Abstract
Reactive oxygen species (ROS) and antioxidant enzymes are required to maintain homeostasis. The loss of this balance can cause excessive ROS production and damage to the cardiovascular tissues. Angiotensin II receptor blockers (ARBs) and β-blockers with antioxidant effects may inhibit ROS in the cardiovascular system. In this study, we directly compared the effects of ARBs and β-blockers with antioxidant properties on cardiovascular protection and the regulation of endothelial progenitor cell (EPC) numbers in the setting of oxidative stress in hypertensive rats. To compare the effects of the drugs, animals were divided into the following groups: Wistar-Kyoto rats (WKY), untreated spontaneously hypertensive rats (SHR) and SHR treated with tempol (TEMP, 5 mg kg−1 per day), trichlorothiazide (TCTZ, 1.6 mg kg−1 per day), atenolol (25 mg kg−1 per day), nebivolol (NEBL, 5 mg kg−1 per day), carvedilol (CVDL, 30 mg kg−1 per day) or telmisartan (TERT, 5 mg kg−1 per day). Following 2 weeks of treatment, blood pressures (BPs) and aortic wall thicknesses were similarly reduced in each antihypertensive drug-treated group. Superoxide anion and malondialdehyde levels were significantly reduced following treatment with NEBL, CVDL and TERT. Additionally, the expression levels of NADPH oxidase subunits were also reduced in the TERT-, CVDL- and NEBL-treated groups. Furthermore, these drugs improved both EPC numbers and the expression levels of peroxiredoxin 2 (Prdx2), an antioxidant enzyme, in the heart and kidneys but not the aorta. Cardiac Prdx2 expression, in particular, was markedly improved by TERT, NEBL and CVDL treatment, and renal Prdx2 expression was enhanced by TEMP. Our data indicate that short-term treatment with TERT may have more beneficial effects on cardiovascular protection, EPC number improvements and Prdx2 expression compared with CVDL and NEBL. In conclusion, TERT may positively modulate the balance between oxidative stress and antioxidant properties and demonstrate capabilities beyond its BP-lowering effects.
Similar content being viewed by others
Introduction
Reactive oxygen species (ROS) have an important role in the progression of multiple diseases, including hypertension, atherosclerosis, diabetes and stroke.1 NADPH oxidase is an important source of ROS in the setting of hypertension. It consists of several subunits, including p22phox, p47phox and gp91phox (also termed ‘NOX2’, homologous to Mox1 in rodents).2 ROS production and intracellular antioxidant enzyme activity are balanced under normal conditions. However, if this balance is disrupted, ROS can cause intracellular damage, which requires antioxidant enzymes for recovery.3 The most prominent intracellular antioxidant enzymes are superoxide dismutase, catalase, glutathione peroxidase and peroxiredoxin (Prdx). Prdx was recently discovered and is an important H2O2 scavenger. Furthermore, several reports indicate that Prdx reduces apoptosis and improves renal and cardiac cell survival rates.4,5 Nevertheless, the relationship between Prdx and antihypertensive drugs remains unclear.
Regenerating damaged vascular endothelial cells following injury is extremely difficult; however, endothelial progenitor cells (EPCs) partially improve the regeneration of damaged vessels through their differentiation.6,7 Unfortunately, EPC numbers are significantly reduced in hypertensive patients.8 Therefore, therapeutic agents that restore the ability of EPCs to regenerate damaged vessels are necessary to treat hypertensive patients.
Elevated ROS levels in hypertension are caused by multiple molecular mechanisms.9 Among these, angiotensin II (Ang II) mediates excessive ROS production via the activation of NADPH oxidase, which is downstream of the Ang II type 1 receptor.10 Ang II receptor blockers (ARBs) enhance cardiovascular protection and prevent cardiovascular oxidation through Ang II type 1 receptor antagonism. Losartan and candesartan reduce cardiovascular oxidation and improve EPC functionality by reducing oxidative stress.11,12 Furthermore, some β-blockers have also been shown to enhance cardiovascular protection, diminish oxidative stress and recover EPC functionality in hypertension. For example, celiprolol, a β-blocker with antioxidant properties, reduced cardiovascular oxidation and improved the functional regulation of EPCs in salt-loaded spontaneously hypertensive rats (SHR).13 However, despite the beneficial effects of these antihypertensive agents, there are no data showing direct comparisons between ARBs and β-blockers with antioxidant properties regarding their effects on cardiovascular oxidation and EPC numbers.
The aim of this study was to directly compare telmisartan (TERT, ARB), carvedilol (CVDL) and nebivolol (NEBL) (β-blockers with antioxidant properties) in SHR to understand their effects on cardiovascular oxidation, EPC numbers and antioxidant enzyme expression.
Methods
Experimental animals
Experimental animal studies were approved by the Institutional Animal Care and Use Committees (IACUC) of the Catholic University of the Korea School of Medicine (CUMC-2008-0038-02).
