Abstract
Measurement of carotid-femoral pulse wave velocity (cfPWV) is considered the gold standard for assessing arterial stiffness. Although widely used in clinical and observational studies, the detection of cfPWV has not yet been applied in everyday clinical practice due to technical and procedural difficulties. We, therefore, evaluated the applicability of oscillometric cfPWV assessment for everyday clinical practice. Eighty-nine patients were prospectively included in the study. Oscillometric calculations of cfPWV were performed with Tel-O-GRAPH and tonometric calculations with Sphygmocor. The accuracy, reproducibility, reliability and robustness of Tel-O-GRAPH calculations in different clinical situations were evalu??ated. The mean study population age was 48.8±19.1 years. More than half (59.6%) of the patients were male, and 15.1% were smokers. The mean difference of PWV between devices was 0.49±1.26 m s−1 (P<0.0001), and the Pearson correlation index was 0.86 (P<0.0001). The coefficient of variation and intraclass correlation coefficients between three single measured PWV values with the Tel-O-GRAPH and Sphygmocor were 2.38±6.13% vs. 6.3±4.33% (P<0.05) and 0.99; 0.99; and 0.99 vs. 0.78; 0.84; and 0.71, respectively. For Tel-O-GRAPH, there was no statistically significant difference between PWV in seated vs. supine positions or by experienced or inexperienced users. High reproducibility and reliability of the calculated single PWV values with Tel-O-GRAPH and considerable performance accuracy compared with Sphygmocor were observed. The reported evidence suggests that oscillometry might evolve as a favored method for the assessment of the PWV in everyday clinical practice and in clinical studies due to its ease of use, accuracy and robustness.
Similar content being viewed by others
Introduction
For more than a century assessment of arterial stiffness (AS) has been a matter of scientific interest. AS reflects the elastic properties of the arterial wall, which influence the manner in which the pulse pressure and blood flow move to and return from the periphery, as well as changes of the arterial wall with each heartbeat. Thus, AS knowledge sheds light on the current status of the arteries and the cardiovascular system. Initially, the assessment of AS could only be performed invasively. Factors such as age, gender, blood pressure, heart rate, diabetes mellitus, chronic kidney disease and particular medicaments significantly influence AS.1, 2, 3 Emerging technologies enable the non-invasive evaluation of AS and have led to the incorporation of this hemodynamic feature in a variety of devices. Many studies have been performed to study AS in different populations. Currently, a reasonable amount of evidence supports the additional predictive value of AS for cardiovascular morbidity and mortality beyond standard cardiovascular risk factors.4, 5, 6 The 2013 European Guidelines for the management of arterial hypertension mentioned AS as a relevant independent risk parameter for the development of cardiovascular events.7 It is now recommended to determine AS by the non-invasive measurement of carotid-femoral pulse wave velocity (cfPWV), which can be performed with several technologies such as tonometry, ultrasonography, MRI-based techniques or cuff-based oscillometry.8 Of the first three technologies, tonometry, in particular, has been extensively used.9, 10, 11 However, all of the above-mentioned technologies require sophisticated equipment, trained personnel, repeated measurements, additional time and predefined positions of the patient, limiting their use in clinical studies. In contrast, oscillometry-based devices are able to calculate the cfPWV during normal brachial blood pressure measurement and could, thus, be suitable for use in everyday clinical practice. However, to our knowledge, there is currently no study addressing the feasibility of the measurement of oscillometric cfPWV in everyday clinical practice. Hence, in this study, we investigated this topic using a new device, the Tel-O-GRAPH(TG) (I.E.M., Stolberg, Germany).
