Abstract
To investigate the effects of variability in self-measured systolic blood pressure at home on the progression of cognitive impairment and white matter lesions in the oldest old. Between April 2009 and October 2009, 248 oldest old aged 80 years or older were eligibly enrolled from geriatric practices and community-dwelling areas of Shandong, China. Self-measured blood pressure at home (HBP) was measured for 7 consecutive days at the baseline, and the Mini-Mental State Examination (MMSE) score and brain white matter hyperintensities (WMH) were assessed at the baseline and during the final follow-up visit. Variability in systolic HBP was evaluated using coefficient of variation (CV) in serial daily systolic HBP measurements of the last 6 consecutive days. After an average of 2.3 years of follow-up visits, 232 oldest old were included in and 16 were excluded from the analysis. The MMSE score declined −4.76 (interquartile ranges: −10.71, −0.83) %, the periventricular WMH, deep WMH, total WMH and WMH fraction increased 16.46 (s.d.: 6.72)%, 10.05 (s.d.: 6.40)%, 14.69 (s.d.: 6.07)% and 15.95 (s.d.: 6.32)%, respectively, in the total oldest old. A declined percentage of the MMSE score and increased percentages of the periventricular WMH, deep WMH, total WMH and WMH fraction in the high group divided by tertile of the CV of the systolic HBP at baseline were greater than those in the low group (P<0.05). The significant differences were retained after adjusting for covariates, including the MMSE score, periventricular WMH, deep WMH and WMH fraction at the baseline (P<0.05). Excessive variability in self-measured systolic HBP exacerbates the progression of cognitive impairment and brain white matter lesions in the oldest old.
Similar content being viewed by others
Introduction
The oldest old, aged 80 years or older,1 is the fastest growing age group worldwide as life expectancy is steadily increasing. The risk of age-related diseases, such as cognitive impairment or dementia, develops at a higher rate and represents an important factor affecting the quality of life for the geriatric population.2, 3 Epidemiological evidence1, 4, 5 demonstrated that cognitive impairment is common in elderly subjects, with more than half of this population showing signs of dementia.6, 7, 8, 9 It is estimated that the prevalence of dementia is up to 24% in people aged 80–89 years and 37 percent in people aged 90 and older.1, 5
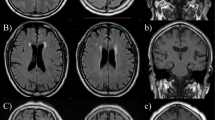
Brain white matter lesions (WMLs) are commonly observed on structural brain scans using MRI in aging individuals.10, 11 White matter hyperintensities (WMHs) are pivotal indicators and one of the pathological changes of WMLs.10, 11 WMH emerges early in the presymptomatic phase, resulting in cognitive decline.10, 12 Evidence has shown that increased WMH volume is closely associated with cognitive impairment and an increased risk of dementia.12
Alzheimer’s disease is the most prevalent early and slow onset dementia in the elderly.13 Evidence has shown that the common presentation on an MRI of the brain is frontal and/or temporal brain atrophy changes, as well as white matter changes involving frontal and parietal structures in AD.14 Barnes et al.15 found that increased WMH is independently associated with longitudinal brain volume loss in subjects who lack clinically significant cognitive decline. In addition, older subjects who have an increased WMH burden are at higher risk for the development of AD.16, 17, 18
More recently, self-measured blood pressure at home (home blood pressure, HBP) by patients is recommended by guidelines to evaluate the status of hypertensive patients.19, 20 HBP monitoring provides multiple measurements of blood pressure over a much longer period and more accurately reflects an individual’s blood pressure level, eliminates the white-coat and masked hypertension phenomena, overcomes some shortcomings of ambulatory blood pressure monitoring and avoids both observer and regression dilution biases.21, 22, 23 Importantly, it can provide information on the day-by-day variability in HBP under relatively well-controlled conditions.21, 22, 23, 24
The major goal of our study was to investigate the association of variability in systolic HBP with the progress of WMLs and cognitive impairment in the oldest old.
Methods
Study population and design
This study was performed in compliance with the ethical standards established in the Declaration of Helsinki and was approved by the Research Ethics committee of Shandong Academy of Medical Sciences. All participants provided written informed consent.
This study was a longitudinal observational study. Between April 2009 and October 2009, a total of 428 oldest old with normotension or hypertension were screened from geriatric practices and community-dwelling in areas of Shandong, China. Of these participants, 248 were eligibly recruited for this study. The exclusion criteria included stroke, dementia, schizophrenia, seizures, Parkinson’s disease, bipolar disorder, claustrophobia, secondary hypertension, end-stage heart disease, renal failure and dialysis treatment, diabetes mellitus, contraindication to MRI and inability with providing informed consent.
