Abstract
Purpose
The purpose of the study was to audit the use of non-contact ultra-widefield retinal imaging in infants with suspected abusive head trauma (AHT) using the Optos P200MA Scanning Laser Ophthalmoscope.
Patients and methods
A retrospective, observational case series. Ten eyes of five consecutive infants (aged 1–15 months) with suspected (or in 1 case, known) AHT referred for an ophthalmological opinion were included. Each infant underwent non-contact ultra-widefield retinal imaging using the Optos P200MA scanning laser ophthalmoscope. Optos fundus fluorescein angiography (FFA) was performed in one infant with oral sedation. The other four infants did not require sedation. The main outcome measure was the acquisition of a single, definitive ultra-widefield retinal image in each eye. Safety was audited by determining adverse changes in heart rate and oxygen saturations that required cessation of imaging.
Results
The Optos P200MA ultra-widefield scanning laser ophthalmoscope acquired good quality retinal images in all infants. Documentation of acute, widespread retinal haemorrhages contributed to a diagnosis of AHT in three infants. Chronic pre-macular haemorrhage and macular schisis were documented by FFA in a fourth infant. The absence of retinal haemorrhages was documented in a fifth infant contributing to the exclusion of a diagnosis of AHT. There were no adverse safety signals in any infant in this series.
Conclusion
The Optos P200MA ultra-widefield scanning laser ophthalmoscope appears safe to use in infants with suspected AHT, providing high-quality retinal images in a single frame without ocular contact. Optos P200MA may be used as alternative to RetCam to document retinal haemorrhages in stable infants with suspected AHT.
Similar content being viewed by others
Introduction
Abusive head trauma (AHT)—also known as shaken baby syndrome—is the commonest cause of traumatic death in infancy.1 It is associated with a 30% mortality, with a further 30% of infants suffering severe neurological sequelae.2 AHT typically presents with an acute unexplained encephalopathy, intracranial haemorrhage (characteristically subdural), and retinal haemorrhages. Exclusion, by full investigation, of congenital or acquired coagulopathies and other masquerading organic disorders2 is mandatory. The diagnosis of AHT is imperative, to ensure safeguarding of the infant, protection of any siblings and initiation of social services and police investigations.
The detection of retinal haemorrhages is central to the diagnosis of AHT.3 The appearance, distribution, laterality, and severity of haemorrhages will assist in objectively distinguishing between accidental and non-accidental causes of head injury in infancy.1
Because of the child protection measures and legal proceedings initiated by a diagnosis of AHT, high-quality photo-documentation of the retinal appearance in cases of suspected AHT is critical. The diagnosis of AHT is likely to be challenged in Court and high-quality retinal images provide objective evidence of any abnormalities. Because some superficial retinal haemorrhages in AHT may resolve over a period of days, accurate documentation is required as soon as possible after admission. Photographs also enable the retinal complications of AHT such as pre-macular haemorrhage and macular schisis to be documented to determine the necessity and timing of any potential intervention.
RetCam (Pleasanton, CA, USA) has become established for retinal imaging in infants with suspected AHT.4 The RetCam is a portable device that requires coupling fluid and ocular contact to acquire retinal images on a supine infant. Sedation may be required for RetCam imaging in some cases, especially if retinal angiography is required.5 Series evaluating the utility of the RetCam imaging system in AHT are often undertaken on paediatric intensive care units where infants are sedated or ventilated,4 although many series do not explicitly state whether sedation was used on RetCam imaging in this patient group.6, 7 The RetCam is able to image a 130° field, typically requiring 10–12 montaged retinal images to record the combined appearance of both eyes. RetCam imaging is the current ‘gold standard’ method of documentation.
When our Retcam was not available in the ophthalmology outpatient facility, we started using the Optos P200MA Scanning Laser Ophthalmoscope (Optos, Dunfermline, UK), which has been demonstrated to attain high-quality retinal images in infants with retinopathy of prematurity (ROP),8, 9 incontinentia pigmenti,10 and other paediatric retinal disorders11 without the need for ocular contact. Optos captures a 200° retinal field enabling documentation of the retinal periphery in a single image, typically without the need for sedation.
We present a series of four infants presenting with suspected AHT, in whom ultra-widefield retinal photographs were acquired using the Optos P200MA Scanning Laser Ophthalmoscope. We describe the Optos imaging technique in infants, present ultra-widefield images, and illustrate their impact on patient management. We outline the relative advantages of Optos and RetCam in the context of retinal imaging of infants with suspected AHT. We demonstrate the utility of fundus fluorescein angiography (FFA) in the evaluation of retinal pathology in a fifth infant who had sustained AHT some weeks earlier. This audit was undertaken to evaluate the safety of this imaging modality in infants with suspected AHT.
