min−1 1.73 m−2, the systolic blood pressure was 126.5±18.7 mm Hg, the diastolic blood pressure was 75.7±13.7 mm Hg, the serum creatinine level was 1.0±0.6 mg dl−1 and the SUA level was 5.8±1.6 mg dl−1. Thirty-four patients (2.8%) had type 2 diabetes, 288 (23.6%) were taking anti-hypertensive drugs, 11 (0.9%) were taking diuretics, and 28 (2.3%) were taking allopurinol at the time of renal biopsy.
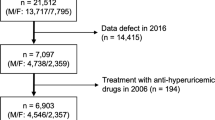
The distribution of baseline SUA level was different between sexes, and SUA levels were 6.7±1.4 mg dl−1 in men and 5.1±1.3 mg dl−1 in women (Figure 1). Therefore, we analyzed the relationship between SUA and renal outcome in each sex separately. The clinical and histopathological characteristics of the three groups according to SUA levels in each sex are shown in Table 2. Patients in the H group were older than those in the M group and had significantly higher BMI, systolic blood pressure, total cholesterol, triglycerides, urinary protein excretion and significantly lower serum albumin and eGFR levels, in both men and women. In contrast, the patients in the L group had significantly lower total serum cholesterol and triglyceride levels, and significantly higher eGFR than those in the M group in both sexes. Under the Oxford classification, the percentage of patients with M1 and T scores were significantly higher in the H group than in the M group in women. The percentage of patients with M1 was significantly lower in the L group in women, and the percentage of patients with E1 was significantly lower in the L group in men. With regard to the treatment, a renin-angiotensin system blocker was more commonly used in the H group in female patients. The other parameters did not show any differences among the three groups in both sexes.
Some parameters showed a sex difference. Between male and female patients, we found differences in BMI (22.6 kg m−2 vs. 21.7 kg m−2, P<0.05), incidence of hypertension (27.0% vs. 20.9%, P<0.05), and triglyceride level (150.7±107.5 mg dl−1 vs. 108.1±67.2 mg dl−1, P<0.05).
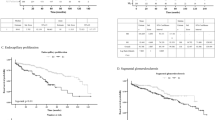
Crude analysis of renal survival in relation to SUA levels
During the follow-up period of a median of 5.1 years, 142 out of 1218 patients (11.7%) developed ESRD. Figure 2 indicates the unadjusted Kaplan–Meier estimates for renal survival in relation to SUA levels in each sex. In male patients, renal survival was lowest in the H group, and the survival in the M group was slightly lower than that in the L group. In women, renal survival in the H group was significantly lower than in the L and M groups; however, the patients in the L group showed lower renal survival than the M group, and 12 patients in the female L group developed ESRD. In the female L group, the actual patient numbers and rates of ESRD according to more detailed SUA levels were as follows: 0/0 in SUA <2.0, 0/13 in SUA ⩾2.0 and <3.0, 6/113 (5.3%) in SUA ⩾3.0 and <4.0 and 6/90 (6.7%) in SUA 4.0–4.4 mg dl−1. Although the survival analysis between L and M in women was not significantly different, as determined by unadjusted analysis (log-rank test, P=0.36), the results indicate that there might be a ‘J-shaped’ association between SUA levels and renal outcome in female patients with IgAN.
Multivariable analysis to identify the association between SUA levels and the development of end-stage renal disease in men and women
In a multivariable proportional hazards Cox regression with a backward selection procedure (P<0.1), age, sex, hypertension, BMI, urinary protein excretion, eGFR, serum albumin, diabetes mellitus, diuretic use, allopurinol use and M, S, and T scores in the Oxford classification were selected as factors.
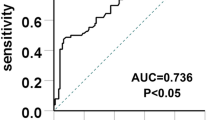
We calculated the HRs for the progression of ESRD with 95% CIs by using a clinical confounding factors adjusted model (model 1), and a model adjusted for both clinical and pathological confounders (model 2) for the L group and H group vs. the M group (Table 3). In the age- and sex-adjusted model, model 1, and model 2, the patients in the H group revealed a significantly higher risk for the development of ESRD compared with those with M group in overall, male and female patients. With regard to the comparison between the L group and M group, the patients in the L group showed a 1.67-fold (95% CI 0.93–3.00) higher risk for ESRD than those in the M group in model 2, but this effect did not reach statistical significance (P=0.08) in the overall analysis. In the sub-analysis with male patients, the effect of low SUA on ESRD was not evident in all three models, a result similar to the crude analysis shown in Figure 2; however, the female patients in the L group showed a 2.73-fold (95% CI 1.10–6.76) risk in model 1 (P=0.03), and a 3.11-fold (1.24–7.85) risk in model 2 (P=0.02), as compared with the M group. As shown in Figure 3, SUA levels and the HRs for the development of ESRD showed a U-shaped trend in female patients, but not in male patients.