Eight-week-old Wistar-Kyoto (WKY) rats (n=6) and age-matched SHR (n=63) were purchased through Central Laboratory Animal. (SLC Japan authorized company in Korea, Seoul, South Korea). WKY rats were used for the normal control group. Untreated SHR (SHR, n=9) were used for the hypertensive control group and were administered normal saline orally. Randomly selected SHR were divided according to the type of antihypertensive drug they received as follows: CVDL (n=9, 30 mg kg−1 per day, Roche, GmBh, Germany); NEBL (n=9, 5 mg kg−1 per day, GlaxoSmithKline, Brentford, UK); and TERT (n=9, 5 mg kg−1 per day, GlaxoSmithKline). Atenolol (ATEL, n=9, 25 mg kg−1 per day, Sigma-Aldrich, St Louis, MO, USA) was used to compare the antioxidant properties of the β-blockers, a group that includes CVDL and NEBL. Trichlorothiazide (TCTZ, n=9, 1.6 mg kg−1 per day, Apotex, Toronto, ON, Canada) was administered to compare its antihypertensive effects with those of other drugs. Furthermore, tempol (TEMP, n=9, 5 mg kg−1 per day, Sigma-Aldrich) was administered to compare the antioxidant effects of all drugs. Drug doses were based on previously published literature values.14,15 All drugs were administered orally for 14 days.
Hemodynamic measurements
Following drug treatments, blood pressure (BP; systolic BP and diastolic BP) and heart rate (HR) were measured using a BP-2000 BP analysis system (Visitech Systems, Apex, NC, USA), which was modified as previously described.16
Animals were incubated in warming chambers at 37 °C for stability, and the BP and HR of each animal were measured between 15 and 20 times. Selected results (n=10) were used for statistical analyses.
Preparation of tissue samples
For analysis, experimental animals were sacrificed under anesthesia using tiletamine and zolazepam (tiletamine, 18.8 mg kg−1; zolazepam, 18.8 mg kg−1; Zoletile 50, Virbac Laboratories, Carros, France). Heparin sodium solution (1 U g−1, Sigma-Aldrich) was subcutaneously injected into each animal to prevent blood clotting. Heart, aorta and kidney tissues were isolated after 30 min.
Excised tissue samples were divided into two pieces. One piece was embedded in optimal cutting temperature (OCT) freezing media (Tissue-Tek, Sakura Finetek USA, Torrance, CA, USA) and stored in a deep freezer. The other was stored in liquid nitrogen until the conclusion of the experimental analysis.
Analysis of oxidative stress in tissues
Dehydroethidium (DHE) staining
Frozen tissue samples were cut into 5-μm sections using a cryo microtome. Samples were subsequently washed with 1x phosphate-buffered saline (PBS) for 10 min before being stained with 2 μm DHE (Molecular Probe, Eugene, OR, USA) solution for 1 h at 37 °C. They were then transferred into a humidity chamber kept at 4 °C in order to stop the reaction. Sections were incubated with 4′,6-diamidino-2-phenylindole (5 μg ml−1, Sigma-Aldrich) for 10 min and mounted with crystal-mounting solution cover glasses. Fluorescence images were taken using an Axiovert 200 fluorescence microscope (Zeiss, Göttingen, Germany).
Thiobarbituric acid reactive substance assay
Stored samples were immediately homogenized using liquid nitrogen and were resuspended with 1x PBS to obtain the following concentrations: heart=50 mg ml−1, aorta=20 mg ml−1 and kidney=50 mg ml−1. Tissue samples (100 μl) were mixed with 100 μl sodium dodecyl sulfate solution, to which 2.5 ml of thiobarbituric acid/buffer reagent was added. The samples were covered with either glass marble or a cap and incubated at 95 °C for 1 h.Samples were then cooled to room temperature in an ice bath for 10 min. The samples were centrifuged at 3000 r.p.m. for 20 min, and the supernatant was removed from the samples for fluorescence analysis with an excitation of 530 nm and an emission of 550 nm.
Immunofluorescence staining of NADPH oxidase subunits and antioxidant enzymes
The expression patterns of the NADPH oxidase subunits (p22phox (Santa Cruz, CA, USA) p47phox (Santa Cruz) and Mox1 (gp91phox homologous in rodent, Santa Cruz) and antioxidant enzymes (Prdx1 and 2 (Ab frontier, Seoul, South Korea)) were confirmed via immunofluorescence staining.
Sectioned tissue samples (thickness: 5 μm) were washed with 1x PBS, and fixed with 4% formalin solution for 10 min. Sections were then blocked with 1.5% normal horse serum for 30 min at room temperature. Primary antibodies (p22phox, p47phox, Mox1, Prdx1 and 2) were conjugated overnight in a humidity chamber at 4 °C. An anti-mouse Alexa 568 secondary antibody (Molecular Probe, Eugene, OR, USA) was used to visualize the primary antibody. Nuclei were stained using 4′,6-diamidino-2-phenylindole, and cover slips were mounted using crystal-mounting solution. Fluorescence images were taken using an Axiovert 200 fluorescence microscope.
EPC colony-forming unit hills analysis
EPCs were isolated from peripheral blood (PB) and bone marrow (BM). PB was collected from the left renal artery, and BM was isolated from the tibia and femur. PB- and BM-EPCs were isolated with Histopaque 1083 (Sigma-Aldrich) using gradient centrifugation (1800 r.p.m. for 30 min at room temperature). Isolated PB- and BM-EPCs were transferred into fresh collecting tubes, washed twice with 1x PBS, and suspended in endothelial growth media-2 (EGM-2: endothelial basal medium containing 10% FBS and endothelial growth factors, Cambrex, Walkersville, MD, USA).
PB- and BM-EPCs were seeded in 24-well culture plates at a density of 5x104 cells per well, and colonies were generated 7 to 10 days after seeding. EPC colony-forming unit hills were randomly counted using an inverted microscope.