Materials and methods
Patients
Four consecutive infants with suspected AHT were referred to the paediatric ophthalmology service at the Oxford Eye Hospital, UK between November 2013 and December 2014 for retinal examination and photography. Another infant, diagnosed with AHT elsewhere was referred for a surgical opinion. Infants were aged between 1 and 15 months, four were male and one female. The audit protocol was approved by the clinical governance committee of the Oxford Eye Hospital (Registration number: 210416-NOTSS-YUSUF). All imaging was performed with the full informed consent of the parents, and in adherence with the tenets of the Declaration of Helsinki.
Retinal imaging protocol
Retinal photographs were acquired using the Optos P200MA Scanning Laser Ophthalmoscope in each infant as previously described.8, 9, 10, 11 Mydriasis was achieved with topical phenylephrine 2.5% and cyclopentolate 0.5%. Topical proxymetacaine 0.5% was instilled into each eye followed by insertion of a paediatric Lieberman speculum to part the eyelids, secured to the temple with Micropore tape. A peripheral oxygen saturation probe monitored heart rate and peripheral capillary oxygen saturation with a paediatric neonatal nurse present, trained in neonatal resuscitation. The infant was held in the ‘flying baby position’ with the infants trunk supported by the forearm, chin supported by the hand, with the contralateral hand placed on the occiput for stability. A physiological saline solution was applied intermittently to the ocular surface to maintain a clear cornea. The infant was manoeuvred to the camera’s aperture and fine adjustments were made by the imaging technician using an image capture control. Pseudo-colour fundal images were acquired from both eyes, taking <5 min in each case. Ultra-widefield fluorescein angiography was performed in one infant following peripheral venous cannulation. Ten percent sodium fluorescein was injected at a dose of 0.1 mg/kg, with images acquired from both eyes at regular time intervals with early phase images acquired on the right eye and late phases in both eyes. No infants required cessation of image acquisition due to reduced oxygen saturation or altered cardiovascular parameters. Optos fundus images are presented in pseudo colour, balanced from green and red laser images.
Results
Case 1
A 2-month-old male infant had been admitted to the paediatric high-dependency unit with unexplained facial soft tissue injuries, apnoea, and a nuchal rash. General examination revealed hypertonia with brisk reflexes. Neuroimaging revealed bilateral acute subdural haematomas with subarachnoid blood. Dilated retinal examination demonstrated a symmetrical distribution of over 100 retinal haemorrhages in each eye concentrated at the posterior pole, extending to the retinal periphery. The optic discs appeared unremarkable. Ultra-widefield colour images were acquired without sedation (Figure 1). A diagnosis of AHT was made. Three weeks later, the eyes were convergent with reduced abduction and visual responsiveness. Dilated fundoscopy revealed resolution of retinal haemorrhages.
Case 2
A 4-week-old male infant presented with a left parieto-occipital fluctuant swelling measuring 4 × 5.5 cm without discoloration. The child was born at 39 weeks gestation by caesarean section following abandoned forceps delivery. Scalp electrodes were used but vacuum-assisted delivery was not attempted. No clear explanation for the swelling was apparent, although the child had been vomiting. Computerised tomography (CT) imaging of the brain revealed a shallow left parieto-occipital sub-galeal fluid collection but no intracranial abnormalities. A paediatric ophthalmology consult was requested. Ultra-widefield colour images were acquired without sedation, documenting the absence of retinal haemorrhages to the retinal periphery (Figure 2). AHT was subsequently excluded; radiological skeletal survey and extended clotting screen were unremarkable and the sub-galeal collection resolved on repeat neuroimaging.
Case 3
A 4-month-old male infant had been admitted to the paediatric intensive care unit with unexplained loss of consciousness that required mechanical ventilation. The infant was previously fit and well, born through normal vaginal delivery at 40 weeks gestation. Neuroimaging showed intracranial, subarachnoid, and subdural haemorrhages. Dilated retinal examination revealed bilateral pre-macular haemorrhages and extensive superficial, intra-retinal and pre-retinal haemorrhages in the posterior pole, extending to the periphery. The optic discs were normal. A diagnosis of AHT was made. RetCam images documented the retinal appearance in both eyes (Supplementary information 1a and 1b). Ultra-widefield retinal imaging without sedation 6 days later documented resolution of the majority of the peripheral and posterior pole retinal haemorrhages, with improvement of bilateral subretinal, pre-macular haemorrhages in both eyes (Figure 3). Three weeks later, fundal appearances had normalised.