Methods
Study population
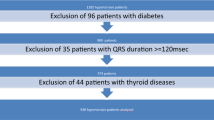
All participants were prospectively included in the study from the outpatient unit of the Department of Nephrology, Charité University, Berlin, Germany. The local ethics committee approved the protocol, and written informed consent was obtained from all subjects. The absence of sinus rhythm, the presence of multiple extrasystoles causing significant arrhythmia, significant arterial stenosis, pregnancy, an impalpable arterial pulse at the site of measurement and age <18 years were the exclusion criteria. For each subject, age, sex, height, weight and body mass index were recorded. Brachial blood pressure and heart rate were recorded with TG, which was validated according to the British Society of Hypertension protocol and showed excellent measurement accuracy for brachial blood pressure.12
Recordings with the study and reference devices
The validation measurements were performed in a warm and quiet room (21–24 °C) on study subjects in a relaxed supine position after 15 min of rest. For measurement with Sphygmocor (SC) (AtCor Medical, West Ryde, NSW, Australia), the left carotid and femoral pulses were palpated and marked appropriately. Using applanation tonometry with SC by experienced users, pulse waveforms were recorded sequentially for the left common carotid and left femoral artery. The time delay was calculated using the transit time between the two arterial sites in relation to the R-wave of the ECG. The ascending part of the pressure waveform was used as a reference point using the intersecting tangent algorithm. A single recording was deemed acceptable if the s.d. of the PWV was ⩽0.5 m s−1. The distance was calculated by subtracting the suprasternal notch to carotid site distance from the suprasternal notch to the femoral site distance.
The TG device used in the study was kindly provided by the firm I.E.M. The oscillometric measurements were performed with TG on the left upper arm. The circumference of the arm was measured, and an appropriate cuff was chosen from two available cuff sizes (24–34 cm and 32–42 cm). After obtaining the brachial blood pressure, the cuff was again inflated to maintain diastolic pressure level for 10 s for the assessment of the pulse waveform.13 The computed PWV values were recorded. The mathematic method for computing PWV implemented in TG is the algorithm used in the ARCSolver.14 Using a high-fidelity pressure sensor, the brachial pressure waveform can be recorded with the oscillometric approach. Using generalized transfer functions (Fourier analysis and de-compensation into wave harmonics), the aortic pressure waveform can be then modulated. The central flow curve can be calculated by an adopted, multi-dimensional Windkessel model. The time-lag between the pressure and flow curves is generally referred to as ‘characteristic impedance (Zc)’, in which the flow curve follows the pressure curve. Zc, together with input variables, including brachial systolic and diastolic blood pressure and age, allows the TG to estimate aortic PWV.15
The validation procedure and the assessment of cfPWV variation
In the first part of the study, we validated the oscillometric cfPWV calculation obtained by TG against that obtained by SC. Eighty-nine subjects were included. For every patient, three valid recordings of the cfPWV with TG and SC were included in the analysis. The validation procedure was performed according to the ARTERY Society guidelines for the validation of non-invasive hemodynamic measurement devices.16 For the evaluation of the cfPWV calculation robustness with TG and SC, variation and intraclass correlation coefficients (ICC) for single cfPWV values obtained with TG and SC were determined.
TG performance in supine and seated positions
In the second part of the study, we evaluated the reliability of the calculated cfPWV values obtained in the supine and seated positions. Fifteen patients were included. The measurement procedure was started in the supine position after 15 min of rest. The subject was then asked to sit up, and recordings were performed in the seated position. The cfPWV values were included in the analysis only if the mean arterial pressure (MAP) between the single recordings in supine and seated positions was stable, whereby MAP was accepted as stable within a wide range of variation (<15 mm Hg). For each patient, three valid recordings were included in the analysis.
TG performance by experienced and non-experienced users
In the third part of the study, we analyzed the influence of experience with TG on the reliability of the calculated cfPWV values. Twenty-four patients were included. During a routine ambulatory visit, the patients were asked to perform TG recordings without a preliminary explanation of the operating procedure (that is, the patients were non-experienced users). Afterwards, an experienced user performed a recording. The cfPWV values were included in the analysis only if the MAP between single recordings from experienced and non-experienced users was stable, and MAP was accepted as stable within a wide range of variation (<15 mm Hg). All patients were familiar with the general procedures for the brachial blood pressure measurement with automatic oscillometric devices. For each patient, one valid recording obtained from a non-experienced user and one corresponding recording obtained from an experienced user were included in the analysis.
Statistical analyses
The mean and s.d. were calculated for each continuous variable. The comparison between the standard method and test method was performed using the Bland–Altman approach. P-values <0.05 were considered statistically significant. Analyses were performed using GraphPad Prism 5 (GraphPad Software, La Jolla, CA, USA) and SPSS Statistics 21.0 (IBM, New York City, NY, USA).