EPC characterization
Isolated EPCs were confirmed via acetylated low-density lipoprotein uptake and UEA-1 lectin binding assays. The 24-well plates were gently washed with 1x PBS. Acetylated low-density lipoprotein (Molecular Probes) was diluted 1:100 with EBM-2, and 500 μl acetylated low-density lipoprotein solution was sprayed on each well. The plates were then incubated at 37 °C and 5% CO2 in a humidity chamber for 4 h. After the uptake reaction was finished, each well was carefully washed with PBS and loaded with UEA-1 lectin (Sigma-Aldrich) diluted in PBS (1:50). Following lectin binding, each well was washed with PBS, and nuclei were stained using 4′,6-diamidino-2-phenylindole. Images were taken using an Axiovert fluorescence microscope.
Statistical analysis
Fluorescence densities were measured using Image J software (free software, http://rsbweb.nih.gov/ij/index.html), and data were presented after normalization with the control group (WKY group). Results were expressed as the means±s.e.m. Comparisons between two groups were confirmed using the unpaired Student's t-test. Data were considered statistically significant if corresponding P-values were <0.05.
Results
TEMP, NEBL and CVDL elicited similar reductions in BP
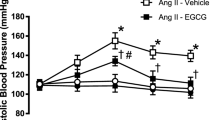
Systolic BP and diastolic BP were each higher in SHR than in WKY rats (P<0.01, Figure 1a). Antihypertensive drug treatments alleviated the elevated systolic BP and diastolic BP to similar extents (P<0.01). Interestingly, systolic BP and diastolic BP were also reduced following treatment with TEMP (P<0.01).
Hemodynamic analyses performed by measuring blood pressure (a, systolic and diastolic blood pressure) and heart rate (b). *P<0.01 vs. WKY and #P<0.01 vs. SHR. ATEL, SHR treated with atenolol; CVDL, SHR treated with carvedilol; NEBL, SHR treated with nebivolol; SHR, Spontaneously hypertensive rats; TCTZ, SHR treated with trichlorothiazide; TEMP, SHR treated with tempol; TERT, SHR treated with telmisartan; WKY, Wistar-Kyoto Rat.
HRs were higher in SHR than in WKY rats (P<0.01, Figure 1b). However, treatment with ATEL, NEBL and CVDL reduced HRs (P<0.01). Nevertheless, no changes in HR were observed following treatment with either TCTZ or TERT (P>0.05).
TEMP, NEBL and CVDL reduced aortic wall thicknesses
Anatomical analyses were performed by measuring aortic wall thicknesses (Figure 2a). Aortic walls were thicker in SHR than in WKY rats (P<0.01, Figure 2b). Wall thicknesses were similarly ameliorated following treatment with each experimental drug (P<0.01), with the exception of TEMP (P>0.05).
Anatomical analyses showed by histological findings of aortic wall thickness (a) and bar graph (b). *P<0.01 vs. WKY and #P<0.01 vs. SHR. ATEL, SHR treated with atenolol; CVDL, SHR treated with carvedilol; NEBL, SHR treated with nebivolol; SHR, Spontaneously hypertensive rats; TCTZ, SHR treated with trichlorothiazide; TEMP, SHR treated with tempol; TERT, SHR treated with telmisartan; WKY, Wistar-Kyoto Rat. A full color version of this figure is available at the Hypertension Research journal online.
TEMP, NEBL and CVDL each improved EPC numbers following order
EPC characterization was performed via acetylated low-density lipoprotein uptake and UEA-1 lectin binding assays (Figure 3a). In PB- and BM-EPCs, the numbers of EPC hills were lower in SHR than in WKY rats (Figures 3b–e). Each experimental drug treatment significantly increased EPC colony-forming unit hill numbers as follows: TERT>NEBL>CVDL>TEMP>ATEL=TCTZ (P<0.01).
EPC-colony forming units (CFU) hills assays were confirmed using Ac-LDL uptake and UEA-1 lectin binding assays (a). EPCs were isolated from peripheral blood (PB) and bone marrow (BM), and colonies were generated 7 to 10 days following isolation (b and c). For statistical analysis, the numbers of EPC-CFU hills were calculated in each group (d and e). *P<0.01 vs. SHR and ##P<0.01 vs. SHR. ATEL, SHR treated with atenolol; CVDL, SHR treated with carvedilol; NEBL, SHR treated with nebivolol; SHR, Spontaneously hypertensive rats; TCTZ, SHR treated with trichlorothiazide; TEMP, SHR treated with tempol; TERT, SHR treated with telmisartan; WKY, Wistar-Kyoto Rat. A full color version of this figure is available at the Hypertension Research journal online.
TERT, followed by CVDL and NEBL, ameliorated superoxide anion levels and malondialdehyde (MDA) concentrations
In heart
Tissue superoxide anion levels were confirmed using DHE staining (Figure 4a). The fluorescence intensities of DHE were higher in SHR than in WKY rats (P<0.01, Figure 4b). Each experimental drug treatment improved these intensities.
Tissue superoxide anion levels were measured using dehydroethidium (DHE) staining (a). Fluorescence intensities were presented as bar graphs, and relative optical intensities were normalized to WKY (b – d). Tissue malondialdehyde (MDA) concentrations were measured using a thiobarbituric acid reactive substance assay (TBARS assay, e,f). *P<0.01 vs. WKY, #P<0.05 vs. SHR and ##P<0.01 vs. SHR. ATEL, SHR treated with atenolol; CVDL, SHR treated with carvedilol; NEBL, SHR treated with nebivolol; SHR, Spontaneously hypertensive rats; TCTZ, SHR treated with trichlorothiazide; TEMP, SHR treated with tempol; TERT, SHR treated with telmisartan; WKY, Wistar-Kyoto Rat. A full color version of this figure is available at the Hypertension Research journal online.