We additionally performed sensitivity analyses. First, multivariable analysis after excluding 28 patients with allopurinol use revealed that male patients in the H group showed a 1.31-fold (95% CI 0.74–2.43) higher risk for ESRD than those in the M group in model 1 and a 1.32-fold (95% CI 0.73–2.50) higher risk in model 2, although this trend did not reach statistical significance (P=0.35 and 0.37, respectively). In contrast, in female patients, the association between low SUA and the development of ESRD remained significant (model 2 analysis; HR 3.09, 95% CI 1.23–7.79, P=0.02). We performed an additional analysis including serum total cholesterol and triglycerides as covariates. In these analyses, male patients in the H group showed a 1.59-fold (95% CI 0.87–2.90) higher risk for ESRD than those in the M group in model 1, and a 1.84-fold (95% CI 0.96–3.51) higher risk in model 2, although this result was again not statistically significant (P=0.13 and 0.06, respectively). In the female H group, the association was also weakened, and the HR was 2.14 (95% CI 0.98–4.65, P=0.06). The association between low SUA and the development of ESRD remained significant in model 2 (HR 3.11, 95% CI 1.23–7.85, P=0.02).
Discussion
In this study, we investigated the effect of the SUA level at kidney biopsy on the clinical course of IgAN by using a large retrospective cohort. We demonstrated that not only high SUA but also low SUA is a significant risk factor for the development of ESRD in patients overall and especially in female patients. Although the clinical effect of high SUA has already been studied in IgAN,13, 14, 15 previous studies have compared only high versus normal SUA and have not commented on low SUA levels.
Recent observational studies have demonstrated a J-shaped trend between SUA and the development of cardiovascular diseases in the general population17 and in patients with essential hypertension,8 type 2 diabetes,9 CKD18 and under hemodialysis.19 With regard to the association between low SUA and kidney function, Kanda et al.20 have demonstrated a similar association between SUA and decreases in kidney function in healthy subjects in their large-scale prospective study. Otomo et al.21 have retrospectively investigated 81 770 hospitalized patients and have demonstrated a higher odds ratio of acute kidney injury incidence in patients with both high and low SUA levels. In that study, the adjusted odds ratio of acute kidney injury were found to be significantly increased in patients with SUA ⩽3.0 mg dl−1 for women and ⩽4.5 mg dl−1 for men. These studies suggest that SUA plays a bidirectional role and that low SUA and high SUA might be associated with unfavorable outcomes in kidney function.
Although the pathogenesis of the effects of low SUA on cardiovascular diseases and kidney dysfunction have not been demonstrated in detail, several possible mechanisms have been proposed. Low SUA might be associated with poor protein intake and malnutrition, decreased daily intake of purines or nucleotides, which are essential nutrients, and a deficit in antioxidant capacity, because uric acid has important antioxidant properties.18, 19 Other possible explanations are that hypouricemia is associated with diabetes.28 Because the prevalence of diabetes and eGFR levels tended to be higher in the female L group, glomerular hyperfiltration might promote the progression of CKD. In addition, some patients might have renal hypouricemia that can cause recurrent acute kidney injury with severe loin pain after anaerobic exercise and can cause the development of CKD.20 Our study population included many young patients who were unlikely to have malnutrition, and we performed a multivariable proportional hazards Cox regression to exclude the effects of malnutrition and diabetes. Although we could not exclude the possibility of some genetic abnormalities that might have caused renal hypouricemia, those conditions are not common, and we speculate the most important mechanism is an inadequate protection against oxidative stress.