Results
The validation procedure and assessment of cfPWV variation
Overall, 89 patients were prospectively included in this part of the study. The mean age was 48.8±19.1 years. Following the requirements of the ARTERY Society, 25 of the patients were younger than 30 years, 32 of the patients were between 30 and 60 years old and 32 of the patients were older than 60 years.16 The mean body mass index was 24.7±4.7 kg m−2, and the mean PWV was 7.8±2.3 m s−1 obtained with TG and 7.3±1.65 m s−1 obtained with SC. A wide range of PWV with a minimum of 4.6 and a maximum of 11.6 m s−1 was captured in the study. More than half (59.6%) of the patients were male, and 15.1% were smokers. The baseline characteristics for the study sample are summarized in Table 1.
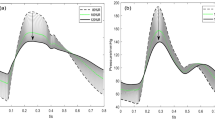
The mean difference in PWV between the test and reference devices was 0.49±1.26 m s−1 (P<0.0001). The Pearson correlation index was r=0.86 (P<0.0001) (Figure 1).
The mean difference between the first, second and third measurement with the TG compared with the mean PWV obtained with the SC was 0.58±1.25, 0.41±1.56 and 0.47±1.22 m s−1, respectively. There was no significant distinction in mean PWV differences between the TG and SC, when the mean of three values measured with TG or the first, second or third single value was assessed (Figure 2). The coefficient of variation between a single cfPWV value was significantly lower with TG than with SC (2.38±6.13% vs. 6.3±4.33% (P<0.05), respectively). ICC between the single values were higher with TG than with SC. The s.d. of the mean PWV differences between the single values were lower with TG than with SC. Table 2 presents an overview of these reproducibility and variation parameters.
TG performance in supine and seated positions
Overall, 15 patients were included in this part of the study. The mean age was 49.8±16.0 years, and 33.3% were male. The mean body mass index was 24.5±4.0 kg m−2. The mean difference of the PWV values measured in supine and seated positions with TG was 0±0.27 m s−1. The Pearson correlation index was r=0.99 (P<0.0001) (Figure 3).
TG performance by experienced and non-experienced users
Overall, 24 patients were included in this part of the study. The mean age was 50.3±15.2 years, and 40% were male. The mean body mass index was 24.7±3.9 kg m−2. The mean difference in the PWV values in non-experienced and experienced users measured using TG was 0±0.20 m s−1. The Pearson correlation index was r=0.96 (P<0.0001) (Figure 4).
Discussion
In this study, we evaluated the performance of an oscillometry-based assessment technique using TG for the calculation of PWV with a particular interest in the possible utilization of this technology in everyday clinical practice. In the first part of the study, we compared the accuracy of cfPWV measurements made with TG and SC, which uses tonometry for the determination of cfPWV and has been used in clinical trials to provide independent prognostic values.16, 17, 18 We detected a small but statistically significant difference of 0.49 m s−1 between TG and SC, suggesting that TG mildly overestimates the calculated PWV compared with SC. According to the accuracy requirements established by the ARTERY Society,16 TG demonstrated excellent accuracy for the mean difference (<0.5 m s−1) and acceptable accuracy for the s.d. (⩽1.5 m s−1). Several other commercial devices are available for the non-invasive assessment of PWV using ultrasound, MRI and tonometry.19, 20, 21, 22 Among the devices using oscillometry, similar to TG, are the Vicorder (Skidmore Medical, Bristol, UK), Arteriograph (Tensiomed, Budapest, Hungary), Vasotens (OOO Petr Telegin, Nizhny Novgorod, Russia) and Mobil-O-Graph (I.E.M.).15, 23, 24, 25 With the exception of the Mobil-O-Graph, which shares the same mathematical algorithm as the TG, all devices necessitate additional measurement of the travel distance between two sites (usually the sternal notch and symphysis), which has been previously recognized as a major source of inaccuracy in the determination of the PWV.26 More details about the measurement techniques of the available oscillometric devices are provided in the Supplementary Information (Supplementary Table 1).
