Abstract
A significant correlation between hypertension history and high blood pressure has been observed with regard to age, race and gender. Investigating carotid intima-media thickness and aortic stiffness prior to the development of hypertension in children of hypertensive parents enabled us to evaluate these patients for subclinical atherosclerosis. We compared carotid intima-media thickness, aortic strain, distensibility, stiffness indices and elastic modulus in 67 normotensive children whose parents had a diagnosis of essential hypertension and 39 normotensive children with no parental history of hypertension. Although there were no significant differences between the two groups in terms of systolic blood pressure, diastolic blood pressure, average blood pressure and pulse pressure (P>0.05), systolic blood pressures were higher among patients 15 years and older in the study group. No significant differences were noted between the control and study groups regarding interventricular septal thickness, left-ventricular posterior wall thickness, left-ventricular systolic and diastolic diameter and aortic annulus diameter (P>0.05). The left atrium diameter was larger in the study group compared with that in the control group, mainly because of the values of the 15-year-old and older children (P=0.01). The mean, maximum and minimum values of carotid intima-media thickness were significantly different in the study group compared with the control group among all age groups (P<0.001, P<0.001, P=0.006, respectively). Aortic systolic and diastolic diameters were larger in normotensive children of hypertensive parents compared with the control group (P=0.014, P=0.001, respectively). Although there were no differences between the study and control groups regarding aortic strain, aortic distensibility, elastic modulus and stiffness indices (P>0.05), aortic distensibility was lower, and aortic stiffness indices were higher among children 15 years and older in the study group. An increase in the carotid intima-media thickness in all age groups and a decrease in aortic elastic properties in 15-year-old and older children of hypertensive parents may indicate subclinical atherosclerosis in these apparently healthy children.
Similar content being viewed by others
Introduction
Hypertension is one of the most common reasons for hospital visits in adults worldwide, with the incidence rate increasing in children and adolescents.1, 2 Children of hypertensive parents have higher blood pressures compared with children of normotensive parents, particularly during adolescence.3, 4 Therefore, early diagnosis of atherosclerosis at the subclinical phase may alert clinicians about atherosclerosis-related disease such as hypertension and may contribute to the prevention or at least the delay of the disease with measures taken early before clinical presentation of the disease.
Carotid intima-media thickness may be indicative of an asymptomatic vascular disease, as suggested by several researchers.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 Increased carotid intima thickness is a valid index and early indicator of disseminated atherosclerosis. Studies conducted in adult populations have demonstrated significant correlations between high carotid intima thickness values and myocardial infarction, stroke, premature death and cardiovascular events.10, 11, 12, 14, 15, 16, 17
Arterial stiffness is the term most commonly used to define the viscoelastic characteristics of the arterial wall. It occurs as a result of aging and increased atherosclerotic risk factors, including smoking, hypercholesterolemia, diabetes mellitus and hypertension. Arterial stiffness is an independent indicator of coronary heart disease in patients with essential hypertension.18
Normotensive children of hypertensive parents experience cardiovascular changes earlier in life compared with children of normotensive parents.19 Kolo et al.20 demonstrated that the left-ventricular mass of normotensive children with hypertensive parents was increased prior to the development of hypertension compared with control subjects; they concluded that this increase and the presence of diastolic dysfunction were early signs of hypertension.
Assessments of aortic stiffness and carotid intima-media thickness are less commonly done in children. Carotid intima-media thickness and aortic stiffness were investigated to search for endothelial dysfunction or atherosclerosis, which accompanies diseases such as obesity, type I diabetes, intrauterine growth restriction, hypercholesterolemia, hypertension and end-stage renal failure in children.21, 22, 23, 24, 25 Although there are limited numbers of studies evaluating carotid intima-media thickness and aortic stiffness in hypertensive children, very few studies regarding carotid intima-media thickness and aortic stiffness in normotensive children of hypertensive parents have been undertaken. Carotid intima-media thickness and arterial stiffness are increased in normotensive adolescents and young adults with hypertensive parents.26, 27, 28, 29, 30, 31, 32
The aim of this study was to determine if subclinical atherosclerosis was present in children with hypertensive parents and to determine whether arterial stiffness and carotid intima-media thickness are indicators of hypertension during adulthood. Furthermore, this study also aimed to determine the time period in which carotid intima-media thickness and arterial stiffness increase in normotensive children of hypertensive parents.