At baseline, each participant underwent a clinical visit to assess covariates, which included official blood pressure, history of hypertension, use of antihypertensive drugs, smoking, alcohol consumption, body mass index, education, blood lipid and glucose. Thereafter, a clinical visit was performed every 3 months. For the oldest old with hypertension, antihypertensive therapy had been advised by a cardiologist if the participant was willing to receive treatment. The antihypertensive agents included angiotensin-converting enzyme inhibitors, angiotensin II receptor blockers, calcium channel blockers, diuretics or other medication. Because our study was an observational study, there was no unified antihypertensive schedule for participants with hypertension. HBP was measured at baseline, and cognitive function and WMH were assessed at baseline and during the final follow-up visit.
Self-measured HBP
HBP was measured as previously described.25, 26 In brief, every eligible participant was supplied with an automatic device (BP3MX1-1, Microlife WatchBP Home), which was validated and satisfied the criteria of the European Society of Hypertension International Protocol.27 After 5 min of sitting at rest and with a gap of 2 min between measurements, the HBP measurement was performed in the sitting position twice each morning (0600–0900 h) and twice each evening (1700–2100 h) for 7 consecutive days. The data were excluded from the following analysis if any of the six consecutive HBP readings was invalidated.
HBP profiles were evaluated using the average of within-subject readings. Variability in systolic HBP was calculated as the coefficient of variation (CV) in serial daily systolic HBP measurements of the last 6 consecutive days. The CV was calculated as the following: CV%=s.d. of the daily systolic HBP/average of the daily systolic HBP × 100.
Assessment of MMSE
Assessment of global cognitive function was performed using the Mini-Mental State Examination (MMSE) by a neuropsychological expert who was blinded to the clinical and imaging outcomes of participants. The MMSE is a 30-point test that consists of five areas of potential cognitive impairment: orientation, registration, attention and calculation, and language. It is a validated and powerful tool for diagnosis in the advanced stages of cognitive impairment.
MRI scanning protocol and processing
Brain MRI acquisition was performed on the same 3 T GE Signa Horizon scanner (General Electric Medical Systems, Milwaukee, WI, USA) according to the same protocol. The sequences were used to image the brain as follows: a T1-weighted three-dimensional magnetization prepared rapid gradient echo sequence (isotropic 1-mm voxel, TR/TE/TI=1900/3/900 ms, flip angle 9°; acquisition matrix 256 × 256 with 160 slices yielding 1 mm3 isotropic voxels; field of view 256 × 240 mm2, 1-mm thick slices, and no gap), T2-weighted three-dimensional fast spin-echo (TR/TE=3000/98 ms, field of view=24 cm, acquisition matrix=256 × 256, number of excitations=0.5, 3-mm slice thickness and no gap), and a fluid-attenuated inversion recovery (TR/TE/TI=5000/355/1800 ms, flip angle 120°, acquisition matrix 256 × 256 with 60 slices, 2-mm thick slices and no slice gap).
WMH volume was computed from an automated subcortical and periventricular segmentation routine with T2 scan using Freesurfer.28 When the WMH was adjacent to a ventricle, the WMH was labeled as periventricular WMH; otherwise, it was deemed to be a deep WMH. The volumes of periventricular and deep WMH were calculated by summing the volumes of all of the hyperintensities detected in each area.29 The total WMH=periventricular WMH+deep WMH. The TIV (total intracranial volume) was calculated as the sum of white matter, gray matter and cerebrospinal fluid volumes using voxel-based morphometry techniques. The total volume of WMH was evaluated using a fraction of TIV as described by White:30 WMH fraction (%)=(total WMH (ml)/TIV (ml)) × 100. Volumetric analysis of the WMLs was performed using the brain extraction tool (BET) and FMFIB's automated segmentation tool (FAST) tools from the FSL 4.1 software package.31 All MRI analyses were performed by the same neuro-radiologist who blinded to clinical, laboratory and cognitive function data.
Statistical analysis
Continuous data were presented as the mean±s.d., and categorical data were expressed as percentages. As the distribution was skewed, the MMSE scores were expressed as the median and interquartile range. Paired t-tests were performed to evaluate the differences of the characteristics of all participants between the baseline and final visits. Participants were classified into three groups: low, middle and high groups, according to the tertile of CV of systolic HBP at baseline. Change percentages were used and calculated as ((value at final—value at baseline)/value at baseline) × 100. Differences in changes of the MMSE score, WMH and WMH fraction among strata in each group were assessed using one-way analysis of variance with Bonferroni procedure or Kruskal–Wallis test. The effect of CV of systolic HBP on change percentages of the MMSE score, WMH and WMH fraction were examined using a general linear model with multivariate analysis adjusted for covariates including the baseline MMSE score and baseline WMH fraction. Covariates included: age, sex, baseline body mass index, baseline official BP, baseline blood lipid and glucose, education, smoking and alcohol consumption. Statistical analysis was performed using the SPSS for Windows software package, version 17.0 (SPSS, Chicago, IL, USA). A two-tailed P<0.05 was considered statistically significant.