Ultra-widefield optomap colour images of right fundus (a) demonstrating haemorrhage at the posterior pole with widespread retinal haemorrhages extending into the retinal periphery. Macula exudative detachment (white arrowhead) is noted adjacent to the superotemporal arcade secondary to haemorrhage. The left (b) fundus demonstrates resolving haemorrhage at the posterior pole (white arrowhead) and resolving peripapillary intra-retinal haemorrhages extending into the retinal periphery, distributed adjacent to the retinal veins.
Case 4
A 15-month-old male was admitted to the paediatric intensive care unit in poor condition after a seizure and collapse attributed to a fall from a chair. A CT scan performed on admission revealed a 6 mm acute subdural haematoma in the right fronto-parietal region with midline shift, although neurosurgical intervention was not required. A skeletal survey demonstrated a wrist fracture. Blood coagulation disorders were excluded on testing. On examination, multiple bruises were present on the forehead, chin, and cheek. Dilated fundal examination (using a speculum and indirect ophthalmoscope without scleral indentation) the day after admission in an awake, active child was difficult, with suspected retinal haemorrhages inferior to the left optic disc only. However, ultra-widefield retinal imaging 6 days later in the outpatient clinic revealed multiple intra-retinal and pre-retinal haemorrhages in the left eye, and sparse retinal haemorrhages inferiorly in the right eye that were not identified clinically (Figure 4). The retinal appearances were consistent with inflicted trauma and a diagnosis of AHT was made.
Case 5
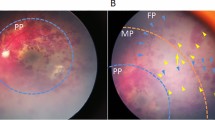
A 6-month-old female infant was referred to the paediatric vitreo-retinal service for surgical drainage of presumed pre-macular haemorrhage obscuring the fovea in both eyes. Two months earlier, the infant had presented with an acute encephalopathy and been found to have bilateral subdural haematomas and extensive retinal haemorrhages including at the posterior poles and obscuring the macular. A diagnosis of AHT was made. Neurological recovery was swift, but visual function remained poor and acuities were fix and follow OD, and no interest OS. Ultra-widefield colour images and intravenous FFA (0.1 mg/kg) were undertaken under oral sedation (chloral hydrate 50 mg/kg). A right posterior pole haemorrhage was demonstrated with a fluid level and the fovea was not obscured (Figure 5a). FFA confirmed normal macular perfusion and fovea was not obscured. Retinal vessels anterior to the haemorrhage (Figure 5c), prove at least part of the collection was intra-retinal rather than in the retrohyaloid space. However, the inferotemporal arcade is masked, indicating that the haemorrhage is likely to be multi-layered. No vitreo-retinal intervention was therefore recommended. The left eye revealed macular schisis with posterior pole retinal detachment, partial posterior vitreous detachment with persistent retrohyaloid blood (Figures 5b and d).
(a) Ultra-widefield optomap colour image of the right eye demonstrates the appearance of a pre-retinal haemorrhage at the posterior pole with a fluid level, partially obscuring the macula (white arrowhead). A resolving intra-retinal haemorrhage was noted adjacent to the optic disc (black arrowhead). The retinal periphery appears unaffected. (b) The left eye reveals macular schisis and an annulus of retrohyaloid blood (white arrowheads) at the limits of vitreo-retinal attachment. A fluid level of retrohyaloid blood is seen inferiorly, and the optic disc and fovea are obscured. (c) FFA confirms anterior displacement of retinal vessels over the posterior pole haemorrhage (white arrowhead) indicating that part of the haemorrhage is intra-retinal or subretinal, although the inferotemporal arcade is obscured, indicating that the haemorrhage is likely multi-layered. This information changed the clinical course: pars plana vitrectomy was not required. FFA further confirms normal macular perfusion. (d) FFA confirms the extent of pre-retinal haemorrhage and macular schisis. Perfusion of retinal arterioles is preserved. Fine perfused vessels (white arrowhead) are identified protruding anteriorly at the optic disc.
