Abstract
The possible counteracting effect of angiotensin (Ang)-converting enzyme (ACE)2/Ang-(1–7)/Mas axis against the ACE/Ang II/Ang II type 1 (AT1) receptor axis in blood pressure control has been previously described. We examined the possibility that this pathway might be involved in the anti-hypertensive effect of a newly developed AT1 receptor blocker (ARB), azilsartan, and compared azilsartan’s effects with those of another ARB, olmesartan. Transgenic mice carrying the human renin and angiotensinogen genes (hRN/hANG-Tg) were given azilsartan or olmesartan. Systolic and diastolic blood pressure, as determined by radiotelemetry, were significantly higher in hRN/hANG-Tg mice than in wild-type (WT) mice. Treatment with azilsartan or olmesartan (1 or 5 mg kg−1 per day) significantly decreased systolic and diastolic blood pressure, and the blood pressure-lowering effect of azilsartan was more marked than that of olmesartan. The urinary Na concentration decreased in an age-dependent manner in hRN/hANG-Tg mice. Administration of azilsartan or olmesartan increased urinary Na concentration, and this effect was weaker with olmesartan than with azilsartan. Azilsartan decreased ENaC-α mRNA expression in the kidney and decreased the ratio of heart to body weight. Olmesartan had a similar but less-marked effect. ACE2 mRNA expression was lower in the kidneys and hearts of hRN/hANG-Tg mice than in WT mice. This decrease in ACE2 mRNA expression was attenuated by azilsartan, but not by olmesartan. These results suggest that the hypotensive and anti-hypertrophic effects of azilsartan may involve activation of the ACE2/Ang-(1–7)/Mas axis with AT1 receptor blockade.
Similar content being viewed by others
Introduction
Recently, the counteracting effect of the angiotensin (Ang)-converting enzyme (ACE) 2/Ang-(1–7)/Mas axis against the ACE/Ang II/Ang II type 1 (AT1) receptor axis has been highlighted in studies of blood pressure regulation and organ protection.1, 2 Administration of Ang-(1–7) attenuated the development of severe hypertension and end-organ damage in spontaneously hypertensive rats treated with L-NAME.3 Giani et al.4 reported that chronic administration of Ang-(1–7) normalized arterial pressure, reduced glycemia and triglyceridemia, improved proteinuria and ameliorated structural alterations in the kidneys of stroke-prone spontaneously hypertensive rat. To further evaluate the possible counter-regulatory effects of ACE2/Ang-(1–7)/Mas on the ACE/Ang II/AT1 receptor in blood pressure control, we used transgenic mice carrying the human renin and angiotensinogen genes (hRN/hANG-Tg).5
We speculated that an increase in the Ang-(1–7) level during ACE inhibition and AT1 receptor blockade might result in Mas receptor activation and contribute to the cardioprotective and renoprotective effects.6 Moreover, it is possible that AT1 receptor blockade directly activates the ACE2/Ang-(1–7)/Mas pathway.7, 8, 9, 10 We also demonstrated that in AT1a receptor knockout mice, there was greater mRNA expression and immunostaining of ACE2 and Mas in the injured artery than in wild-type (WT) mice, with less neointimal formation.11
A newly developed AT1 receptor blocker (ARB), azilsartan, has a high binding capacity for the AT1 receptor and shows a marked hypotensive effect.12, 13 In a clinical study, azilsartan reduced blood pressure more effectively than olmesartan and valsartan in patients with stage 1 and 2 hypertension.14 Therefore, we examined the possibility that the ACE2/Ang-(1–7)/Mas axis might be involved in the anti-hypertensive effect of azilsartan and compared its effects with those of olmesartan.
Materials and methods
Animals
This study was performed in accordance with the National Institutes of Health guidelines for the use of experimental animals. All animal studies were reviewed and approved by the Animal Studies Committee of Ehime University. Ten-week-old male C57BL/6 (Clea Japan, Tokyo, Japan) and human renin (hRN-Tg; C57BL/6 background) and human angiotensinogen (hANG-Tg; C57BL/6 background) double transgenic mice (hRN/hANG-Tg) were used in this study.5 Mice were housed in a room where lighting was controlled (12 h on, 12 h off) and the temperature was kept at 24 °C. The mice were fed a standard diet (MF, Oriental Yeast, Tokyo, Japan) and water ad libitum.