Several experimental studies have supported the hypothesis that uric acid has an antioxidant function. In aerobic cells, free radicals are constantly produced mostly as reactive oxygen species. Once they are produced, free radicals are removed by antioxidant defenses including the enzymes catalase, glutathione peroxidase and superoxide dismutase (SOD). SOD1 and SOD3 are inactivated by H2O2, but this inactivation is prevented by uric acid in a dose-dependent manner.29 Therefore, baseline physiological levels of uric acid are required to prevent the inactivation of SOD1 and SOD3 by H2O2. With regard to in vivo studies, Spitsin et al.30 have investigated the effect of uric acid on experimental allergic encephalomyelitis and have demonstrated that uric acid significantly improves the clinical score, inflammation, and the expression of inducible NO synthase and nitrotyrosine. In their study, the protective effect of uric acid has been found to be associated with its ability to neutralize the oxidative properties of ONOO−. Haberman et al.31 have also investigated the therapeutic potential for soluble analogs of uric acid in the experimental model of stroke and related neurodegenerative conditions. In their study, 1,7-dimethyluric acid (mUA2) and 6,8-dithiouric acid (sUA2) were administered to mice with transient or permanent ischemia, and uric acid analogs attenuated damage of the brain and exhibited neuroprotective activity.
The association between oxidative stress and the progression of kidney disease has been studied using various experimental models32, 33, and the important role of advanced oxidation protein products (AOPPs), a family of oxidized, dityrosine-containing protein-insoluble products generated by oxidative stress, has been emphasized.34, 35 Intravenous administration of AOPP-modified rat serum albumin has been found to accelerate proteinuria, renal fibrosis and renal dysfunction in 5/6 nephrectomized rats, thus suggesting that the accumulation of AOPP promotes renal fibrosis, probably via a redox-sensitive inflammatory pathway.34 Zhou et al. have demonstrated that intravenous injection of AOPP-modified albumin induces podocyte apoptosis and proteinuria in normal rats. They have also shown that AOPPs trigger apoptosis of cultured podocytes by NADPH oxidase-dependent O2− generation.35 With regard to the clinical studies, Latscha et al. have reported that elevated plasma AOPPs at the early stages of disease are a significant prognostic factor in patients with IgAN.36 Another study has shown that AOPPs significantly correlate with serum IgA1 with galactose-deficient hinge-region O-glycans, which is thought to be a key player in the development of IgAN.37
The second important finding in the present study is that the J-shaped trend was more clearly observed in women than in men (Figure 3). Notably, in female patients, the association between low SUA and ESRD remained significant even in the sensitivity analyses excluding the effect of allopurinol and including serum cholesterol and triglycerides as covariables. Only a few studies have analyzed the effect of low SUA in both sexes separately. Kanda et al.20 and Otomo et al.21 have demonstrated the unfavorable effect of low SUA on kidney function decline in the general population and the development of acute kidney injury in both male and female hospitalized patients, results that conflict with our results. However, the baseline SUA levels in our study and Kanda et al.20 and Otomo et al.21 were different, and our study population showed higher baseline SUA levels because all subjects were CKD patients with IgAN. In our study, the analyses using the tertiles of SUA level revealed that the low SUA group in men had SUA levels <6.1 mg dl−1, which included many normouricemic patients. Thus, the most likely explanation of the sex difference in the present study is that there were an extremely small number of male patients with an absolutely low SUA level. Another possible explanation is that male IgAN patients are more likely to have risk factors for ESRD, including smoking, obesity, hypertension, dyslipidemia and non-adherence. In the present study, we found differences in BMI, incidence of hypertension and triglyceride levels between male and female patients. Therefore, we speculate that the effect of low SUA on the progression of IgAN was weakened in male patients by other risk factors.
Several limitations in this study should be noted. First, this was a retrospective study. Therefore, we were unable to adjust for unmeasured confounding factors. For example, genetic background should be considered because some individuals show familial renal hypouricemia characterized by extraordinarily high renal uric acid clearance and low SUA.38 Second, a single measurement of SUA at the time of diagnosis was used for the analyses, and this measurement might have failed to capture the intra-individual variability over time, and thus may have caused the misclassification of some patients into different SUA level categories. Third, we were unable to determine the optimal SUA levels for protection from oxidative stress, as in other clinical studies. Detailed analysis in the female L group revealed no difference in the rates of ESRD at SUA levels of 3.0–4.0 and 4.0–4.4 mg dl−1, and no ESRD was found in 3.0 mg dl−1 or less. Further investigations with large sample sizes including patients with extremely low SUA are necessary.