Currently, non-invasive cfPWV assessments are easy to perform, but their widespread use in everyday clinical practice is limited due to the complex analysis procedure, which requires repeated measurements to establish adequate reliability of the obtained cfPWV values. This fact makes the determination of clinically relevant data difficult. We, thus, analyzed the degree of variation of the singly measured cfPWV values with TG to assess the reliability of this oscillometric measurement. With a low coefficient of variation, a low s.d. of the mean difference and high ICC, all obtained variation assessment parameters indicated the high reliability and robustness of the measured intra-individual values. Compared with TG, SC showed higher variation indices of the single measured intra-individual PWV in our study population, indicating inferior robustness (Table 2). High cfPWV measurement reliability was also highlighted by the fact that comparable accuracy for TG could be shown independent of whether a single PWV value or an average of three values was used in a comparison with an average of the PWV values obtained by SC (Figure 2). Our results suggest that due to the low between-value variation, a single measurement of cfPWV with TG is adequate for the calculation of a reliable and clinically relevant cfPWV value. This is of special interest for everyday clinical practice.
Few previous studies have addressed the reliability and reproducibility of the cfPWV measurements obtained non-invasively during a single visit. A very high ICC can be achieved using ultrasonography in the assessment of cfPWV.19, 27 In the most recent study, Meyer et al.28 reported a s.d. of 1.13 m s−1 for the mean difference between two single PWV measurements during one visit obtained by the VP 1000. Papaioannou et al.29 also found high ICC between single cfPWV values obtained with the Complior (Alam Medical, France), though the coefficient of variation was higher than that achieved with TG in our study. One study reported a lower s.d. for the mean difference (0.81 m s−1) for SC compared with that obtained with SC in our study. In contrast, the same study reported a higher coefficient of variation (9%) compared with that obtained for SC in our study. The reliability and repeatability of the Vicorder have been simultaneously assessed, and the s.d. of the mean difference between two measured cfPWV values of 2.29 m s−1 is unsatisfactory.30 To our knowledge, this is the only study to assess the reproducibility and reliability of the oscillometric-based measurement of cfPWV.
To establish a method suitable for routine measurement in everyday clinical practice, it is optimal to be able to reveal reliable results in various clinical circumstances. An important clinical circumstance is the body position required during the measurement. Usually, cfPWV measurement procedures require the patient to be in a supine position.16 In the second part of the study, we compared cfPWV values obtained with TG in supine and seated positions and found reliable results independent of the patient’s body position.
Finally, we sought to determine whether any experience with TG is required to obtain valid and reliable data. Thus, in the third part of the study, we compared the cfPWV values obtained when the measurement procedure was performed by our patients (non-experienced users) with the values obtained for an experienced user. We could not detect any significant difference between the cfPWV values based on user experience.
To our knowledge, our study was the first to address the performance of the oscillometric cfPWV measurement in different clinical situations such as the patient’s body position or levels of user experience.
The present study has some limitations. First, this study lacks a comparison to the invasive measurement of PWV, which was not performed because of the obvious risks of the invasive procedure in our low-risk outpatient study population. One of the independent variables included in the formula for calculation of the PWV with TG is brachial blood pressure. Thus, inaccuracies in the blood pressure measurement could cause inaccuracies in PWV assessment with TG. Though the requirements of the ARTERY Society were fulfilled, further studies are needed to confirm the generalizability of the reported results, especially, because some factors could differentially influence cfPWV values calculated by TG and values obtained conventionally. As already described, we observed incremental changes in the cfPWV values obtained with TG or SC with increased age (Supplementary Table 2).
In conclusion, our study extends the evidence supporting the feasibility of an oscillometry-based approach for the non-invasive assessment of cfPWV. A unique finding was the observation of very high reproducibility and low variation between single measurements of cfPWV values with TG in comparison with the previously reported, although limited, data obtained using tonometric and another oscillometric devices. These results lead to the conclusion that one measurement is sufficient for obtaining a reliable cfPWV value with TG. In addition, the measurements remained robust independent of the patient‘s body position or experience.
Overall, it can be concluded that oscillometry might evolve to become the favored method for the assessment of cfPWV in everyday clinical practice and in clinical studies due to its ease of performance with concurrent reliability and accuracy. One of the essential prerequisites for new measurements seem to be the removal of the travel distance measurement from the PWV calculation, as is realized in TG.