Experiment 1
The blood pressure of the C57BL/6 and hRN/hANG-Tg mice was analyzed by radiotelemetry.15 Briefly, mice were anesthetized with Nembutal in saline. A midline neck incision was made, and the left common carotid artery was isolated. The telemetry probe (PA-C10; Data Sciences International, New Brighton, MN, USA) was inserted into the left common carotid artery. Ten days after implantation, blood pressure was measured. Then, hRN/hANG-Tg mice were separated into two groups receiving either 1 mg kg−1 per day of azilsartan (provided by Takeda, Tokyo, Japan) or olmesartan (Olmesartan Acid, Toronto Research Chemicals, Toronto, Ontario, Canada) in chow for 2 weeks. Two weeks after the start of treatment, the mice were given 5 mg kg−1 per day of azilsartan or olmesartan for 2 weeks. Blood pressure was measured 2 weeks after the start of administration of each ARB.
Experiment 2
Ten-week-old hRN/hANG-Tg mice were given control chow or chow containing one of two different doses (1 or 5 mg kg−1 per day) of azilsartan or olmesartan for 4 weeks. Urine samples were obtained before the start of treatment, and 2 and 4 weeks later by using metabolic cages (3600M021, Tecniplast, Tokyo, Japan), and the urinary Na concentration was determined (DRI-CHEM 7000 V, FUJIFILM, Tokyo, Japan). Kidney and heart samples were obtained 4 weeks after the start of treatment.
Real-time reverse transcriptase-PCR
Kidney and heart samples were frozen in liquid nitrogen and stored at −80 °C until analysis. Total mRNA was extracted from heart and kidney samples with Sepasol-RNA I Super G (Nacalai Tesque, Kyoto, Japan). Quantitative real-time reverse transcriptase-PCR was performed with a SYBR green kit (MJ Research, Waltham, MA, USA). The PCR primers were as follows: 5′-TCAACCAGGCCCCCTGCAATCA-3′ (forward) and 5′-GCTCTGTGCGCAGTGTCAGGG-3′ (reverse) for ENaC-α and 5′-TGTGTCTGATGTCATTCCTAGAAGT-3′ (forward) and 5′-AGGCTGGTAAGGTGGCTCAAG-3′ (reverse) for ACE2.
Ang-(1–7) treatment
A telemetry transmitter was implanted in hRN/hANG-Tg mice. Ten days after implantation, blood pressure was measured and the hRN/hANG-Tg mice were given 5 mg kg−1 per day Ang-(1–7) (4332, Peptide Institute, Osaka, Japan) via an osmotic mini-pump (model 1004, Alzet, Cupertino, CA, USA). Blood pressure was measured 2 weeks after the onset of treatment.
Statistical analysis
All values are expressed as mean±s.e.m. in the text and figures. Blood pressure response data were analyzed by two-way repeated measures analysis of variance with a Bonferroni multiple comparison post-test. All other data were evaluated by one-way analysis of variance followed by post hoc analysis for multiple comparisons.
Results
Blood pressure
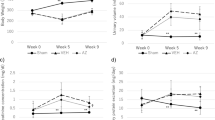
The systolic and diastolic blood pressure in hRN/hANG-Tg mice were significantly higher than in WT mice (Figure 1). Treatment with azilsartan or olmesartan (1 or 5 mg kg−1 per day) significantly decreased systolic and diastolic blood pressure, and the blood pressure-lowering effect of azilsartan was more marked than that of olmesartan (Figures 1a and b). Treatment with azilsartan or olmesartan at a dose of 10 mg kg−1 per day did not increase the blood pressure-lowering effect when compared with the effects of the 5 mg kg−1 per day dose (data not shown). There were no differences in heart rate between the two groups (Supplementary Figure 1).
Urinary Na concentration
The urinary Na concentration decreased in an age-dependent manner in hRN/hANG-Tg mice when compared with WT mice (Figure 2a). Administration of azilsartan or olmesartan increased the urinary Na concentration compared with that of untreated hRN/hANG-Tg mice 2 and 4 weeks after the start of treatment, and the effect of 1 mg kg−1 per day of olmesartan was weaker than the effect of the same dose of azilsartan (Figure 2a). The expression of ENaC-α mRNA in the kidneys of hRN/hANG-Tg mice did not differ from that seen in WT mice (Figure 2b). Administration of azilsartan significantly decreased ENaC-α mRNA expression compared with untreated hRN/hANG-Tg mice. In contrast, olmesartan treatment slightly decreased ENaC-α mRNA expression; however, this effect was not significant.