Results
Participants, demographic baselines and clinical characteristics
A flow diagram of the study is provided in Figure 1. Of the 248 participants, 16 were excluded for the following reasons: participants failed the brain MRI assessment during the final follow-up visit, 10 participants died and 4 participants suffered from stroke onset during an average follow-up period of 2.3 years. Finally, 232 participants completed the follow-up visit and were included in the analysis. Among these participants, 173 were females and were 59 males. There were 73 normotensives and 159 hypertensives participants. Among the hypertensive participants, 89 received antihypertensive treatment and 70 were free of antihypertensive treatment. The demographic baselines and clinical characteristics of the participants at baseline are represented in Table 1. Participants were followed for 2.3 (s.d.: 0.2) years on average. The CV of systolic HBP was 14.69±5.00% and the tertile was <12.60%, 12.60–16.47% and>16.47%.
Changes of MMSE score, periventricular WMH, deep WMH, total WMH and WMH fraction during the follow-up period
Changes in the MMSE score, periventricular WMH, deep WMH, total WMH and WMH fraction during the follow-up period are shown in Table 2. The MMSE score declined, and the periventricular WMH, deep WMH, total WMH and WMH fraction increased in all normotensive participants over the 2.3 years of follow-up. Similar changes were also observed in hypertensive patients either with anti- or non-antihypertensive treatment. There were no significant differences in the change percentages of the MMSE score, periventricular WMH, deep WMH, total WMH and WMH fraction between normotensive and hypertensive participants. The MMSE score declined, and the periventricular WMH, total WMH and WMH fraction increased in non-antihypertensive patients and were significantly greater than antihypertensive patients (P<0.05).
Effect of variability in systolic HBP on progression of cognitive impairment during the follow-up period
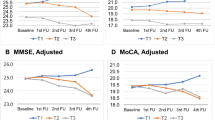
The effect of CV of systolic HBP on the change in the MMSE score during the follow-up period is shown in Figure 2. In all participants, there was an upward trend in the declined percentage of the MMSE score from the low to high group, and the differences were significant between any two groups even after adjusted for covariates, including the baseline MMSE score (P<0.05). After adjusting for covariates, including the baseline MMSE score, declined percentages of the MMSE score in the high group were significantly greater compared with those in the low group in normotensive subjects and hypertensive, antihypertensive and non-antihypertensive patients (P<0.05, respectively).
Effect of CV of systolic HBP on change percentage of the MMSE score during the follow-up period. (a) Shown as mean values with s.d.s. (b) Shown as estimated marginal mean values with 95% confidence intervals resulting from the analysis of covariance model adjusted for age, sex, the baseline body mass index, the baseline official blood pressure, the baseline blood lipid and glucose, education, smoking, alcohol consumption and the baseline MMSE score. MMSE indicates Mini-Mental State Examination. *P<0.05, compared with the Low group; †P<0.05, compared with the middle group.
Effect of variability in systolic HBP on progression of WMLs during the follow-up period
First, we determined the effect of CV of systolic HBP on the progression of total WMH and WMH fraction during the follow-up period. The change percentage of WMH is shown in Figure 3, and the change percentage of the WMH fraction is provided in Figure 4. In all participants and normotensive subjects, there was an upward trend in increased percentages of the WMH and WMH fraction from the low to high group, and the differences were significant between any two groups. After adjusting for covariates, which included the baseline WMH fraction, the trend and differences were maintained (P<0.05, respectively). In hypertensive, antihypertensive and non-antihypertensive patients, increased percentages of WMH and WMH fraction in the middle and high groups were greater than those in the low groups after adjusting for covariates, including the baseline WMH fraction (P<0.05, respectively).
Effect of CV of systolic HBP on change percentage of white matter hyperintensities during the follow-up period. (a) Shown as mean values with s.d.s. (b) Shown as estimated marginal mean values with 95% confidence intervals resulting from the analysis of covariance model adjusted for age, sex, the baseline body mass index, the baseline official blood pressure, the baseline blood lipid and glucose, education, smoking, alcohol consumption and the baseline white matter hyperintensities fraction. WMH indicates white matter hyperintensities. *P<0.05, compared with the Low group; †P<0.05, compared with the middle group.
Effect of CV of systolic HBP on change percentage of white matter hyperintensities fraction during the follow-up period. (a) Shown as mean values with s.d.s. (b) Shown as estimated marginal mean values with 95% confidence intervals resulting from the analysis of covariance model adjusted for age, sex, the baseline body mass index, the baseline official blood pressure, the baseline blood lipid and glucose, education, smoking, alcohol consumption and the baseline white matter hyperintensities fraction. WMH indicates white matter hyperintensities. *P<0.05, compared with the Low group; †P<0.05, compared with the middle group.