Materials and methods
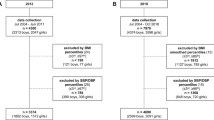
A total of 106 children, including 39 normotensive children without any familial history of hypertension and 67 normotensive children who presented to Eskisehir Osmangazi University Medical School, Pediatric Cardiology Department with noncardiac chest pain, an innocent murmur or a family history of essential hypertension were included in this study. A signed consent form was obtained after informing families of the aims and principles of the study. Consent for the study protocol was obtained from the ethics committee of Eskisehir Osmangazi University Medical School, with a consent date of 27 January 2012/03.
The children were divided into the following two groups: group 1 consisted of children with hypertensive mothers or fathers (n=67), and the control group consisted of children with no familial history of hypertension (n=39). Comparisons between the two groups were made based on echocardiographic findings, carotid intima thickness and aortic stiffness. To compare changes in several parameters, including blood pressure, echocardiographic findings, carotid intima-media thickness and aortic stiffness, the children were also divided into the following three subgroups: age 10 years or below, between 11 and 15 years of age, and above 15 years of age.
Children with parents with essential hypertension who regularly used antihypertensive medications and were without any history of additional illnesses causing secondary hypertension were included in the present study. Children with a parental history of cardiovascular disease, chronic renal failure, diabetes, hyperlipidemia, obesity or smoking were excluded from the study.
Detailed personal and familial medical histories of the children were recorded. Exclusion criteria included chronic illness, history of prematurity, anemia and medication use. Children with normal physical examination findings were included in the present study. Biochemical laboratory tests such as complete blood count, erythrocyte sedimentation rate and low-density lipoprotein, high-density lipoprotein, triglyceride and total cholesterol concentrations were performed for all children. Children with congenital heart disease, chronic renal failure, diabetes, hyperlipidemia and obesity were excluded from the study.
Height was measured by using a calibrated standard height scale, with each child in an upright position and not wearing shoes. Body mass index was calculated by using the following formula: weight (kg)/height2 (m2). Blood pressure was measured three times by using a mercury sphygmomanometer by employing an appropriate armband on each seated child following 10 min of rest, and mean blood pressures were recorded. When Korotkoff sounds were heard over the brachial artery, the armband was inflated by 20 mm Hg, above the point at which brachial pressure was not apparent; the pressure was subsequently decreased by releasing the air at a rate of 2–3 mm Hg s−1. The first Korotkoff sound represented each patient’s systolic pressure, whereas the fourth Korotkoff sound represented each patient’s diastolic blood pressure (DBP) in children under the age of 12; the fifth Korotkoff sound represented each patient’s diastolic pressure in children over the age of 12.
Echocardiographic evaluation
Echocardiography was performed by an experienced pediatric cardiologist using a Hewlett Packard Sonos 5500 (Indianapolis, IN, USA) with 2–4 and 4–8 MHz broadband probes. Following standard echocardiographic examinations, M-mode, 2D long axis ascending aortic recordings were obtained with patients in the supine position. These M-mode ascending aortic recordings were measured ~2 cm above the aortic valve. Aortic valve diameters were calculated by using the diameter between the inferior rims of anterior and posterior aortic walls during systole and diastole. The systolic diameter of the aorta was measured with the valve open, and the diastolic diameter was determined simultaneously by using the QRS wave peak on Elecrtrocardiogram; these measurements were repeated over five successive beats, and the means of these recordings were obtained. Additional echocardiographic measurements, such as left-ventricular ejection fraction, left-ventricular end systolic diameter, left-ventricular end diastolic diameter, left-ventricular posterior wall thickness and interventricular septal thickness were obtained by using M-mode in the long axis.
Carotid intima-media measurements
All individuals were evaluated by using Vivid I color Doppler ultrasonography with a 12-MHz linear probe. During the evaluation, each child was supine, with a thin pillow under the neck and the neck turned in the opposite direction. A 1-cm segment within a 2-cm area distal to the main carotid arterial bulbous was noted, and the images were transferred to a computer. The mean, minimum and maximum values for the designated segment were calculated by using a special intima-media thickness assessment program based on distant rim measurements. These measurements were also repeated, and mean values were obtained for both main carotid arteries.