Effect of azilsartan or olmesartan on urinary Na excretion in hRN/hANG-Tg mice before and after 2 and 4 weeks of administration (a). Effect of azilsartan or olmesartan on expression of ENaC-α mRNA in the kidneys of hRN/hANG-Tg mice after 4 weeks of administration (b). n=6 for each group. *P<0.05 vs WT mice. †P<0.05 vs untreated hRN/hANG-Tg mice. ‡P<0.01 vs untreated hRN/hANG-Tg mice.
Cardiac hypertrophy
The ratio of heart to body weight in hRN/hANG-Tg mice was greater than in WT mice (Figure 3). Treatment with azilsartan at a dose of 1 or 5 mg kg−1 per day decreased the ratio of heart to body weight compared with the untreated hRN/hANG-Tg mice; however, the same dose of olmesartan did not decrease this ratio.
Expression of ACE2 mRNA
The expression of ACE2 mRNA in the kidneys and hearts of hRN/hANG-Tg mice was lower than in WT mice (Figures 4a and b). These decreases in ACE2 mRNA expression were attenuated by azilsartan; however, olmesartan did not have this effect.
Effect of Ang-(1–7) administration on blood pressure
Administration of 5 mg kg−1 per day Ang-(1–7) via an osmotic mini-pump significantly decreased systolic and diastolic blood pressure (Supplementary Figure 2).
Discussion
Transgenic mice carrying the hRN/hANG-Tg had higher blood pressures and lower urinary Na concentration and expression of ACE2 mRNA in the kidney than did WT mice. Treatment with azilsartan significantly decreased systolic and diastolic blood pressure and increased urinary Na concentration and ACE2 mRNA expression in the kidney with a decrease in ENaC-α mRNA expression in the kidney. At each dose, these effects of azilsartan were more marked than the effects of olmesartan. These results suggest that the hypotensive effects of azilsartan may involve activation of the ACE2/Ang-(1–7)/Mas axis with AT1 receptor blockade.
Activation of the Ang II/AT1 receptor is pivotal in increasing blood pressure due to Na reabsorption in the kidney. Crowley et al.16, 17 reported that expression of Ang II in the kidney induces hypertension, possibly by promoting Na reabsorption. Moreover, Mamenko et al.18 reported that Ang II activates ENaC and that this effect was additive to the effect of aldosterone.
Consistent with these results, we demonstrated that urinary Na concentration was lower in hRN/hANG-Tg mice than in WT mice, and that this decrease was attenuated by treatment with ARBs.
Accumulating evidence suggests that the ACE2/Ang-(1–7)/Mas pathway in the kidney has a role in blood pressure control. In the Goldblatt hypertension rat, an Ang-(1–7) antagonist or ACE2 inhibitor increased blood pressure and kidney damage.19 It has been reported that the ACE2/ACE ratio is higher in the normal kidney than in the hypertensive nephropathy.8 AT1 receptor stimulation decreases the expression of ACE2 and increases that of ACE in the kidney. We observed that ACE2 mRNA expression in the kidneys of hRN/hANG-Tg mice was lower than in WT mice, and treatment with azilsartan increased ACE2 mRNA and decreased ENaC-α mRNA. However, these effects were not observed with olmesartan treatment at a dose of 1 or 5 mg kg−1 per day, suggesting that the anti-hypertensive effect of azilsartan in hRN/hANG-Tg mice might be partially due to changes in ACE2 and ENaC-α expression. ENaC has an important role in the control of blood pressure. Loss-of-function mutations in ENaC lead to type 1 pseudohypoaldosteronism and cause hypotension, whereas-gain-of function mutations lead to Liddle syndrome and cause hypertension;20, 21 this suggests that the decrease in the expression of ENaC-α caused by azilsartan could be partially responsible for its ability to lower blood pressure.