Next, we evaluated the effect of CV of systolic HBP on the progression of periventricular WMH during the follow-up period (Figure 5). After adjusting for covariates, including baseline periventricular WMH, there was an upward trend in increased percentages of periventricular WMH from the low to high group, and these differences were significant between any two groups in total and antihypertensive subjects (P<0.05, respectively). Increased percentages of periventricular WMH in the high group were greater than that in the low and middle groups in normotensive subjects (P<0.05). In hypertensive and non-antihypertensive patients, the increased percentages in the middle and high groups were higher than those in the low group after adjusting for covariates (P<0.05).
Effect of CV of systolic HBP on change percentage of periventricular white matter hyperintensities during the follow-up period. (a) Shown as mean values with s.d.s. (b) Shown as estimated marginal mean values with 95% confidence intervals resulting from the analysis of covariance model adjusted for age, sex, the baseline body mass index, the baseline official blood pressure, the baseline blood lipid and glucose, education, smoking, alcohol consumption and the baseline periventricular white matter hyperintensities. WMH indicates white matter hyperintensities. *P<0.05, compared with the Low group; †P<0.05, compared with the middle group.
Third, we assessed the effect of CV of systolic HBP on progression of deep WMH during the follow-up period (Figure 6). Covariates, including baseline deep WMH, were adjusted in all analyses. In all subjects, even patients who were classified into normotension, hypertension, antihypertension and non-hypertension groups, increased percentages of deep WMH in the high groups were greater compared with the low group (P<0.05, respectively).
Effect of CV of systolic HBP on change percentage of deep white matter hyperintensities during the follow-up period. (a) Shown as mean values with s.d.s. (b) Shown as estimated marginal mean values with 95% confidence intervals resulting from the analysis of covariance model adjusted for age, sex, the baseline body mass index, the baseline official blood pressure, the baseline blood lipid and glucose, education, smoking, alcohol consumption and the baseline deep white matter hyperintensities. WMH indicates white matter hyperintensities. *P<0.05, compared with the Low group; †P<0.05, compared with the middle group.
Discussion
The main finding of the present study was that a higher CV of systolic HBP was associated with a declined percentage of the MMSE score and increased percentage of periventricular WMH, deep WMH, total WMH and WMH fraction during the follow-up period in normotensive subjects, hypertensive patients, antihypertensive patients and non-antihypertensive patients. These associations were independent of mean BP, antihypertensive treatment, the baseline MMSE score and baseline WMH and other confounding factors. Our findings indicated that excessive variability in systolic HBP exacerbated the progression of cognitive impairment and WMLs in the oldest old.
Although the relationship between BP level and target organ damage is well established,32, 33 it remains unclear whether variability in BP is related to cardio- and cerebrovascular diseases.23 Schutte et al.34 reported that variability in BP did not contribute to risk stratification beyond the mean systolic BP in an unbiased general population sample. In contrast, there is increasing evidence of the association of variability in BP with target organ damage and mortality independent of mean BP.35, 36, 37, 38 The Honolulu-Asia Aging study35 revealed that higher variability in SBP in midlife significantly increased the risk of WMLs and atrophy. The Ohasama study36 demonstrated that day-to-day variability in systolic HBP is markedly associated with cognitive decline after adjusting for mean systolic HBP (odds ratio was 1.51, P=0.02). Consistent with these findings, our exploratory analyses indicated that excessive variability in systolic HBP, assessed by CV of systolic HBP, is an independent contributor to the MMSE score decline and WMH and WMH fraction increases in the oldest old independent of the classification of the participants into normotensive and hypertensive subjects, and hypertensive patients classification into patients with anti- and non-antihypertensive treatment.
Our results indicated that excessive variability in systolic HBP is a strong contributor to the progression of cognitive function decline and WML increase, including WMLs in different regions of the brain. Excessive CV of systolic HBP significantly contributed to increasing total WMH and WMH fractions, and markedly contributed to increases in periventricular and deep WMH in all subjects although they were categorized into normotension, hypertension, antihypertension and non-antihypertension groups. It may be related to dysfunction of the autonomic nervous system and advance arterial stiffness, which are common among elderly people, particularly the oldest old. Higher variability in systolic HBP, which contributes to frequent hypotension episodes, can result in cerebral hypoperfusion with consequent cerebral small vessel disease39 and hippocampal atrophy40 and accelerate cognitive impairment.41 Moreover, aggressive fluctuations of systolic blood pressure may result in hemodynamic instability in the systemic circulation and induce low or even oscillatory shear stress on the vascular wall.42, 43 These shear stresses result in vascular endothelial dysfunction and micro-cerebral vessel damage, which subsequently destroy the structure and function of the brain.42
In the present study, we found that there were no significant differences in the decreased percentages of the MMSE score and increased percentages of WMH and WMH fractions between participants with normotension and hypertension during the follow-up period. This may have occurred because the hypertensive patients included patients with antihypertensive and non-antihypertensive therapy. The results of the present study revealed that the decreased percentages of the MMSE score and increased percentages of WMH and WMH fractions in patients with non-antihypertensive therapy were significantly greater compared with patients with antihypertensive therapy.