Determination of aortic elasticity features
Elastic features of aorta were considered indicators of the elastic function of the aorta. Mean systolic blood pressure (SBP) and DBP were calculated by acquiring pressures from the right and the left arm; pulse pressures were estimated by subtracting SBP from diastolic pressure. The following parameters were analyzed: aortic systolic diameter (AoS), aortic diastolic diameter (AoD), SBP and DBP:33

Statistical analysis
The IBM SPSS Statistics 20 (Chicago, IL, USA) program was used for statistical analysis. The consistency of the variables was assessed by using the Shapiro–Wilk test. The variables with normal distributions were analyzed with a t-test for independent samples and expressed as the means±s.d. The Mann–Whitney U-test was performed for variables with non-normal distributions, and the median and percentile values (25–75%) were obtained. To evaluate the relationship among the variables, a Spearman correlation analysis was performed. P<0.05 was considered statistically significant.
Results
Group 1 consisted of 67 children (ages 7–19), and group 2 consisted of 39 children (ages 7–18). Comparisons of anthropometric features, blood pressures and echocardiographic variables of the groups are included in Table 1. There were no significant differences between the study and control groups regarding gender, age, weight, height, body mass index, SBP and DBP and pulse pressure (P<0.05). Similarly, interventricular septal thickness, left-ventricular posterior wall thickness, left-ventricular systolic and diastolic diameters, end-systolic and end diastolic left-ventricular masses and aortic annulus diameter did not differ between the groups (P>0.05). Left atrial diameter was significantly larger in the study group compared with the control group (P=0.01). Comparisons of blood pressures and echocardiographic variables based on each age group are included in Table 2. SBP (P<0.05), left-ventricular systolic (P<0.05), diastolic mass (P<0.01), aortic diameter (P<0.05) and left-atrial diameter (P<0.001) were significantly larger in the study group among patients over 15 years of age.
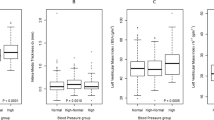
The distributions of carotid intima-media thickness and aortic stiffness variables are included in Table 3. Mean, maximum and minimum carotid intima-media thickness values were significantly higher in the study group compared with the control group (P<0.001, P<0.001, P<0.006, respectively). The systolic (P=0.01) and diastolic diameters (P=0.001) of the ascending aorta were significantly larger in the study group, but no differences were noted among the indices of aortic strain, distensibility, elastic modulus and stiffness compared with the control group (P>0.05). Table 4 includes comparisons of carotid intima-media thickness and aortic stiffness based on each age group. Significantly higher mean (P<0.05, P<0.05, P<0.05, respectively) and maximum carotid intima-media thicknesses (P<0.05, P<0.05, P<0.01, respectively) were noted in the study groups of each age group. Although aortic distensibilities were lower and stiffness indices were higher among patients 15 years of age and older in the study group (P<0.05, P<0.05, respectively), no differences were noted between the study and the control groups among children younger than 15 years of age (P>0.05). Likewise, no significant differences were noted between the study and the control groups regarding minimum carotid intima-media thickness, pulse pressure, aortic strain and elastic modulus among all age groups (P>0.05).
In our study, the fathers of 36 children and the mothers of 25 children were hypertensive. Of these, both mothers and fathers of six children had hypertension. The distribution of aortic stiffness variables and carotid intima-media thicknesses based on parental hypertension are summarized in Table 5. No significant differences were noted regarding pulse pressure, aortic strain or carotid intima-media thickness in the children of hypertensive mothers compared with the children of hypertensive fathers (P>0.05). However, children with hypertensive mothers demonstrated significantly lower aortic distensibility and higher elastic modulus and aortic stiffness indices compared with children with hypertensive fathers (P=0.02, P<0.02, P<0.01, respectively).