References
Laszlo A, Reusz G, Nemcsik J . Ambulatory arterial stiffness in chronic kidney disease: a methodological review. Hypertens Res 2016; 39: 192–198.
Boardman H, Birse K, Davis EF, Whitworth P, Aggarwal V, Lewandowski AJ, Leeson P . Comprehensive multi-modality assessment of regional and global arterial structure and function in adults born preterm. Hypertens Res 2016; 39: 39–45.
Peng F, Pan H, Wang B, Lin J, Niu W . The impact of angiotensin receptor blockers on arterial stiffness: a meta-analysis. Hypertens Res 2015; 38: 613–620.
Vlachopoulos C, Aznaouridis K, Stefanadis C . Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010; 55: 1318–1327.
Saji N, Kimura K, Yagita Y, Kawarai T, Shimizu H, Kita Y . Comparison of arteriosclerotic indicators in patients with ischemic stroke: ankle-brachial index, brachial-ankle pulse wave velocity and cardio-ankle vascular index. Hypertens Res 2015; 38: 323–328.
Schillaci G, Battista F, Settimi L, Anastasio F, Pucci G . Cardio-ankle vascular index and subclinical heart disease. Hypertens Res 2015; 38: 68–73.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA . 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159–2219.
Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, Heffernan KS, Lakatta EG, McEniery CM, Mitchell GF, Najjar SS, Nichols WW, Urbina EM, Weber T . Recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement from the American Heart Association. Hypertension 2015; 66: 698–722.
Townsend RR, Wimmer NJ, Chirinos JA, Parsa A, Weir M, Perumal K, Lash JP, Chen J, Steigerwalt SP, Flack J, Go AS, Rafey M, Rahman M, Sheridan A, Gadegbeku CA, Robinson NA, Joffe M . Aortic PWV in chronic kidney disease: a CRIC ancillary study. Am J Hypertens 2010; 23: 282–289.
McEniery CM, Spratt M, Munnery M, Yarnell J, Lowe GD, Rumley A, Gallacher J, Ben-Shlomo Y, Cockcroft JR, Wilkinson IB . An analysis of prospective risk factors for aortic stiffness in men: 20-year follow-up from the Caerphilly prospective study. Hypertension 2010; 56: 36–43.
Miljkovic D, Perret-Guillaume C, Alla F, Salvi P, Erpelding ML, Benetos A . Correlation between peripheral blood pressure and pulse-wave velocity values in the institutionalized elderly persons 80 years of age and older: the PARTAGE study. Am J Hypertens 2013; 26: 163–173.
Reshetnik A, Gohlisch C, Zidek W, Tolle M, van der Giet M . Validation of the Tel-O-GRAPH, a new oscillometric blood pressure-measuring device, according to the British Hypertension Society protocol. Blood Press Monit (e-pub ahead of print 19 April 2016; doi:10.1097/MBP.0000000000000195).
Wassertheurer S, Kropf J, Weber T, van der Giet M, Baulmann J, Ammer M, Hametner B, Mayer CC, Eber B, Magometschnigg D . A new oscillometric method for pulse wave analysis: comparison with a common tonometric method. J Hum Hypertens 2010; 24: 498–504.
Wassertheurer S, Mayer C, Breitenecker F . Modeling arterial and left ventricular coupling for non-invasive measurements. Simul Model Pract Theory 2008; 16: 988–997.
Hametner B, Wassertheurer S, Kropf J, Mayer C, Holzinger A, Eber B, Weber T . Wave reflection quantification based on pressure waveforms alone—methods, comparison, and clinical covariates. Comput Methods Programs Biomed 2013; 109: 250–259.
Wilkinson IB, McEniery CM, Schillaci G, Boutouyrie P, Segers P, Donald A, Chowienczyk PJ . ARTERY Society guidelines for validation of non-invasive haemodynamic measurement devices: part 1, arterial pulse wave velocity. Artery Res 2010; 4: 34–40.
Reference Values for Arterial Stiffness C. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: 'establishing normal and reference values'. Eur Heart J 2010; 31: 2338–2350.