One of the major strengths of our study is that the BP profiles were assessed using seven consecutive days of self-measured BP monitoring by participants at home. As previously described, HBP more accurately reflects an individual’s BP than the official BP, and provides variability in BP under relatively well-controlled conditions.21, 22, 23, 24, 25, 26 To the best of our knowledge, this is the first study of the effect of variability in systolic HBP on the progression of cognitive impairment and WMLs in the oldest old. Furthermore, to determine this effect, we classified the oldest old into normotensive subjects and hypertensive patients, and hypertensive patients were categorized into patients with and without antihypertensive treatment. In addition, the function, structure, and region of the WHLs in the brain were evaluated using the MMSE score, periventricular WMH, deep WMH, total WMH and WMH fractions in the present study.
However, limitations in the present study must be considered. First, all data in our study are observational in nature with known limitations. Second, this study included more females than males, which may have introduced bias in the results of analyses, as sex is a confounding factor for cognitive impairment and WMLs.44 Third, a small number of oldest old was enrolled in this study. A larger sample is needed in future studies.
Conclusions
In conclusion, excessive variability in systolic HBP exacerbates the progression of cognitive dysfunction and brain WMLs in the oldest old. Variability in systolic BP, particularly variability in systolic HBP, should be fully considered in the management of BP and daily life in the oldest old.
References
Peters R, Bekett N, Geneva M, Tzekova M, Lu FH, Poulter R, Gainsborough N, Williams B, de Vernejoul MC, Fletcher A, Bulpitt C . Sociodemographic and lifestyle risk factors for incident dementia and cognitive decline in the HYVET. Age Ageing 2009; 38: 521–527.
Peng J, Lu F, Wang Z, Zhong M, Sun L, Hu N, Liu Z, Zhang W . Excessive lowering of blood pressure is not beneficial for progression of brain white matter hyperintensive and cognitive impairment in elderly hypertensive patients: 4-year follow up study. J Am Med Dir Assoc 2014; 15: 904–910.
Mok V, Wong KK, Xiong Y, Wong A, Schmidt R, Chu W, Hu X, Leung EY, Chen S, Chen Y, Tang WK, Chen X, Ho CL, Wong KS, Wong ST . Cortical and frontal atrophy are associated with cognitive impairment in age-related confluent white-matter lesion. J Neurol Neurosurg Psychiatry 2011; 82: 52–57.
Peters R, Beckett N, Forette F, Tuomilehto J, Ritchie C, Walton I, Waldman A, Clarke R, Poulter R, Fletcher A, Bulpitt C . Vascular risk factors and cognitive function among 3763 participants in the Hypertension in the Very Elderly Trial (HYVET): a cross-sectional analysis. Int Psychogeriatr 2009; 21: 359–365.
Lobo A, Launer LJ, Fratiglioni L, Andersen K, Di Carlo A, Breteler MM, Copeland JR, Dartigues JF, Jagger C, Martinez-Lage J, Soininen H, Hofman A . Prevalence of dementia and major subtypes in Europe: a collaborative study of population-based cohorts. Neurologic Diseases in the Elderly Research Group. Neurology 2000; 54: S4–S9.
Savva GM, Wharton SB, Ince PG, Forster G, Matthews FE, Brayne C . Medical Research Council Cognitive Function and Ageing Study. Age, neuropathology, and dementia. N Engl J Med 2009; 360: 2302–2309.
Poon LW, Woodard JL, Stephen Miller L, Green R, Gearing M, Davey A, Arnold J, Martin P, Siegler IC, Nahapetyan L, Kim YS, Markesbery W . Understanding dementia prevalence among centenarians. J Gerontol A Biol Sci Med Sci 2012; 67: 358–365.
Ossenkoppele R, Jansen WJ, Rabinovici GD, Knol DL, van der Flier WM, van Berckel BN, Scheltens P, Visser PJ, Amyloid PET Study Group Verfaillie SC, Zwan MD, Adriaanse SM, Lammertsma AA, Barkhof F, Jagust WJ, Miller BL, Rosen HJ, Landau SM, Villemagne VL, Rowe CC, Lee DY, Na DL, Seo SW, Sarazin M, Roe CM, Sabri O, Barthel H, Koglin N, Hodges J, Leyton CE, Vandenberghe R, van Laere K, Drzezga A, Forster S, Grimmer T, Sánchez-Jan P, Carril JM, Mok V, Camus V, Klunk WE, Cohen AD, Meyer PT, Hellwig S, Newberg A, Frederiksen KS, Fleisher AS, Mintun MA, Wolk DA, Nordberg A, Rinne JO, Chételat G, Lleo A, Blesa R, Fortea J, Madsen K, Rodrigue KM, Brooks DJ . Prevalence of amyloid PET positivity dementia syndromes: a meta-analysis. JAMA 2015; 313: 1939–1949.