Discussion
The present study demonstrated that although SBP, DBP and the mean blood pressure were higher in the study group compared with control subjects, no statistically significant differences were noted regarding blood pressure values among normotensive children of hypertensive parents. Previous studies noted significant correlations between family histories of hypertension and high blood pressures.34, 35, 36, 37, 38 By contrast, Dernelis et al.31 (age range 12–16) and Evrengul et al.39 (age range 18–22) did not observe any significant changes in the blood pressures of normotensive children with hypertensive parents compared with controls. To evaluate the alterations in carotid intima-media thickness prior to the development of hypertension in children with hypertensive parents, pre-hypertensive and hypertensive children of hypertensive parents were excluded from the study. The development of hypertension occurs during adolescence and young adulthood; however, the age range of the study and the control groups was lower in our study (7–19 years).
There were no statistically significant differences between the study group and the control groups regarding SBP and DBP because hypertensive children were excluded from the study. When the normotensive children of hypertensive parents were divided into age groups, SBP was significantly higher in children 15 years of age and older compared with controls. However, systolic and diastolic pressures did not differ among children younger than 15. In previous studies, significant correlations were noted between family histories of hypertension and the incidence of high blood pressure, particularly following adolescence.34, 35, 36, 37, 38 SBP levels were elevated after the age of 15 in the study group compared with controls after the children were separated based on their ages. This result indicated that clinical findings may be observed in normotensive children of hypertensive parents, particularly following adolescence.
Comparisons of left-atrial diameter demonstrated that the atria were significantly larger in normotensive children of hypertensive parents; conversely, no differences were noted regarding the remaining echocardiographic data. When the echocardiographic findings were assessed based on patients’ ages, left-ventricular diastolic and systolic masses and aortic and left-atrial diameters were each significantly higher in the study group among children 15 years of age and older; there were no significant differences in these parameters among children younger than 15. Kolo et al.20 noted that increased left-ventricular mass and diastolic dysfunction were early signs of hypertension, and diastolic dysfunction was observed without an increased left-ventricular mass in the normotensive children of hypertensive parents. Increased left-ventricular diameter represents one of the most prominent signs of diastolic dysfunction.39, 40 The presence of an enlarged left ventricle in children of hypertensive parents and increased left-ventricular mass in children over the age of 15 indicated that signs of diastolic dysfunction may develop early in life.
The mean, maximum and minimum measurements of carotid intima-media thickness were significantly higher in the study group compared with control subjects. When patients were divided into subgroups based on age, increased mean and maximum carotid intima-media thickness was observed among patients of all ages in the study group. Studies comparing carotid intima-media thickness and aortic stiffness in normotensive children of hypertensive parents with children of normotensive parents revealed that carotid intima-media thickness increased in both adolescents and young adults.24, 25, 26, 27, 28, 29, 30, 41, 42, 43, 44 Evelein et al.27 found that carotid intima-media thickness was higher in children older than 5 years of age compared to controls, an increase that may be observed as early as at the age of 5. Xiang et al.26 evaluated 206 children aged 16 years and older from 69 hypertensive families and demonstrated that carotid intima-media thickness was increased, an increase that correlated with both age and genetic factors. They also emphasized that although genetic factors were stronger determinants at an early age, environmental factors made a more significant impact later in life. Cuomo et al.24 demonstrated significantly elevated carotid intima-media thickness in 29 individuals between the ages of 11 and 30 with a family history of hypertension compared with control subjects.
Carotid intima-media thickness is used to evaluate adults for subclinical atherosclerosis and future cardiovascular risk. Our study confirmed that carotid intima-media thickness was elevated in children with hypertensive parents, beginning at an early age. This elevation may indicate the presence of subclinical atherosclerosis within vascular beds without accompanying changes in blood pressure or echocardiographic findings. Elevated carotid intima-media thickness may be considered a risk factor for hypertension and future cardiovascular disease. Although cardiovascular events are rarely observed during childhood and adolescence, an early determination or prediction of possible diseases associated with endothelial dysfunction and atherosclerosis based on carotid intima-media thickness and aortic stiffness may be important in preventing the progression and complications of these diseases. Even in the absence of hypertension and other risk factors, diet and lifestyle changes may be recommended in the setting of elevated carotid intima-media thickness during childhood, particularly in normotensive children of hypertensive parents.