McEniery CM, Yasmin, Hall IR, Qasem A, Wilkinson IB, Cockcroft JR . ACCT Investigators. Normal vascular aging: differential effects on wave reflection and aortic pulse wave velocity: the Anglo-Cardiff Collaborative Trial (ACCT). J Am Coll Cardiol 2005; 46: 1753–1760.
Calabia J, Torguet P, Garcia M, Garcia I, Martin N, Guasch B, Faur D, Valles M . Doppler ultrasound in the measurement of pulse wave velocity: agreement with the Complior method. Cardiovasc Ultrasound 2011; 9: 13.
Joly L, Perret-Guillaume C, Kearney-Schwartz A, Salvi P, Mandry D, Marie PY, Karcher G, Rossignol P, Zannad F, Benetos A . Pulse wave velocity assessment by external noninvasive devices and phase-contrast magnetic resonance imaging in the obese. Hypertension 2009; 54: 421–426.
Salvi P, Lio G, Labat C, Ricci E, Pannier B, Benetos A . Validation of a new non-invasive portable tonometer for determining arterial pressure wave and pulse wave velocity: the PulsePen device. J Hypertens 2004; 22: 2285–2293.
Cortez-Cooper MY, Supak JA, Tanaka H . A new device for automatic measurements of arterial stiffness and ankle-brachial index. Am J Cardiol 2003; 91: 1519–1522 A9.
Hickson SS, Butlin M, Broad J, Avolio AP, Wilkinson IB, McEniery CM . Validity and repeatability of the Vicorder apparatus: a comparison with the SphygmoCor device. Hypertens Res 2009; 32: 1079–1085.
Trachet B, Reymond P, Kips J, Swillens A, De Buyzere M, Suys B, Stergiopulos N, Segers P . Numerical validation of a new method to assess aortic pulse wave velocity from a single recording of a brachial artery waveform with an occluding cuff. Ann Biomed Eng 2010; 38: 876–888.
Kotovskaya YV, Kobalava ZD, Orlov AV . Validation of the integration of technology that measures additional ‘vascular’ indices into an ambulatory blood pressure monitoring system. Med Devices 2014; 7: 91–97.
Segers P, Kips J, Trachet B, Swillens A, Vermeersch S, Mahieu D, Rietzschel E, De Buyzere M, Van Bortel L . Limitations and pitfalls of non-invasive measurement of arterial pressure wave reflections and pulse wave velocity. Artery Res 2009; 3: 79–88.
Magda SL, Ciobanu AO, Florescu M, Vinereanu D . Comparative reproducibility of the noninvasive ultrasound methods for the assessment of vascular function. Heart Vessels 2013; 28: 143–150.
Meyer ML, Tanaka H, Palta P, Patel MD, Camplain R, Couper D, Cheng S, Al Qunaibet A, Poon AK, Heiss G . Repeatability of central and peripheral pulse wave velocity measures: the Atherosclerosis Risk in Communities (ARIC) Study. Am J Hypertens 2015; 29: 470–475.
Papaioannou TG, Protogerou AD, Nasothimiou EG, Tzamouranis D, Skliros N, Achimastos A, Papadogiannis D, Stefanadis CI . Assessment of differences between repeated pulse wave velocity measurements in terms of 'bias' in the extrapolated cardiovascular risk and the classification of aortic stiffness: is a single PWV measurement enough? J Hum Hypertens 2012; 26: 594–602.
van Leeuwen-Segarceanu EM, Tromp WF, Bos WJ, Vogels OJ, Groothoff JW, van der Lee JH . Comparison of two instruments measuring carotid-femoral pulse wave velocity: Vicorder versus SphygmoCor. J Hypertens 2010; 28: 1687–1691.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Reshetnik, A., Gohlisch, C., Tölle, M. et al. Oscillometric assessment of arterial stiffness in everyday clinical practice. Hypertens Res 40, 140–145 (2017). https://doi.org/10.1038/hr.2016.115
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2016.115
Keywords
This article is cited by
-
Low muscle strength and increased arterial stiffness go hand in hand
Scientific Reports (2021)
-
Was sagen die Gefäßparameter über die Gefäßalterung aus?
CardioVasc (2020)
-
Frequency of early vascular aging and associated risk factors among an adult population in Latin America: the OPTIMO study
Journal of Human Hypertension (2018)