Jansen WJ, Ossenkoppele R, Knol DL, Tijms BM, Scheltens P, Verhey FR, Visser PJ, Amyloid Biomarker Study Group Aalten P, Aarsland D, Alcolea D, Alexander M, Almdahl IS, Arnold SE, Baldeiras I, Barthel H, van Berckel BN, Bibeau K, Blennow K, Brooks DJ, van Buchem MA, Camus V, Cavedo E, Chen K, Chetelat G, Cohen AD, Drzezga A, Engelborghs S, Fagan AM, Fladby T, Fleisher AS, van der Flier WM, Ford L, Förster S, Fortea J, Foskett N, Frederiksen KS, Freund-Levi Y, Frisoni GB, Froelich L, Gabryelewicz T, Gill KD, Gkatzima O, Gómez-Tortosa E, Gordon MF, Grimmer T, Hampel H, Hausner L, Hellwig S, Herukka SK, Hildebrandt H, Ishihara L, Ivanoiu A, Jagust WJ, Johannsen P, Kandimalla R, Kapaki E, Klimkowicz-Mrowiec A, Klunk WE, Köhler S, Koglin N, Kornhuber J, Kramberger MG, Van Laere K, Landau SM, Lee DY, de Leon M, Lisetti V, Lleó A, Madsen K, Maier W, Marcusson J, Mattsson N, de Mendonça A, Meulenbroek O, Meyer PT, Mintun MA, Mok V, Molinuevo JL, Møllergård HM, Morris JC, Mroczko B, Van der Mussele S, Na DL, Newberg A, Nordberg A, Nordlund A, Novak GP, Paraskevas GP, Parnetti L, Perera G, Peters O, Popp J, Prabhakar S, Rabinovici GD, Ramakers IH, Rami L, Resende de Oliveira C, Rinne JO, Rodrigue KM, Rodríguez-Rodríguez E, Roe CM, Rot U, Rowe CC, Rüther E, Sabri O, Sanchez-Juan P, Santana I, Sarazin M, Schröder J, Schütte C, Seo SW, Soetewey F, Soininen H, Spiru L, Struyfs H, Teunissen CE, Tsolaki M, Vandenberghe R, Verbeek MM, Villemagne VL, Vos SJ, van Waalwijk van Doorn LJ, Waldemar G, Wallin A, Wallin ÅK, Wiltfang J, Wolk DA, Zboch M, Zetterberg H . Prevalence of cerebral amyloid pathology in persons without dementia: a meta-analysis. JAMA 2015; 313: 1924–1938.
Debette S, Markus HS . The clinical importance of white matter hyperintensities on brain magnetic resonance imaging: systematic review and meta-analysis. BMJ 2010; 341: c3666.
Gunning-Dixon FM, Brickman AM, Cheng JC, Alexopoulos GS . Aging of cerebral white matter: a review of MRI findings. Int J Geriatr Psychiatry 2009; 24: 109–117.
Silbert LC, Dodge HH, Perkins LG, Sherbakov L, Lahna D, Erten-Lyons D, Woltjer R, Shinto L, Kaye JA . Trajectory of white matter hyperintensity burden preceding mild cognitive impairment. Neurology 2012; 79: 741–747.
Teipel SJ, Grothe M, Lista S, Toschi N, Garaci FG, Hampel H . Relevance of magnetic resonance imaging for early detection and diagnosis of Alzheimer Disease. Med Clin N Am 2013; 97: 399–424.
Frings L, Yew B, Flanagan E, Lam BYK, Hüll M, Huppertz HJ, Hodges JR, Hornberger M . Longitudinal grey and white matter changes in frontotemporal dementia and Alzheimer’s disease. PLoS ONE 2014; 9: e90814.
Barnes J, Carmichael OT, Leung KK, Schwarz C, Ridgway GR, Bartlett JW, Malone IB, Schott JM, Rossor MN, Biessels GJ, DeCarli C, Fox NC . Alzheimer’s Disease Neuroimaging Initiative. Vascular and Alzheimer’s disease markers independently predict brain atrophy rate in Alzheimer’s disease neuroimaging initiative controls. Neurobiol Aging 2013; 34: 1996–2002.
Brickman AM, Muraskin J, Zimmerman ME . Structural neuroimaging in Alzheimer’s disease: do white matter hyperintensities matter? Dialogues Clin Neurosci 2009; 11: 181–190.