Ascending aortic systolic and diastolic diameters were larger in normotensive children of hypertensive parents compared with controls. However, there was no difference regarding aortic strain, distensibility, elastic modulus and stiffness indices when subjects were divided into subgroups based on age. Aortic distensibility was significantly lower, and stiffness indices were higher in children older than 15 years of age in the study group. There are very limited numbers of studies regarding carotid and aortic stiffness in normotensive children with hypertensive parents.28, 29, 30, 39 Kyvelou et al.28 evaluated 143 children between the ages of 14–30 of hypertensive parents and demonstrated that carotid and aortic stiffness increased independently of anthropometric (age, weight and body mass index) and biochemical parameters (glucose, cholesterol and triglyceride); these increases were significantly higher in children with hypertensive parents.
Evrengul et al.39 observed elevated aortic stiffness and diminished distensibility in normotensive children between the ages of 18–22 years with hypertensive parents compared with the controls. They concluded that a history of parental hypertension may increase an individual’s predisposition to aortic stiffness and cause subclinical atherosclerosis in the absence of hypertension; therefore, hypertension and atherosclerosis may develop in the future. Kucerova et al.30 noted increased aortic stiffness values compared with controls, and they reported that these increases became more prominent with age and blood pressure in 174 children between the ages of 14 and 40 with at least one hypertensive parent. By contrast, Zhou et al.42 evaluated 270 subjects between 16 and 30 years of age and observed decreased compliance in the great elastic and small muscular vessels of subjects with a history of hypertension, a decrease that was statistically significant in men.
The compliance of the great vessels correlated with SBP and DBP; small vessel compliance was independent of blood pressure and correlated with a familial history of hypertension. Aortic stiffness is a useful parameter for determining hypertension; therefore, early preventive measures should be utilized in individuals with increased aortic stiffness. Meaney et al.29 noted increased carotid stiffness and unchanged aortic stiffness and pulse pressures in 50 children between the ages of 10–21 years with a family history of hypertension compared with controls. Rajzer et al.43 noted results consistent with those obtained by Meaney et al.29 The age range of our study was similar to that studied by Meaney et al.29 The age range of the children with hypertensive parents was higher in these studies, each of which demonstrated increased aortic and carotid stiffness compared with our study. Subjects older than 15-20 years of age with a parental history of hypertension demonstrated elevated aortic stiffness. The finding of lower aortic distensibility in subjects over 15 years of age in our study suggests that aortic stiffness may be affected following adolescence.
Aortic distensibility was significantly lower, and elastic modulus was higher in children with hypertensive mothers in our study. Evalein et al.27 evaluated children older than 5 years of age and demonstrated that carotid intima-media thickness was increased in children with hypertensive mothers and that both carotid intima-media thickness and aortic stiffness were increased in children with hypertensive mothers and fathers. Rodrigues–Moran et al.44 demonstrated that cardiovascular risk factors such as high blood pressure, hyperglycemia, hyperinsulinemia and low high-density lipoprotein were affected more significantly in children with a maternal history of hypertension compared with children with a paternal history of hypertension in a study involving normotensive children between 6–10 years of age with hypertensive parents. They concluded that a maternal history of hypertension is a more significant cardiovascular risk factor for children. They speculated that an individual’s cardiovascular risk may be hereditary via mitochondria. Aortic stiffness is increased in children with a maternal history of hypertension. As suggested by Rodrigues–Moran et al.,44 we believe that cardiovascular risk factors pass to children via mitochondrial inheritance patterns and that a maternal history of hypertension increases an individual’s predisposition to hypertension and endothelial dysfunction.
Study limitations
The present study has some limitations. One of these is the small number of participants. Second, we did not examine other cardiac risk factors that might play a major role in endothelial function and atherosclerosis. Further longitudinal studies involving larger patient series and family members are warranted. Therefore, additional prospective studies that include larger series with long-term follow-up evaluation are necessary to clarify hypertension and cardiac risk factors, such as homocysteine levels or elevated C-reactive protein levels.