MDA concentrations were higher in SHR than in WKY rats (P<0.01, Figure 4e). The increased MDA levels were attenuated following treatment with TERT, CVDL, NEBL and TEMP (P<0.01).
In aorta
DHE fluorescence intensities were higher in SHR than in WKY rats (P<0.01, Figure 4c). Each experimental drug reduced the intensities of DHE after 14 days (P<0.01). However, there were some differences in DHE fluorescence intensities following drug treatments. TERT was the most effective drug, and CVDL and TEMP elicited greater improvements than did NEBL, ATEL or TCTZ (P<0.01).
MDA concentrations were significantly higher in SHR than in WKY rats (P<0.01, Figure 4f). MDA levels were significantly attenuated by treatment with TERT, followed by CVDL, NEBL and TEMP (P<0.01).
In kidney
The intensities of DHE fluorescence were higher in SHR than in WKY rats (P<0.01, Figure 4d). The intensities were attenuated following treatment with TERT, CVDL, NEBL, TEMP and ATEL. However, the intensities were unchanged following TCTZ treatment.
MDA concentrations were also higher in SHR than in WKY rats (Figure 4g). These concentrations were significantly reduced by each experimental drug. TERT was the most effective drug, followed by CVDL, NEBL, TEMP, ATEL and TCTZ (P<0.01).
TERT and antioxidant β-blockers attenuated NADPH oxidase subunit expression
In heart
NADPH oxidase subunit (p22phox, p47phox and Mox1) levels were higher in SHR than in WKY rats (P<0.01, Figures 5a–c). Three NADPH oxidase subunits were attenuated following treatment with each experimental drug. However, the effects of these drugs were diverse. Among the drugs, TERT and CVDL significantly attenuated subunit levels (P<0.01). Following drug treatment, the expression levels of both p22phox and p47phox were lower than that of Mox1.
The expression of NAPDH oxidase subunits was measured via immunofluorescence staining using p22phox, p47phox and Mox1 specific antibodies in heart (a – c), aorta (d – f) and kidneys (g – i). Furthermore, the expression of peroxiredoxin 2 was analyzed via immunofluorescence staining in heart, aorta and kidneys (j– l). *P<0.01 vs. WKY, #P<0.05 vs. SHR and ##P<0.01 vs. SHR. ATEL, SHR treated with atenolol; CVDL, SHR treated with carvedilol; NEBL, SHR treated with nebivolol; SHR, Spontaneously hypertensive rats; TCTZ, SHR treated with trichlorothiazide; TEMP, SHR treated with tempol; TERT, SHR treated with telmisartan; WKY, Wistar-Kyoto Rat.
In aorta
The expression of aortic-NADPH oxidase subunits was higher in SHR than WKY rats (P<0.01, Figures 5d–f). The levels of p22phox and p47phox were significantly decreased, whereas only a slight decrease was observed in the level of Mox1. Furthermore, the expression levels of p22phox and Mox1 were improved most significantly by TERT treatment, followed by CVDL, TEMP, NEBL, ATEL and TCTZ. However, p47phox levels improved most significantly following treatment with TEMP, as opposed to CVDL.
In kidney
NADPH oxidase subunit levels were higher in SHR than in WKY rats (P<0.01, Figures 5g–i). Furthermore, p22phox and p47phox expression levels were significantly attenuated in the TERT- and CVDL-treated groups (P<0.01). However, the TEMP-, TCTZ- and ATEL-treated groups exhibited no changes in the levels of each of the three subunits.
Antioxidant β-blockers and ARBs increase Prdx2 expression in heart and kidneys
The expression levels of the endogenous antioxidant enzymes, Prdx1 and Prdx 2, were determined via immunofluorescence (Figures 5j–l). Unfortunately, Prdx1 was not detected in any of the experimental groups in this study (data not shown).
Prdx2 expression was significantly lower in heart and kidneys of SHR than in heart and kidneys of WKY rats (P<0.01). However, Prdx2 expression was not changed in the aortic tissues of SHR compared with WKY rats (P>0.05). In SHR, attenuated cardiac and renal Prdx2 expression levels improved following treatment with TERT, NEBL, CVDL, TEMP (P<0.01) and ATEL (heart, P<0.05 and kidney, P<0.01). Treatment with TERT, NEBL and CVDL, in particular, nearly restored Prdx2 expression to normal levels in heart. Furthermore, TEMP treatment improved Prdx2 expression such that levels approached those observed in WKY kidneys. However, attenuated cardiac and renal Prdx2 expression levels did not improve following treatment with TCTZ in SHR (P>0.05).
Discussion
Several antihypertensive drugs, such as β-blockers with antioxidant effects and ARBs, decrease ROS levels in the cardiovascular system. Valsartan and CVDL suppressed ROS production in mononuclear cells, and irbesartan reduced superoxide anion levels and lipid peroxidation in patients with coronary artery disease.17, 18, 19 These findings indicate that some antihypertensive drugs reduce ROS levels; however, no direct comparisons among these drugs had been performed previously. Our data indicated that TERT had superior antioxidant effects on the cardiovascular system compared with antioxidant β-blockers such as CVDL and NEBL.