In conclusion, not only high but also low SUA levels may be independent risk factors for the progression of IgAN, and these associations are more likely to be observed in women. Further investigations are required, especially large-scale, prospective studies with long-term observations, to confirm the association between SUA and kidney dysfunction in CKD, including IgAN.
References
Barratt J, Feehally J . IgA nephropathy. J Am Soc Nephrol 2005; 16: 2088–2097.
D'Amico G . Natural history of idiopathic IgA nephropathy: role of clinical and histological prognostic factors. Am J Kidney Dis 2000; 36: 227–237.
Goto M, Wakai K, Kawamura T, Ando M, Endoh M, Tomino Y . A scoring system to predict renal outcome in IgA nephropathy: a nationwide 10-year prospective cohort study. Nephrol Dial Transplant 2009; 24: 3068–3074.
Tanaka S, Ninomiya T, Katafuchi R, Masutani K, Tsuchimoto A, Noguchi H, Hirakata H, Tsuruya K, Kitazono T . Development and validation of a prediction rule using the Oxford classification in IgA nephropathy. Clin J Am Soc Nephrol 2013; 8: 2082–2090.
Nagayama Y, Nishiwaki H, Hasegawa T, Komukai D, Kawashima E, Takayasu M, Tayama H, Inoue Y, Inui K, Yoshimura A . Impact of the new risk stratification in the 2011 Japanese Society of Nephrology clinical guidelines for IgA nephropathy on incidence of early clinical remission with tonsillectomy plus steroid pulse therapy. Clin Exp Nephrol 2014; 19: 646–652.
Krishnan E, Kwoh CK, Schumacher HR, Kuller L . Hyperuricemia and incidence of hypertension among men without metabolic syndrome. Hypertension 2007; 49: 298–303.
Nagahama K, Inoue T, Kohagura K, Kinjo K, Ohya Y . Associations between serum uric acid levels and the incidence of hypertension and metabolic syndrome: a 4-year follow-up study of a large screened cohort in Okinawa, Japan. Hypertens Res 2015; 38: 213–218.
Verdecchia P, Schillaci G, Reboldi G, Santeusanio F, Porcellati C, Brunetti P . Relation between serum uric acid and risk of cardiovascular disease in essential hypertension. The PIUMA study. Hypertension 2000; 36: 1072–1078.
Mazza A, Zamboni S, Rizzato E, Pessina AC, Tikhonoff V, Schiavon L, Casiglia E . Serum uric acid shows a J-shaped trend with coronary mortality in non-insulin-dependent diabetic elderly people. The CArdiovascular STudy in the ELderly (CASTEL). Acta Diabetol 2007; 44: 99–105.
Kamei K, Konta T, Hirayama A, Suzuki K, Ichikawa K, Fujimoto S, Iseki K, Moriyama T, Yamagata K, Tsuruya K, Kimura K, Narita I, Kondo M, Asahi K, Watanabe T . A slight increase within the normal range of serum uric acid and the decline in renal function: associations in a community-based population. Nephrol Dial Transplant 2014; 29: 2286–2292.
Obermayr RP, Temml C, Gutjahr G, Knechtelsdorfer M, Oberbauer R, Klauser-Braun R . Elevated uric acid increases the risk for kidney disease. J Am Soc Nephrol 2008; 19: 2407–2413.
Park M, Jung SJ, Yoon S, Yun JM, Yoon HJ . Association between the markers of metabolic acid load and higher all-cause and cardiovascular mortality in a general population with preserved renal function. Hypertens Res 2015; 38: 433–438.
Syrjanen J, Mustonen J, Pasternack A . Hypertriglyceridaemia and hyperuricaemia are risk factors for progression of IgA nephropathy. Nephrol Dial Transplant 2000; 15: 34–42.
Ohno I, Hosoya T, Gomi H, Ichida K, Okabe H, Hikita M . Serum uric acid and renal prognosis in patients with IgA nephropathy. Nephron 2001; 87: 333–339.
Cheng GY, Liu DW, Zhang N, Tang L, Zhao ZZ, Liu ZS . Clinical and prognostic implications of serum uric acid levels on IgA nephropathy: a cohort study of 348 cases with a mean 5-year follow-up. Clin Nephrol 2013; 80: 40–46.