In conclusion, increased carotid intima-media thickness was noted in all age groups; decreased aortic distensibility and increased stiffness indices were noted in children over 15 years of age, indicating that normotensive children with hypertensive parents have developed subclinical atherosclerosis and endothelial dysfunction. Increased SBP, left-ventricular mass and left-atrial size indicate that carotid intima-media thickness changes before such changes are visualized via echocardiography, particularly in children over 15 years of age, and blood pressure, left-ventricular mass, left-atrial size and aortic stiffness are affected following adolescence. Despite the fact that cardiovascular events are rare in adolescence, endothelial dysfunction and atherosclerosis-related diseases may be predicted by using carotid intima-media thickness and aortic stiffness, which may slow disease progression and prevent complications. Diet and lifestyle modifications may be recommended in the absence of other cardiovascular risk factors, particularly in the setting of increased carotid intima-media thickness in normotensive children with hypertensive parents.
References
Staessen JA, Wang J, Bianchi G . Essential Hypertension. Lancet 2003; 261: 1629–1641.
Karpettas N, Nasothimiou E, Kollias A, Vazeou A, Stergiou GS . Ambulatory and home blood pressure monitoring in children and adolescents: diagnosis of hypertension and assessment of target-organ damage. Hypertens Res 2013; 36: 285–292.
Waeber B, Brunner HR, Burnier M . Hypertension. In Willerson JT, Cohn JN (eds). Cardiovascular Medicine 2th edn.Springer, Philadelphia. 2000, 1496–1511.
Robinson RF, Batisky DL, Hayes JR . Body mass index in primary and secondary pediatric hypertension. Pediatr Nephrol 2004; 19: 1379–1384.
Davis PH, Dawson JD, Mahoney LT, Lauer RM . Increased carotid intimal- medial thickness and coronary calcification are related in young and middle-aged adults. The Muscatine study. Circulation 1999; 100: 838–842.
Smilde TJ, van Wissen S, Wollersheim H, Kastelein JJ, Stalenhoef AF . Genetic and metabolic factors predicting risk of cardiovascular disease in familial hypercholesterolemia. Neth J Med 2001; 59: 184–195.
Salonen JT, Salonen R . Ultrasonographically assessed carotid morphology and the risk of coronary heart disease. Arterioscler Thromb 1991; 11: 1245–1249.
Bruckert E, Giral P, Salloum J, Kahn JF, Dairou F, Truffert J, Reverdy V, Thomas D, Evans J, Grosgogeat Y . Carotid stenosis is a powerful predictor of a positive exercise electrocardiogram in a large hyperlipidemic population. Atherosclerosis 1992; 92: 105–114.
Bots ML, Hoes AW, Koudstaal PJ, Hofman A, Grobbee DE . Common carotid intima-media thickness and risk of stroke and myocardial infarction: the Rotterdam Study. Circulation 1997; 96: 1432–1437.
Hodis HN, Mack WJ, LaBree L, Selzer RH, Liu CR, Liu CH, Azen SP . The role of carotid artery intima-media thickness in predicting clinical coronary events. Ann Intern Med 1998; 128: 262–269.
McGill HC Jr, McMahan CA, Herderick EE, Tracy RE, Malcom GT, Zieske AW, Strong JP . Effects of coronary heart disease risk factors on atherosclerosis of selected regions of the aorta and right coronary artery: PDAY research group, Pathobiological Determinants of Atherosclerosis in Youth. Arterioscler Thromb Vasc Biol 2000; 20: 836–845.
Chambless LE, Folsom AR, Clegg LX, Sharrett AR, Shahar E, Nieto FJ, Rosamond WD, Evans G . Carotid wall thickness is predictive of incident clinical stroke: the Atherosclerosis Risk in Communities (ARIC) study. Am J Epidemiol 2000; 151: 478–487.
Kitamura A, Iso H, Imano H, Ohira T, Okada T, Sato S, Kiyama M, Tanigawa T, Yamagishi K, Shimamoto T . Carotid intima-media thickness and plaque characteristics as a risk factor for stroke in Japanese elderly men. Stroke 2004; 35: 2788–2794.