A balance between ROS formation and antioxidant enzyme activity is required for homeostasis. Loss of this balance causes excessive ROS production by multiple mechanisms.20 Excessive ROS production leads to cardiovascular diseases, including atherosclerosis, congestive heart failure and hypertension.21 ROS affects multiple intracellular targets, including the mitogen-activated protein kinase family, the cell survival kinase family, Akt, Ras/Rac, c-Src, protein kinase C and tyrosine phosphatases.22 To date, researchers have attempted to devise a means of reducing oxidative stress via molecular and pharmacological approaches. Antioxidants restore the functions damaged by ROS in vitro; however, this ability had not been tested in clinical trials.23 The aim of this study was to investigate EPC numbers and the balance between ROS and antioxidants following antihypertensive drug treatments in a hypertensive animal model.
In the hypertension model, BPs and aortic wall thicknesses improved following treatment with olmesartan, an ARB, and TERT.24,25 Additionally, each of our experimental drugs, with the exception of TEMP, ameliorated BPs and aortic wall thicknesses similarly following short-term treatment.
In hypertension, vascular function deteriorates, thereby affecting the cardiovascular system. EPCs have a role in the regeneration of damaged endothelial cells by differentiating and secreting cytokines and growth factors within the vessel.26,27 Circulating EPC functions were restored following treatment with ARBs, suggesting that blocking the Ang II type 1 receptor is a novel therapeutic strategy for enhancing EPC function.11,12 Our observations indicate that both ARB and β-blockers with antioxidant effects restored the numbers of circulating and BM derived EPCs.
The superoxide anion is an important member of the ROS family and induces tissue lipid peroxidation by converting into the hydroxyl radical. Lipid peroxidation results in accelerated tissue oxidative stress and triggers the onset of vascular disease, including atherosclerosis.28 Treatment with losartan and celiprolol reduced MDA concentrations in two separate studies.11,13 We also observed that superoxide anion levels and MDA concentrations were attenuated following treatment with TERT, CVDL and NEBL in a simultaneous comparison study.
ROS are produced by several sources, including NADPH oxidase, xanthine oxidase and cytochrome p450. Among these sources, NADPH oxidase is the most prominent source of ROS in the setting of hypertension due to its ability to activate Ang II. The expression of NADPH oxidase components is tissue-type specific. NADPH oxidase subunit expression is greater in heart than in kidneys.29 However, Ang II expression is higher in kidneys than in heart.30 NADPH oxidase consists of many subunits, such as membrane bound cytochrome b558 (p22phox and gp91phox) and cytosolic activating factors (p47phox and p67phox).1 NADPH oxidase subunits are expressed at higher levels in SHR than in normotensive rats.2 We also found that the expression of NADPH oxidase subunits (p22phox, p47phox and Mox1 (homolog of gp91phox)) in heart, aorta and kidneys was increased in SHR compared with WKY rats. Some studies have shown that treatment with NEBL prevents both increases in NADPH oxidase subunit expression and superoxide anion formation.31 We found that NADPH oxidase subunit expression was reduced following treatment with TERT, CVDL and NEBL in heart and aorta. In the kidneys, CVDL and TERT treatment significantly attenuated NADPH oxidase subunit levels, particularly p47phox and p22phox. p22phox behaves as a stabilizer, and p47phox behaves as an organizer and is an important NADPH oxidase subunit. Suppression of both subunits via pharmacological approaches reduces ROS production. The development of NADPH oxidase subunit inhibitors is currently in progress.32 Recent molecular studies regarding the control of NADPH oxidase subunit expression as a means of reducing ROS levels remain ongoing. p47phox-deficient mice and gp91phox knockout mice are characterized by reduced superoxide anion production. p22phox siRNA rats attenuate NADPH oxidase activity, ROS formation and BP elevation.1 It may be useful to administer commercially available antihypertensive drugs with antioxidant properties to hypertensive patients until a means of regulating NADPH oxidase subunits is found.
The relationship between BP and oxidative stress has caused great controversy. Some groups have suggested that antioxidants may reduce BP. By contrast, others have not found a connection between BP and oxidative stress. It has been reported that TERT exerts antioxidant and cardioprotective effects independent of its BP-lowering effects.25 In our study, ARBs and antioxidant β-blockers, particularly TERT, controlled BP and inhibited oxidative stress. However, we could not elucidate the relationship between oxidative stress and BP.
Our study showed that TERT exerted superior antioxidant effects on the cardiovascular system compared with CVDL and NEBL. TERT regulates oxidative stress in the cardiovascular system by several mechanisms. TERT is characterized by the combined properties of ARBs and partial PPAR-γ agonists. The PPAR-γ pathway is involved in many cellular functions, including oxidative stress regulation. In vascular smooth muscle cells, PPAR-γ attenuates Ang II type 1 receptor gene expression, thereby inactivating the NADPH oxidase complex and decreasing the ROS generation.33 Other reports indicate that TERT stimulates the production of endothelial nitric oxide synthase via the PPAR-γ pathway. Endothelial nitric oxide synthase produces nitric oxide, which interacts with superoxide and affects vascular pathophysiology.34 These reports demonstrated that TERT is involved in many pathways by which it regulates the balance between oxidative stress and antioxidant effects.