Kang DH, Han L, Ouyang X, Kahn AM, Kanellis J, Li P, Feng L, Nakagawa T, Watanabe S, Hosoyamada M, Endou H, Lipkowitz M, Abramson R, Mu W, Johnson RJ . Uric acid causes vascular smooth muscle cell proliferation by entering cells via a functional urate transporter. Am J Nephrol 2005; 25: 425–433.
Culleton BF, Larson MG, Kannel WB, Levy D . Serum uric acid and risk for cardiovascular disease and death: the Framingham Heart Study. Ann Intern Med 1999; 131: 7–13.
Suliman ME, Johnson RJ, Garcia-Lopez E, Qureshi AR, Molinaei H, Carrero JJ, Heimburger O, Barany P, Axelsson J, Lindholm B, Stenvinkel P . J-shaped mortality relationship for uric acid in CKD. Am J Kidney Dis 2006; 48: 761–771.
Hsu SP, Pai MF, Peng YS, Chiang CK, Ho TI, Hung KY . Serum uric acid levels show a 'J-shaped' association with all-cause mortality in haemodialysis patients. Nephrol Dial Transplant 2004; 19: 457–462.
Kanda E, Muneyuki T, Kanno Y, Suwa K, Nakajima K . Uric acid level has a U-shaped association with loss of kidney function in healthy people: a prospective cohort study. PLoS ONE 2015; 10: e0118031.
Otomo K, Horino T, Miki T, Kataoka H, Hatakeyama Y, Matsumoto T, Hamada-Ode K, Shimamura Y, Ogata K, Inoue K, Taniguchi Y, Terada Y, Okuhara Y . Serum uric acid level as a risk factor for acute kidney injury in hospitalized patients: a retrospective database analysis using the integrated medical information system at Kochi Medical School hospital. Clin Exp Nephrol 2016; 20: 235–243.
Roberts IS, Cook HT, Troyanov S, Alpers CE, Amore A, Barratt J, Berthoux F, Bonsib S, Bruijn JA, Cattran DC, Coppo R, D'Agati V, D'Amico G, Emancipator S, Emma F, Feehally J, Ferrario F, Fervenza FC, Florquin S, Fogo A, Geddes CC, Groene HJ, Haas M, Herzenberg AM, Hill PA, Hogg RJ, Hsu SI, Jennette JC, Joh K, Julian BA, Kawamura T, Lai FM, Li LS, Li PK, Liu ZH, Mackinnon B, Mezzano S, Schena FP, Tomino Y, Walker PD, Wang H, Weening JJ, Yoshikawa N, Zhang H . The Oxford classification of IgA nephropathy: pathology definitions, correlations, and reproducibility. Kidney Int 2009; 76: 546–556.
Katafuchi R, Ninomiya T, Nagata M, Mitsuiki K, Hirakata H . Validation study of oxford classification of IgA nephropathy: the significance of extracapillary proliferation. Clin J Am Soc Nephrol 2011; 6: 2806–2813.
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A . Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 2009; 53: 982–992.
Schwartz GJ, Haycock GB, Edelmann CM Jr, Spitzer A . A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics 1976; 58: 259–263.
Schwartz GJ, Brion LP, Spitzer A . The use of plasma creatinine concentration for estimating glomerular filtration rate in infants, children, and adolescents. Pediatr Clin North Am 1987; 34: 571–590.
Tanaka S, Ninomiya T, Masutani K, Nagata M, Tsuchimoto A, Tsuruya K, Kitazono T . Prognostic impact of serum bilirubin level on long-term renal survival in IgA nephropathy. Clin Exp Nephrol 2015; 19: 1062–1070.
Bo S, Cavallo-Perin P, Gentile L, Repetti E, Pagano G . Hypouricemia and hyperuricemia in type 2 diabetes: two different phenotypes. Eur J Clin Invest 2001; 31: 318–321.
Hink HU, Santanam N, Dikalov S, McCann L, Nguyen AD, Parthasarathy S, Harrison DG, Fukai T . Peroxidase properties of extracellular superoxide dismutase: role of uric acid in modulating in vivo activity. Arterioscler Thromb Vasc Biol 2002; 22: 1402–1408.