Vermeer SE, Prins ND, den Heijer T, Hofman A, Koudstaal PJ, Breteler MM . Silent brain infarcts and the risk of dementia and cognitive decline. N Engl J Med 2003; 348: 1215–1222.
Wolf H, Ecke GM, Bettin S, Dietrich J, Gertz HJ . Do white matter changes contribute to the subsequent development of dementia in patients with mild cognitive impairment? A longitudinal study. Int J Geriatr Psychiatry 2000; 15: 803–812.
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Böhm M, Christiaens T, Cifkov R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Redon J, Dominiczak A, Narkiewicz K, Nilsson PM, Burnier M, Viigimaa M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Schmieder RE, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Coca A, Gillebert TC, Tendera M, Rosei EA, Ambrosioni E, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Hoes AW, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Olsen MH, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Rydén L, Sirenko Y, Stanton A, Struijker-Boudier H, Tsioufis C, van de Borne P, Vlachopoulos C, Volpe M, Wood DA . 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for themanagement of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2013; 34: 2159–2219.
Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B., Management of Arterial Hypertension of the European Society of Hypertension; European Society of Cardiology. 2007 guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2007; 25: 1105–1187.
O’Brien E, Asmar R, Beilin L, Imai Y, Mallion JM, Mancia G, Mengden T, Myers M, Padfield P, Palatini P, Parati G, Pickering T, Redon J, Staessen J, Stergiou G, Verdecchia P, . European Society of Hypertension Working Group on Blood Pressure Monitoring. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertens 2003; 21: 821–848.
Hashimoto T, Kikuya M, Ohkubo T, Satoh M, Metoki H, Inoue R, Asayama K, Kanno A, Obara T, Hirose T, Hara A, Hoshi H, Totsune K, Satoh H, Sato H, Imai Y . Home blood pressure level, blood pressure variability, smoking, and stroke risk in Japanese men: the Ohasama Study. Am J Hypertens 2012; 25: 883–891.
Stergiou GS, Ntineri A, Kollias A, Ohkubo T, Imai Y, Parati G . Blood pressure variability assessed by home measurements: a systematic review. Hypertens Res 2014; 37: 565–572.
Asayama K, Wei FF, Liu YP, Hara A, Gu YM, Schutte R, Li Y, Thijs L, Staessen JA . Does blood pressure variability contribute to risk stratification? Methodological issues and a review of outcome studies based on home blood pressure. Hypertens Res 2015; 38: 97–101.
Liu Z, Wei F, Zhao Y, Lu F, Zhang H, Diao Y, Song H, Qi Z . Day-by-day variability of self-measured blood pressure at home associated with cold pressor test norepinephrine, and heart rate variability in normotensive to moderate hypertensive. Int J Cardiol 2013; 15: 4574–4576.
Liu Z, Zhao Y, Lu F, Zhang H, Diao Y . Day-by-day variability in self-measured blood pressure at home: effects on carotid artery atherosclerosis, brachial flow-mediated dilation, and endothelin-1 in normotensive and mild-moderate hypertensive individuals. Blood Press Monit 2013; 18: 316–325.
Stergiou GS, Giovas PP, Gkinos CP, Patouras JD . Validation of the Microlife WatchBP Home device for self home blood pressure measurement according to the International Protocol. Blood Press Monit 2007; 12: 185–188.
Fischl B, Salat DH, Busa E, Albert M, Dieterich M, Haselgrove C, van der Kouwe A, Killiany R, Kennedy D, Klaveness S, Montillo A, Makris N, Rosen B, Dale AM . Whole brain segmentation: automated labeling of neuroanatomical structures in the human brain. Neuron 2002; 33: 341–355.
Godin O, Tzourio C, Mailard P, Mazoyer B, Dufouil C . Antihypertensive treatment and change in blood pressure are associated with the progression of white matter lesion volumes: the Three-City (3C)-Dijon Magnetic Resonance Imaging Study. Circulation 2011; 123: 266–273.
White WB, Wolfson L, Wakefield DB, Hall CB, Campbell P, Moscufl N, Schmidt J, Kaplan RF, Pearlson G, Guttmann CR . Average daily blood pressure, not office blood pressure, is associated with progression of cerebrovascular disease and cognitive decline in older people. Circulation 2011; 124: 2312–2319.
Jenkinson M, Beckmann CF, Behrens TE, Woolrich MW, Smith SM . Fsl. NeuroImage 2012; 62: 782–790.
Olindo S, Cabre P, Deschamps R, Chatot-Henry C, Rene-Corail P, Fournerie P, Saint-Vil M, May F, Smadja D . Acute stroke in the very elderly: epidemiological features, stroke subtypes, management, and outcome in Martinique, French West Indies. Stroke 2003; 34: 1593–1597.