NEBL provided cardiovascular protection by reducing oxidative stress and augmenting nitric oxide bioavailability through the scavenging of ROS. NEBL is a racemic mixture containing equal amounts of two isomers, d-NEBL and l-NEBL.35 Furthermore, NEBL has β1-blocking properties. NEBL inhibits NADPH oxidase activity in various models of hypertension. However, the molecular mechanisms by which NEBL reduces oxidative stress are not well understood.36,37
CVDL possesses ROS-scavenging and ROS-suppressive properties. Short-term treatment with CVDL attenuates ROS generation by a way of polymorphonuclear leukocytes and mononuclear cells. CVDL treatment also reduces the level of 4-hydroxy-2-nonenal, a major lipid peroxidation product and source of oxidative stress.17,38,39
Mammalian cells are equipped with intrinsic antioxidant enzymes such as catalase, glutathione peroxidase and superoxide dismutase. The recently discovered antioxidant, Prdx, exists in six isoforms that reduce tissue lipid peroxidation by scavenging hydrogen peroxide. The six subclasses of Prdx have different cellular localizations. For example, Prdx1, 2, 4, 5 and 6 localize to the cytosol, whereas Prdx3 and 5 are found in mitochondria, and Prdx2 exists in the membrane.40 A large amount of research has been devoted to determining the functions of Prdx. Prdx2 protects cortical neurons in the setting of ischemic brain injury and neurodegenerative conditions.41 Prdx subclasses are abundant in the normal heart, where they are highly expressed and exert protective effects against oxidative stress. Prdx also protects against apoptosis and necrosis in cardiomyocytes. In kidney podocytes, the upregulation of Prdx2 expression reduces apoptosis and increases cell survival.4,5 These results indicate that Prdx2 is related to cell survival in kidneys and heart. To the best of our knowledge, our study is the first to evaluate the relationship between antihypertensive drugs and Prdx. We found that Prdx2 expression levels were significantly improved following treatment with TERT, NEBL, CVDL and TEMP in heart and kidneys of SHR. The TERT, CVDL and NEBL treatment groups, in particular, almost completely restored the levels of Prdx2 to normal in heart. In kidneys, TEMP treatment restored Prdx2 levels close to those of WKY rats. These results showed that antihypertensive drugs with antioxidant properties improve Prdx2 levels in heart and kidneys. We observed that the Prdx2 expression levels in aortic tissue were unchanged when these tissues were treated with TERT, CVDL and NEBL. However, others have demonstrated that Prdx2 is strongly associated with vascular homeostasis.42 In the future, further study will be necessary to understand the correlation between Prdx2 and antihypertensive drugs.
ARBs and vasodilating β-blockers with antioxidant properties have several important clinical applications. CVDL is a nonselective β/α-1 blocker indicated in the treatment of diseases ranging from hypertension to systolic heart failure. NEBL is a β1-receptor blocker with nitric oxide-potentiating vasodilatory effects used in the treatment of hypertension and senile systolic heart failure. CVDL and NEBL reduced the mortality rates of patients with heart failure.43 According to the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial (ONTARGET) clinical study, TERT appears to have a promising role in protecting high-risk patients against cardiovascular disease.44 According to our data, TERT, CVDL and NBEL may have other mechanisms by which they are involved in cardiovascular protection, beyond their BP-lowering effects.
Our study had several limitations. First, we studied subjects during a 2-week treatment period, as opposed to studying them for a longer period of time. Furthermore, our study did not measure outcome data, such as survival rates. Our sample size was relatively small and featured nine rats in each group. Finally, there were no data comparing different ARBs.
Our results showed that vasodilating β-blockers with antioxidant effects (CVDL and NEBL) and ARB (TERT) improved EPCs numbers, cardiovascular protection and the expression of antioxidant, Prdx2, in addition to lowering the BPs of SHR. We suggest that TERT, rather than CVDL and NEBL, may positively modulate the balance between oxidative stress and antioxidant properties, in addition to its BP-lowering effects.
References
Sedeek M, Hebert RL, Kennedy CR, Burns KD, Touyz RM . Molecular mechanisms of hypertension: role of Nox family NADPH oxidases. Curr Opin Nephrol Hypertens 2009; 18: 122–127.
Paravicini TM, Touyz RM . NADPH oxidases, reactive oxygen species, and hypertension: clinical implications and therapeutic possibilities. Diabetes Care 2008; 31: S170–S180.
Yao EH, Yu Y, Fukuda N . Oxidative stress on progenitor and stem cells in cardiovascular diseases. Curr Pharm Biotechnol 2006; 7: 101–108.
Hsu HH, Hoffmann S, Di Marco GS, Endlich N, Peter-Katalinic J, Weide T, Pavenstadt H . Downregulation of the antioxidant protein peroxiredoxin 2 contributes to angiotensin II-mediated podocyte apoptosis. Kidney Int 2011; 80: 959–969.
Zhao W, Fan GC, Zhang ZG, Bandyopadhyay A, Zhou X, Kranias EG . Protection of peroxiredoxin II on oxidative stress-induced cardiomyocyte death and apoptosis. Basic Res Cardiol 2009; 104: 377–389.
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T, Witzenbichler B, Schatteman G, Isner JM . Isolation of putative progenitor endothelial cells for angiogenesis. Science 1997; 275: 964–967.
Ishikawa M, Asahara T . Endothelial progenitor cell culture for vascular regeneration. Stem Cells Dev 2004; 13: 344–349.
Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, Finkel T . Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. New Engl J Med 2003; 348: 593–600.
Berry C, Brosnan MJ, Fennell J, Hamilton CA, Dominiczak AF . Oxidative stress and vascular damage in hypertension. Curr Opin Nephrol Hypertens 2001; 10: 247–255.
Garrido AM, Griendling KK . NADPH oxidases and angiotensin II receptor signaling. Mol Cell Endocrinol 2009; 302: 148–158.
Yao EH, Fukuda N, Matsumoto T, Kobayashi N, Katakawa M, Yamamoto C, Tsunemi A, Suzuki R, Ueno T, Matsumoto K . Losartan improves the impaired function of endothelial progenitor cells in hypertension via an antioxidant effect. Hypertens Res 2007; 30: 1119–1128.
Yu Y, Fukuda N, Yao EH, Matsumoto T, Kobayashi N, Suzuki R, Tahira Y, Ueno T, Matsumoto K . Effects of an ARB on endothelial progenitor cell function and cardiovascular oxidation in hypertension. Am J Hypertens 2008; 21: 72–77.
Yao EH, Fukuda N, Matsumoto T, Katakawa M, Yamamoto C, Han Y, Ueno T, Kobayashi N, Matsumoto K . Effects of the antioxidative beta-blocker celiprolol on endothelial progenitor cells in hypertensive rats. Am J Hypertens 2008; 21: 1062–1068.
Gorska D, Dudarewicz M, Czarnecka E, Andrzejczak D . Does nebivolol influence serum concentrations of proinflammatory cytokines in hypertensive (SHR) and normotensive (WKY) rats? Pharmacol Rep 2010; 62: 86–94.
Dai Q, Xu M, Yao M, Sun B . Angiotensin AT1 receptor antagonists exert anti-inflammatory effects in spontaneously hypertensive rats. Br J Pharmacol 2007; 152: 1042–1048.
Krege JH, Hodgin JB, Hagaman JR, Smithies O . A noninvasive computerized tail-cuff system for measuring blood pressure in mice. Hypertension 1995; 25: 1111–1115.
Dandona P, Karne R, Ghanim H, Hamouda W, Aljada A, Magsino CH Jr . Carvedilol inhibits reactive oxygen species generation by leukocytes and oxidative damage to amino acids. Circulation 2000; 101: 122–124.
Dandona P, Kumar V, Aljada A, Ghanim H, Syed T, Hofmayer D, Mohanty P, Tripathy D, Garg R . Angiotensin II receptor blocker valsartan suppresses reactive oxygen species generation in leukocytes, nuclear factor-kappa B, in mononuclear cells of normal subjects: evidence of an antiinflammatory action. J Clin Endocrinol Metab 2003; 88: 4496–4501.
Khan BV, Navalkar S, Khan QA, Rahman ST, Parthasarathy S . Irbesartan, an angiotensin type 1 receptor inhibitor, regulates the vascular oxidative state in patients with coronary artery disease. J Am Coll Cardiol 2001; 38: 1662–1667.
Fearon IM, Faux SP . Oxidative stress and cardiovascular disease: novel tools give (free) radical insight. J Mol Cell Cardiol 2009; 47: 372–381.
Sugamura K, Keaney JF Jr . Reactive oxygen species in cardiovascular disease. Free Radic Biol Med 2011; 51: 978–992.
Nickenig G, Harrison DG . The AT(1)-type angiotensin receptor in oxidative stress and atherogenesis: part I: oxidative stress and atherogenesis. Circulation 2002; 105: 393–396.
Hamilton CA, Miller WH, Al-Benna S, Brosnan MJ, Drummond RD, McBride MW, Dominiczak AF . Strategies to reduce oxidative stress in cardiovascular disease. Clin Sci (Lond) 2004; 106: 219–234.
Paulis L, Becker ST, Lucht K, Schwengel K, Slavic S, Kaschina E, Thone-Reineke C, Dahlof B, Baulmann J, Unger T, Steckelings UM . Direct angiotensin II type 2 receptor stimulation in Nomega-nitro-L-arginine-methyl ester-induced hypertension: the effect on pulse wave velocity and aortic remodeling. Hypertension 2012; 59: 485–492.
Goyal S, Arora S, Mittal R, Joshi S, Nag TC, Ray R, Kumari S, Arya DS . Myocardial salvaging effect of telmisartan in experimental model of myocardial infarction. Eur J Pharmacol 2009; 619: 75–84.
Watson T, Goon PK, Lip GY . Endothelial progenitor cells, endothelial dysfunction, inflammation, and oxidative stress in hypertension. Antioxid Redox Signal 2008; 10: 1079–1088.
Imanishi T, Hano T, Nishio I . Angiotensin II accelerates endothelial progenitor cell senescence through induction of oxidative stress. J Hypertens 2005; 23: 97–104.
Giustarini D, Dalle-Donne I, Tsikas D, Rossi R . Oxidative stress and human diseases: Origin, link, measurement, mechanisms, and biomarkers. Crit Rev Clin Lab Sci 2009; 46: 241–281.
Lei S, Liu Y, Liu H, Yu H, Wang H, Xia Z . Effects of N-acetylcysteine on nicotinamide dinucleotide phosphate oxidase activation and antioxidant status in heart, lung, liver and kidney in streptozotocin-induced diabetic rats. Yonsei Med J 2012; 53: 294–303.