It has been reported that ARB treatment attenuates cardiac remodeling after myocardial infarction and increases plasma Ang-(1–7).22, 23 Ferrario et al.24 also reported that blockage of RAS by an ACE inhibitor or ARB increases cardiac Ang-(1–7), ACE2 mRNA and ACE2 activity. In cardiac myocytes, ACE2 activity and mRNA expression are decreased by AngII treatment. However, this decrease is attenuated by cotreatment with the ARB losartan.10 We have also reported that ACE2-deficient mice have cardiac hypertrophy compared with WT mice at the age of 10 weeks.25 hRN/hANG-Tg mice demonstrated cardiac hypertrophy and reduced expression of ACE2 mRNA. This cardiac hypertrophy and ACE2 mRNA reduction were attenuated by treatment with azilsartan and were associated with an increase in ACE2; however, this effect was not observed with olmesartan, suggesting that this effect of azilsartan in hRN/hANG-Tg mice might be partially due to activation of the ACE2/Ang-(1–7)/Mas pathway. It is also possible that the blood pressure differences between mice treated with azilsartan or olmesartan could influence ENaC-α mRNA expression, cardiac hypertrophy and ACE2 mRNA expression.
In conclusion, our results demonstrate that azilsartan inhibits the blood pressure increase and cardiac hypertrophy with increased kidney and heart ACE2 that are seen in transgenic mice carrying both the hRN/hANG-Tg, suggesting that these effects of azilsartan might be in part due to activation of the ACE2/Ang-(1–7)/Mas axis. The same inhibitory effects of olmesartan were less marked in this mouse strain, although olmesartan is known to inhibit vascular remodeling, cardiac hypertrophy and renal damage, involving activation of the ACE2/Ang-(1–7)/Mas pathway.7, 9, 11, 26, 27 Our previous report also demonstrated that treatment with olmesartan prevented a cuff-injury-induced decrease in ACE2 expression in femoral arteries.11 Although the detailed mechanism is yet to be investigated, this apparent discrepancy might be because a different mouse model other than the cuff-injury model was used. Moreover, the antagonistic properties of azilsartan against AT1 receptor blockade could be involved12 because hRN/hANG-Tg mice overproduce Ang II associated with exaggerated AT1 receptor activation. In contrast, Varagic et al.28 recently reported that Ang-(1–7) does not mediate the long-term effects of olmesartan on blood pressure through Mas in addition to counterbalancing renin release in response to AT1 receptor blockade. The Ang II-mediated ACE2 reduction is known to be regulated by the extracellular signal-regulated kinase (ERK) 1/ERK2/phosphatase pathway and/or the ERK/p38 mitogen-activated protein kinase pathway.8, 9 However, it is difficult to explain the different increases in ACE2 mRNA that were induced by azilsartan and olmesartan based only on their effects on the mitogen-activated protein kinase pathway. Further investigation will reveal the pathophysiological role of the ACE2/Ang-(1–7)/Mas axis in blood pressure control and contribute to the discussion of further possible drug effects of ARBs beyond their class effect.
References
Ferreira AJ, Santos RA, Bradford CN, Mecca AP, Sumners C, Katovich MJ, Raizada MK . Therapeutic implications of the vasoprotective axis of the renin-angiotensin system in cardiovascular diseases. Hypertension 2010; 55: 207–213.
Passos-Silva DG, Verano-Braga T, Santos RA . Angiotensin-(1–7): beyond the cardio-renal actions. Clin Sci (Lond) 2013; 124: 443–456.
Benter IF, Yousif MH, Anim JT, Cojocel C, Diz DI . Angiotensin-(1–7) prevents development of severe hypertension and end-organ damage in spontaneously hypertensive rats treated with L-NAME. Am J Physiol Heart Circ Physiol 2006; 290: H684–H691.
Giani JF, Muñoz MC, Pons RA, Cao G, Toblli JE, Turyn D, Dominici FP . Angiotensin-(1–7) reduces proteinuria and diminishes structural damage in renal tissue of stroke-prone spontaneously hypertensive rats. Am J Physiol Renal Physiol 2011; 300: F272–F282.
Fukamizu A, Sugimura K, Takimoto E, Sugiyama F, Seo MS, Takahashi S, Hatae T, Kajiwara N, Yagami K, Murakami K . Chimeric renin-angiotensin system demonstrates sustained increase in blood pressure of transgenic mice carrying both human renin and human angiotensinogen genes. J Biol Chem 1993; 268: 11617–11621.