Rosvall M, Janzon L, Berglund G, Engstrom G, Hedblad B . Incident coronary events and case fatality in relation to common carotid intima media thickness. J Intern Med 2005; 257: 430–437.
van der Meer I, Bots ML, Hofman A, del Sol AI, van der Kuip DA, Witteman JC . Predictive value of noninvasive measures of atherosclerosis for incident myocardial infarction: the Rotterdam study. Circulation 2004; 109: 1089–1094.
Lorenz MW, von Kegler S, Steinmetz H, Markus HS, Sitzer M . Carotid intima-media thickening indicates a higher vascular risk across a wide age range: prospective data from the Carotid Atherosclerosis Progression Study (CAPS). Stroke 2006; 37: 87–92.
O’Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr . Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med 1999; 340: 14–22.
Laurent S, Cockcroft J, Van Bortel L . Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J 2006; 27: 2588–2605.
Garg R, Malhotra V, Dhar U, Tripathi Y . The isometric handgrip exercise as a test for unmasking hypertension in the offsprings of hypertensive parents. J Clin Diagn Res 2013; 7: 996–999.
Kolo P, Sanya E, Ogunmodede J, Omotoso A, Soladoye A . Normotensive offspring of hypertensive Nigerians have increased left ventricular mass and abnormal geometric patterns. Pan Afr Med J 2012; 11: 6.
El Samahy MH, Matter RM, Youssef OI, Shams El Din El Telbany MA, Kamal NA . Relation between carotid intima media thickness and oxidative stress markers in type 1 diabetic childrenand adolescents. J Diabetes Metab Disord 2013; 19: 12–50.
Kusters DM, Wiegman A, Kastelein JJ, Hutten BA . Carotid intima-media thickness in children with familial hypercholesterolemia. Circ Res 2014; 114: 307–310.
Lamotte C, Iliescu C, Libersa C, Gottrand F . Increased intima-media thickness of the carotid artery in childhood: a systematic review of observational studies. Eur J Pediatr 2011; 170: 719–729.
Cuomo S, Gaeta G, Guarini P, Tudisca G, De Michele M, Gene Bond M, Trevisan M . Increased carotid intima-media thickness in healthy young subjects with a parental history of hypertension (parental hypertension and vascular health). Heart 2007; 93: 368–369.
Zanardo V, Visentin S, Trevisanuto D, Bertin M, Cavallin F, Cosmi E . Fetal aortic wall thickness: a marker of hypertension in IUGR children? Hypertens Res 2013; 36: 440–443.
Xiang AH, Azen SP, Buchanan TA, Raffel LJ, Tan S, Cheng LS, Diaz J, Toscano E, Quinonnes M, Liu CR, Liu CH, Castellani LW, Hsueh WA, Rotter JI, Hodis HN . Heritability of subclinical atherosclerosis in Latino families ascertained through a hypertensive parent. Arterioscler Thromb Vasc Biol 2002; 22: 843–848.
Evelein AM, Geerts CC, Bots ML, van der Ent CK, Grobbee DE, Uiterwaal CS . Parental blood pressure is related to vascular properties of their 5-year-old offspring. Am J Hypertens 2012; 25: 907–913.
Kyvelou SM, Vyssoulis GP, Karpanou EA, Adamopoulos DN, Gialernios TP, Spanos PG, Cokkinos DV, Stefanadis CI . Arterial hypertension parental burden affects arterial stiffness and wave reflection to the aorta in young offsprings. Int J Cardiol 2010; 144: 156–160.
Meaney E, Samaniego V, Alva F, Valdovinos RA, Marrufo R, Vela A, Allen T, Misra A, Madsen R . Increased arterial stiffness in children with a parental history of hypertension. Pediatr Cardiol 1999; 20: 203–205.
Kucerová J, Filipovský J, Staessen JA, Cwynar M, Wojciechowska W, Stolarz K, Kuznetsova T, Gasowski J, Dolejsová M, Grodzicki T, Kawecka-Jaszcz K, Fagard R . Arterial characteristics in normotensive offspring of parents with or without a history of hypertension. Am J Hypertens 2006; 19: 264–269.
Dernellis J, Panaretou M . Aortic stiffness in children of parents with hypertension. J Hum Hypertens 2006; 20: 225–226.