Navar LG, Nishiyama A . Why are angiotensin concentrations so high in the kidney? Curr Opin Nephrol Hypertens 2004; 13: 107–115.
Oelze M, Daiber A, Brandes RP, Hortmann M, Wenzel P, Hink U, Schulz E, Mollnau H, von Sandersleben A, Kleschyov AL, Mulsch A, Li H, Forstermann U, Munzel T . Nebivolol inhibits superoxide formation by NADPH oxidase and endothelial dysfunction in angiotensin II-treated rats. Hypertension 2006; 48: 677–684.
Drummond GR, Selemidis S, Griendling KK, Sobey CG . Combating oxidative stress in vascular disease: NADPH oxidases as therapeutic targets. Nat Rev Drug Discov 2011; 10: 453–471.
Takeda K, Ichiki T, Tokunou T, Funakoshi Y, Iino N, Hirano K, Kanaide H, Takeshita A . Peroxisome proliferator-activated receptor gamma activators downregulate angiotensin II type 1 receptor in vascular smooth muscle cells. Circulation 2000; 102: 1834–1839.
Kobayashi N, Ohno T, Yoshida K, Fukushima H, Mamada Y, Nomura M, Hirata H, Machida Y, Shinoda M, Suzuki N, Matsuoka H . Cardioprotective mechanism of telmisartan via PPAR-gamma-eNOS pathway in dahl salt-sensitive hypertensive rats. Am J Hypertens 2008; 21: 576–581.
Toblli JE, DiGennaro F, Giani JF, Dominici FP . Nebivolol: impact on cardiac and endothelial function and clinical utility. Vasc Health Risk Manag 2012; 8: 151–160.
Mason RP, Kubant R, Jacob RF, Walter MF, Boychuk B, Malinski T . Effect of nebivolol on endothelial nitric oxide and peroxynitrite release in hypertensive animals: Role of antioxidant activity. J Cardiovasc Pharmacol 2006; 48: 862–869.
Whaley-Connell A, Habibi J, Johnson M, Tilmon R, Rehmer N, Rehmer J, Wiedmeyer C, Ferrario CM, Sowers JR . Nebivolol reduces proteinuria and renal NADPH oxidase-generated reactive oxygen species in the transgenic Ren2 rat. Am J Nephrol 2009; 30: 354–360.
Dandona P, Ghanim H, Brooks DP . Antioxidant activity of carvedilol in cardiovascular disease. J Hypertens 2007; 25: 731–741.
Nakamura K, Kusano K, Nakamura Y, Kakishita M, Ohta K, Nagase S, Yamamoto M, Miyaji K, Saito H, Morita H, Emori T, Matsubara H, Toyokuni S, Ohe T . Carvedilol decreases elevated oxidative stress in human failing myocardium. Circulation 2002; 105: 2867–2871.
Wood ZA, Schroder E, Robin Harris J, Poole LB . Structure, mechanism and regulation of peroxiredoxins. Trends Biochem Sci 2003; 28: 32–40.
Schroder E, Brennan JP, Eaton P . Cardiac peroxiredoxins undergo complex modifications during cardiac oxidant stress. Am J Physiol Heart Circ Physiol 2008; 295: H425–H433.
Choi MH, Lee IK, Kim GW, Kim BU, Han YH, Yu DY, Park HS, Kim KY, Lee JS, Choi C, Bae YS, Lee BI, Rhee SG, Kang SW . Regulation of PDGF signalling and vascular remodelling by peroxiredoxin II. Nature 2005; 435: 347–353.
Chatterjee S, Biondi-Zoccai G, Abbate A, D'Ascenzo F, Castagno D, Van Tassell B, Mukherjee D, Lichstein E . Benefits of beta blockers in patients with heart failure and reduced ejection fraction: network meta-analysis. Br Med J 2013; 346: f55.
Investigators O. Investigators O Yusuf S, Investigators O Teo KK, Investigators O Pogue J, Investigators O Dyal L, Investigators O Copland I, Investigators O Schumacher H, Investigators O Dagenais G, Investigators O Sleight P, Investigators O Anderson C . Telmisartan, ramipril, or both in patients at high risk for vascular events. New Engl J Med 2008; 358: 1547–1559.
Acknowledgements
This study was supported by a Grant from the Korean Health Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI13C1256).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yoo, S., Choi, S., Jung, M. et al. Short-term use of telmisartan attenuates oxidation and improves Prdx2 expression more than antioxidant β-blockers in the cardiovascular systems of spontaneously hypertensive rats. Hypertens Res 38, 106–115 (2015). https://doi.org/10.1038/hr.2014.151
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/hr.2014.151
Keywords
This article is cited by
-
Serum Malondialdehyde Levels in Hypertensive Patients: A Non-invasive Marker of Oxidative Stress. A Systematic Review and Meta-analysis
High Blood Pressure & Cardiovascular Prevention (2022)
-
Telmisartan protects chronic intermittent hypoxic mice via modulating cardiac renin-angiotensin system activity
BMC Cardiovascular Disorders (2018)
-
Modulation of cardiac stem cell characteristics by metoprolol in hypertensive heart disease
Hypertension Research (2018)
-
Vascular structural and functional changes: their association with causality in hypertension: models, remodeling and relevance
Hypertension Research (2017)
-
EPA:DHA 6:1 prevents angiotensin II-induced hypertension and endothelial dysfunction in rats: role of NADPH oxidase- and COX-derived oxidative stress
Hypertension Research (2017)