Sevá Pessôa B, van der Lubbe N, Verdonk K, Roks AJ, Hoorn EJ, Danser AH . Key developments in renin-angiotensin-aldosterone system inhibition. Nat Rev Nephrol 2013; 9: 26–36.
Igase M, Strawn WB, Gallagher PE, Geary RL, Ferrario CM . Angiotensin II AT1 receptors regulate ACE2 and angiotensin-(1–7) expression in the aorta of spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 2005; 289: H1013–H1019.
Koka V, Huang XR, Chung AC, Wang W, Truong LD, Lan HY . Angiotensin II up-regulates angiotensin I-converting enzyme (ACE), but down-regulates ACE2 via the AT1-ERK/p38 MAP kinase pathway. Am J Pathol 2008; 172: 1174–1183.
Gallagher PE, Ferrario CM, Tallant EA . MAP kinase/phosphatase pathway mediates the regulation of ACE2 by angiotensin peptides. Am J Physiol Cell Physiol 2008; 295: C1169–C1174.
Gallagher PE, Ferrario CM, Tallant EA . Regulation of ACE2 in cardiac myocytes and fibroblasts. Am J Physiol Heart Circ Physiol 2008; 295: H2373–H2379.
Iwai M, Nakaoka H, Senba I, Kanno H, Moritani T, Horiuchi M . Possible involvement of angiotensin-converting enzyme 2 and Mas activation in inhibitory effects of angiotensin II Type 1 receptor blockade on vascular remodeling. Hypertension 2012; 60: 137–144.
Ojima M, Igata H, Tanaka M, Sakamoto H, Kuroita T, Kohara Y, Kubo K, Fuse H, Imura Y, Kusumoto K, Nagaya H . In vitro antagonistic properties of a new angiotensin type 1 receptor blocker, azilsartan, in receptor binding and function studies. J Pharmacol Exp Ther 2011; 336: 801–808.
Bönner G, Bakris GL, Sica D, Weber MA, White WB, Perez A, Cao C, Handley A, Kupfer S . Antihypertensive efficacy of the angiotensin receptor blocker azilsartan medoxomil compared with the angiotensin-converting enzyme inhibitor ramipril. J Hum Hypertens 2013; 27: 479–486.
White WB, Weber MA, Sica D, Bakris GL, Perez A, Cao C, Kupfer S . Effects of the angiotensin receptor blocker azilsartan medoxomil versus olmesartan and valsartan on ambulatory and clinic blood pressure in patients with stages 1 and 2 hypertension. Hypertension 2011; 57: 413–420.
Mills PA, Huetteman DA, Brockway BP, Zwiers LM, Gelsema AJ, Schwartz RS, Kramer K . A new method for measurement of blood pressure, heart rate, and activity in the mouse by radiotelemetry. J Appl Physiol 2000; 88: 1537–1544.
Crowley SD, Gurley SB, Herrera MJ, Ruiz P, Griffiths R, Kumar AP, Kim HS, Smithies O, Le TH, Coffman TM . Angiotensin II causes hypertension and cardiac hypertrophy through its receptor in the kidney. Proc Natl Acad Sci USA 2006; 103: 17985–17990.
Crowley SD, Zhang J, Herrera M, Griffiths R, Ruiz P, Coffman TM . Role of AT1 receptor-mediated salt retention in angiotensin II-dependent hypertension. Am J Physiol Renal Physiol 2011; 301: F1124–F1130.
Mamenko M, Zaika O, Ilatovskaya DV, Staruschenko A, Pochynyuk O . Angiotensin II increases activity of the epithelial Na+ channel (ENaC) in distal nephron additively to aldosterone. J Biol Chem 2012; 287: 660–671.
Bürgelová M, Vanourková Z, Thumová M, Dvorák P, Opocenský M, Kramer HJ, Zelízko M, Malý J, Bader M, Cervenka L . Impairment of the angiotensin-converting enzyme 2-angiotensin-(1–7)-Mas axis contributes to the acceleration of two-kidney, one-clip Goldblatt hypertension. J Hypertens 2009; 27: 1988–2000.
Shimkets RA, Warnock DG, Bositis CM, Nelson-Williams C, Hansson JH, Schambelan M, Gill JR, Ulick S, Milora RV, Findling JW, Canessa CM, Rossier BC, Lifton RP . Liddle’s syndrome: heritable human hypertension caused by mutations in the beta subunit of the epithelial sodium channel. Cell 1994; 79: 407–414.