Lurbe E, Cifkova R, Cruickshank JK, Dillon MJ, Ferreira I, Invitti C, Kuznetsova T, Laurent S, Mancia G, Morales-Olivas F, Rascher W, Redon J, Schaefer F, Seeman T, Stergiou G, Wühl E, Zanchetti A . Management of high blood pressure in children and adolescents: recommendations of the European society of hypertension. J Hypertens 2009; 27: 1719–1742.
Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker-Boudier H . Expert consensus document on arterial stiffness: methodological issues and clinical applications. European Heart Journal 2006; 27: 2588–2605.
van den Elzen AP, de Ridder MA, Grobbee DE, Hofman A, Witteman JC, Uiterwaal CS . Families and the natural history of blood pressure. A 27-year follow-up study. Am J Hypertens 2004; 17: 936–940.
Myers RH, Kiely DK, Cupples LA, Kannel WB . Parental history is an independent risk factor for coronary artery disease: the Framingham Study. Am Heart J 1990; 120: 963–969.
Grandi AM, Gaudio G, Fachinetti A, Bianchi L, Nardo B, Zanzi P, Ceriani L, Guasti L, Venco A . Hyperinsulinemia, family history of hypertension, and essential hypertension. Am J Hypertens 1996; 9: 732–738.
von Eiff AW, Gogolin E, Jacobs U, Neus H . Ambulatory blood pressure in children followed for 3 years. Influence of sex and family history of hypertension. Clin Exp Hypertens A 1986; 8: 577–581.
Munger RG, Prineas RJ, Gomez-Marin O . Persistent elevation of blood pressure among children with a family history of hypertension: the Minneapolis Children’s Blood Pressure Study. J Hypertens 1988; 6: 647–653.
Evrengul H, Tanriverdi H, Kilic ID, Dursunoglu D, Ozcan EE, Kaftan A, Kilic M . Aortic stiffness and flow-mediated dilatation in normotensive offspring of parents with hypertension. Cardiol Young 2012; 22: 451–456.
Demirpençe S, Güven B, Meşe T, Serdaroğlu E, Yılmazer MM, Firuzan E, Tavlı V . Evaluation of left atrial functions in children with chronic renal failure. Anadolu Kardiyol Derg 2014; 14: 280–285.
Barra S, Gaeta G, Cuomo S, Guarini P, Foglia MC, Capozzi G, Materazzi C, Trevisan M . Early increase of carotid intima-media thickness in children with parental history of premature myocardial infarction. Heart 2009; 95: 642–645.
Zhou L, Chen Y, Sun N, Liu X . Family history of hypertension and arteriel elasticity characterics in healty people. Hypertens Res 2008; 31: 833–839.
Rajzer MW, Klocek M, Kawecka-Jaszcz K, Czarnecka D, Baran W, Dudek K, Petriczek T . Aortic pulse wave velocity in young normotensives with a family history of hypertension. J Hypertens 1999; 17: 1821–1824.
Rodríguez-Moran M, Aradillas-García C, Simental-Mendia LE, Monreal-Escalante E, de la Cruz Mendoza E, Dávila Esqueda ME, Guerrero-Romero F . Family history of hypertension and cardiovascular risk factors in prepubertal children. Am J Hypertens 2010; 23: 299–304.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yildirim, A., Kosger, P., Ozdemir, G. et al. Carotid intima-media thickness and elastic properties of aortas in normotensive children of hypertensive parents. Hypertens Res 38, 621–626 (2015). https://doi.org/10.1038/hr.2015.49
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.49
Keywords
This article is cited by
-
Clinical Significance of Altered Vascular Morphology and Function in Normotension
Current Hypertension Reports (2023)
-
Early myocardial changes in normotensive children of hypertensive parents: a tissue Doppler study
Hypertension Research (2018)
-
Epidemiology of hypertension and survey protocols: how to count counts
Hypertension Research (2017)
-
Analysis of beat-to-beat blood pressure variability response to the cold pressor test in the offspring of hypertensive and normotensive parents
Hypertension Research (2017)
-
The influence of prehypertension, controlled and uncontrolled hypertension on left ventricular diastolic function and structure in the general Korean population
Hypertension Research (2017)