Spitsin SV, Scott GS, Mikheeva T, Zborek A, Kean RB, Brimer CM, Koprowski H, Hooper DC . Comparison of uric acid and ascorbic acid in protection against EAE. Free Radic Biol Med 2002; 33: 1363–1371.
Haberman F, Tang SC, Arumugam TV, Hyun DH, Yu QS, Cutler RG, Guo Z, Holloway HW, Greig NH, Mattson MP . Soluble neuroprotective antioxidant uric acid analogs ameliorate ischemic brain injury in mice. Neuromolecular Med 2007; 9: 315–323.
Budisavljevic MN, Hodge L, Barber K, Fulmer JR, Durazo-Arvizu RA, Self SE, Kuhlmann M, Raymond JR, Greene EL . Oxidative stress in the pathogenesis of experimental mesangial proliferative glomerulonephritis. Am J Physiol Renal Physiol 2003; 285: 1138–1148.
Shah SV, Baliga R, Rajapurkar M, Fonseca VA . Oxidants in chronic kidney disease. J Am Soc Nephrol 2007; 18: 16–28.
Li HY, Hou FF, Zhang X, Chen PY, Liu SX, Feng JX, Liu ZQ, Shan YX, Wang GB, Zhou ZM, Tian JW, Xie D . Advanced oxidation protein products accelerate renal fibrosis in a remnant kidney model. J Am Soc Nephrol 2007; 18: 528–538.
Zhou LL, Hou FF, Wang GB, Yang F, Xie D, Wang YP, Tian JW . Accumulation of advanced oxidation protein products induces podocyte apoptosis and deletion through NADPH-dependent mechanisms. Kidney Int 2009; 76: 1148–1160.
Descamps-Latscha B, Witko-Sarsat V, Nguyen-Khoa T, Nguyen AT, Gausson V, Mothu N, Cardoso C, Noel LH, Guerin AP, London GM, Jungers P . Early prediction of IgA nephropathy progression: proteinuria and AOPP are strong prognostic markers. Kidney Int 2004; 66: 1606–1612.
Camilla R, Suzuki H, Dapra V, Loiacono E, Peruzzi L, Amore A, Ghiggeri GM, Mazzucco G, Scolari F, Gharavi AG, Appel GB, Troyanov S, Novak J, Julian BA, Coppo R . Oxidative stress and galactose-deficient IgA1 as markers of progression in IgA nephropathy. Clin J Am Soc Nephrol 2011; 6: 1903–1911.
Kaito H, Ishimori S, Nozu K, Shima Y, Nakanishi K, Yoshikawa N, Iijima K . Molecular background of urate transporter genes in patients with exercise-induced acute kidney injury. Am J Nephrol 2013; 38: 316–320.
Acknowledgements
We thank Drs. Tetsuhiko Yoshida (Hamanomachi Hospital), Kei Hori (Munakata Medical Association Hospital), Takashi Inenaga (Japan Seafarers Relief Association Moji Ekisaikai Hospital), Akinori Nagashima (Japanese Red Cross Karatsu Hospital) and Tadashi Hirano (Hakujyuji Hospital) for patient recruitment, treatment and follow-up. We also thank Ms. Hideko Noguchi for her excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Matsukuma, Y., Masutani, K., Tanaka, S. et al. A J-shaped association between serum uric acid levels and poor renal survival in female patients with IgA nephropathy. Hypertens Res 40, 291–297 (2017). https://doi.org/10.1038/hr.2016.134
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.134
Keywords
This article is cited by
-
Serum uric acid level is associated with an increase in systolic blood pressure over time in female subjects: Linear mixed-effects model analyses
Hypertension Research (2022)
-
An evaluation of the roles of hematuria and uric acid in defining the prognosis of patients with IgA nephropathy
Pediatric Nephrology (2022)
-
U-shaped relationship between serum uric acid level and decline in renal function during a 10-year period in female subjects: BOREAS-CKD2
Hypertension Research (2021)
-
Sex disparities in IgA nephropathy: a retrospective study in Chinese patients
International Urology and Nephrology (2021)
-
Association between serum uric acid and new onset and progression of chronic kidney disease in a Japanese general population: Iki epidemiological study of atherosclerosis and chronic kidney disease
Clinical and Experimental Nephrology (2021)