Nishinaga M, Takata J, Okumiya K, Matsubayashi K, Ozawa T, Doi Y . High morning home blood pressure is associated with a loss of functional independence in the community-dwelling elderly aged 75 years or older. Hypertens Res 2005; 28: 657–663.
Schutte R, Thijs L, Liu YP, Asayama K, Jin Y, Odili A, Gu YM, Kuznetsova T, Jacobs L, Staessen JA . Within-subject blood pressure level—not variability—predicts fatal and nonfatal outcomes in a general population. Hypertension 2012; 60: 1138–1147.
Havlik RJ, Foley DJ, Sayer B, Masaki K, White L, Launer LJ . Variability in midlife systolic blood pressure is related to late-life brain white matter lesions: the Honolulu-Asia Aging study. Stroke 2002; 33: 26–30.
Matsumoto A, Satoh M, Kikuya M, Ohkubo T, Hirano M, Inoue R, Hashimoto T, Hara A, Hirose T, Obara T, Metoki H, Asayama K, Hosokawa A, Totsune K, Hoshi H, Hosokawa T, Sato H, Imai Y . Day-to-day variability in home blood pressure is associated with cognitive decline: the Ohasama study. Hypertension 2014; 63: 1333–1338.
Okada H, Fukui M, Tanaka M, Matsumoto S, Mineoka Y, Nakanishi N, Tomiyasu K, Nakano K, Hasegawa G, Nakamura N . Visit-to-visit variability in systolic blood pressure is a novel risk factor for the progression of coronary artery calcification. Hypertens Res 2013; 36: 996–999.
Yokota K, Fukuda M, Matsui Y, Hoshide S, Shimada K, Kario K . Impact of visit-to-visit variability of blood pressure on deterioration of renal function in patients with non-diabetic chronic kidney disease. Hypertens Res 2013; 36: 151–157.
Pantoni L . Cerebral small vessel disease: from pathogenesis and clinical characterisitics to therapeutic challenges. Lancet Neurol 2010; 9: 689–701.
Barnes J, Bartlett JW, van de Pol LA, Loy CT, Scahill RI, Frost C, Thompson P, Fox NC . A meta-analysis of hippocampal atrophy rates in Alzheimer’s disease. Neurobiol Aging 2009; 30: 1711–1723.
Maule S, Caserta M, Bertello C, Verhovez A, Naso D, Bisbocci D, Veglio F . Cognitive decline and low blood pressure: the other side of the coin. Clin Exp Hypertens 2008; 30: 711–719.
Cecchi E, Giglioli C, Valente S, Lazzeri C, Gensini GF, Abbate R, Mannini L . Role of hemodynamic shear stress in cardiovascular disease. Atherosclerosis 2011; 214: 249–256.
Kim KI, Lee JH, Chang HJ, Cho YS, Youn TJ, Chung WY, Chae IH, Choi DJ, Park KU, Kim CH . Association between blood pressure variability and inflammatory marker in hypertensive patients. Circ J 2008; 72: 293–298.
Li R, Cui J, Shen Y . Brain sex matters: estrogen in cognition and Alzheimer’s disease. Mol Cell Endocrinol 2014; 389: 13–21.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No. 81470489), Natural Science Foundation of Shandong Province, China (No. ZR2014HM098 and ZR2013HL041), Science and Technology Development Project of Shandong Province, China (No. 2014GSF118102) and the Medical and Health Technology Development Program of Shandong Province, China (No. 2014WS0312 and 2014WS0316).
Author contributions
Design and conduct of the study: Zhendong Liu, Yingxin Zhao, Guosheng Jiang. Data collection and analysis: Zhendong Liu, Yingxin Zhao, Hua Zhang, Qiang Chai, Yi Cui, Yutao Diao, Jianchao Xiu, Xiaolin Sun. Data interpretation and manuscript writing: Zhendong Liu, Yingxin Zhao, Hua Zhang.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Liu, Z., Zhao, Y., Zhang, H. et al. Excessive variability in systolic blood pressure that is self-measured at home exacerbates the progression of brain white matter lesions and cognitive impairment in the oldest old. Hypertens Res 39, 245–253 (2016). https://doi.org/10.1038/hr.2015.135
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2015.135
Keywords
This article is cited by
-
Blood Pressure Variability and Cognitive Function: a Scoping Review
Current Hypertension Reports (2022)
-
Diagnosis and Management of Cognitive Concerns in the Oldest-Old
Current Treatment Options in Neurology (2021)
-
Abnormal blood pressure circadian rhythms are relevant to cerebral infarction and Leukoaraiosis in hypertensive patients
BMC Neurology (2020)
-
Home-measured orthostatic hypotension associated with cerebral small vessel disease in a community-based older population
Hypertension Research (2020)
-
Day-to-day blood pressure variability is associated with lower cognitive performance among the Japanese community-dwelling oldest-old population: the SONIC study
Hypertension Research (2020)