Chang SS, Grunder S, Hanukoglu A, Rosler A, Mathew PM, Hanukoglu I, Schild L, Lu Y, Shimkets RA, Nelson-Williams C, Rossier BC, Lifton RP . Mutations in subunits of the epithelial sodium channel cause salt wasting with hyperkalaemic acidosis, pseudohypoaldosteronism type 1. Nat Genet 1996; 12: 248–253.
Ishiyama Y, Gallagher PE, Averill DB, Tallant EA, Brosnihan KB, Ferrario CM . Upregulation of angiotensin-converting enzyme 2 after myocardial infarction by blockade of angiotensin II receptors. Hypertension 2004; 43: 970–976.
Burchill LJ, Velkoska E, Dean RG, Griggs K, Patel SK, Burrell LM . Combination renin-angiotensin system blockade and angiotensin-converting enzyme 2 in experimental myocardial infarction: implications for future therapeutic directions. Clin Sci (Lond) 2012; 123: 649–658.
Ferrario CM, Jessup J, Chappell MC, Averill DB, Brosnihan KB, Tallant EA, Diz DI, Gallagher PE . Effect of angiotensin-converting enzyme inhibition and angiotensin II receptor blockers on cardiac angiotensin-converting enzyme 2. Circulation 2005; 111: 2605–2610.
Moritani T, Iwai M, Kanno H, Nakaoka H, Iwanami J, Higaki T, Ishii E, Horiuchi M . ACE2 deficiency induced perivascular fibrosis and cardiac hypertrophy during postnatal development in mice. J Am Soc Hypertens 2013; 7: 259–266.
Inaba S, Iwai M, Furuno M, Kanno H, Senba I, Okayama H, Mogi M, Higaki J, Horiuchi M . Role of angiotensin-converting enzyme 2 in cardiac hypertrophy induced by nitric oxide synthase inhibition. J Hypertens 2011; 29: 2236–2245.
Shiota A, Yamamoto K, Ohishi M, Tatara Y, Ohnishi M, Maekawa Y, Iwamoto Y, Takeda M, Rakugi H . Loss of ACE2 accelerates time-dependent glomerular and tubulointerstitial damage in streptozotocin-induced diabetic mice. Hypertens Res 2010; 33: 298–307.
Varagic J, Ahmad S, VonCannon JL, Moniwa N, Brosnihan KB, Wysocki J, Batlle D, Ferrario CM . Predominance of AT(1) blockade over mas-mediated angiotensin-(1–7) mechanisms in the regulation of blood pressure and renin-angiotensin system in mRen2.Lewis rats. Am J Hypertens 2013; 26: 583–590.
Acknowledgements
This study was supported by JSPS KAKENHI Grant Numbers 25293310 (MH), 25462220 (MM) and 24791506 (JI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
MH received research support and lecturing fees from Takeda Pharmaceutical Company Ltd. The remaining authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Hypertension Research website
Supplementary information
Rights and permissions
About this article
Cite this article
Iwanami, J., Mogi, M., Tsukuda, K. et al. Role of angiotensin-converting enzyme 2/angiotensin-(1–7)/Mas axis in the hypotensive effect of azilsartan. Hypertens Res 37, 616–620 (2014). https://doi.org/10.1038/hr.2014.49
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.49
Keywords
This article is cited by
-
Overexpression of angiotensin-converting enzyme 2 by renin-angiotensin system inhibitors. Truth or myth? A systematic review of animal studies
Hypertension Research (2021)
-
Tissue-specific expression of the SARS-CoV-2 receptor, angiotensin-converting enzyme 2, in mouse models of chronic kidney disease
Scientific Reports (2021)
-
Improved pharmacokinetics and bone tissue accumulation of Angiotensin-(1–7) peptide through bisphosphonate conjugation
Amino Acids (2021)
-
Interactions of coronaviruses with ACE2, angiotensin II, and RAS inhibitors—lessons from available evidence and insights into COVID-19
Hypertension Research (2020)
-
Antihypertensive effect of azilsartan versus olmesartan in patients with essential hypertension: a meta-analysis
Irish Journal of Medical Science (1971 -) (2019)