Discussion
Non-contact retinal imaging in infants using the Optos P200MA scanning laser ophthalmoscope is capable of acquiring clinically useful, high-quality, ultra-widefield images in the following settings: (1) colour images of premature infants with ROP, demonstrating disease progression and regression following treatment9 (2) FFA images using oral fluorescein in infants with ROP to guide retinal photocoagulation treatment8 (3) FFA images using oral fluorescein in an infant with incontinentia pigmenti to guide surgical planning10 (4) Intravenous FFA in infants with a range of retinal vascular disorders including familial exudative vitreoretinopathy.11
This series is the first to describe non-contact ultra-widefield retinal imaging of infants with suspected AHT. The Optos P200MA scanning laser ophthalmoscope effectively documented acute and chronic AHT-related retinal haemorrhages, accurately defined the anatomical location of haemorrhage in one infant who was referred for consideration of vitrectomy, and excluded retinal haemorrhages and consequently AHT in a fifth infant. A single, high-yield, definitive retinal image was attained in each case to confirm the diagnosis and document clinical findings. In case 4, an experienced paediatric ophthalmologist had achieved a very limited retinal view, but Optos imaging documented much more widespread abnormalities than were suspected. There were no adverse changes in physiological parameters in any infant that necessitated cessation of imaging.
RetCam is a well-established retinal imaging modality for infants, both for colour photographs and FFA in the context of ROP8, 9 and AHT.1 Non-contact ultra-widefield retinal imaging using the Optos P200MA scanning laser ophthalmoscope offers many advantages over RetCam for the documentation of retinal haemorrhages in the context of AHT:
Non-contact imaging
Infants with AHT may suffer significant intracranial haemorrhage and are at increased risk of bradycardia and respiratory arrest from secondary brainstem dysfunction. The Optos P200MA imaging system does not require ocular contact, and may consequently reduce the risk of stimulating oculocardiac/vagal responses in infants with AHT—a risk with RetCam contact imaging.12 However, the speculum that is necessary to undertake imaging is likely to cause the infant some distress.13 Ocular steering required on RetCam imaging to attain peripheral retinal images entails significant additional pressure on the globe, particularly without sedation when the infant’s Bell’s reflex may be preserved. The Optos P200MA may reduce the risk of inducing intra-retinal haemorrhages—which may be morphologically identical to those encountered in AHT—a possibility with RetCam contact imaging, at least in the setting of ROP.14 The risk of inducing retinal haemorrhages with the RetCam in suspected AHT is theoretical and has never been reported. We have not encountered any adverse events in infants undergoing non-contact Optos P200MA imaging in our centre—across any indication—using the ‘flying baby position’ in more than 100 examinations to date.8, 9, 10, 11 Larger numbers of Optos non-contact imaging studies are required before definitive conclusions can be made regarding safety.
Ocular contact required during RetCam imaging holds a theoretical risk of inducing retinal haemorrhages.14 However, in this report, the cause of the retinal haemorrhages was unclear. It must be noted that the retinal haemorrhages in this case (a premature infant) are likely to be different to the responses in a term infant with normal retinal development. The risk of cross infection between infants is also minimised as the P200MA imaging system does not contact the ocular surface.
Field of view
The Optos P200MA captures a 200° retinal field, superior to the 130° field possible with RetCam. Imaging of the retinal periphery is important in the setting of AHT.1 Systematic review of the distribution of retinal haemorrhages in abusive vs accidental head trauma identified 63% of children with AHT had peripheral retinal extension of haemorrhages (9% in non-AHT).1 Ultra-widefield documentation of peripheral retinal haemorrhages increases the likelihood of AHT, and may increase diagnostic precision.1 Accurate reporting of retinal haemorrhage location is paramount in AHT and a number of descriptive tools have been designed to aid documentation.3 To overcome challenges with photodocumentation of AHT in centres with no ophthalmic expertise, telemedicine-based imaging protocols are being evaluated.6 Ultra-widefield Optos P200MA may increase the sensitivity and specificity of retinal imaging of AHT in a telemedicine setting when compared to RetCam. However, a study directly comparing retinal imaging modalities is required in the setting of AHT before this conclusion can be made. The Optos P200MA imaging system may provide a greater field of imaging in the horizontal field (nasal and temporal) vs the vertical field (superior and inferior). In addition, the speculum and eyelashes may interfere with the inferior field of imaging (Figure 4).
General anaesthesia and sedation
Sedation is not required for the majority of infants imaged in the ophthalmic office setting with the Optos P200MA scanning laser ophthalmoscope owing to the speed of the imaging technique we have developed.8, 9, 10, 11 Colour images of both eyes in this series took <5 min in each infant. Retinal haemorrhages are present bilaterally in 83% of infants with AHT1; 2 images are required with Optos P200MA compared to 10–12 images with RetCam (typically 5–6 images are required for each eye to capture the entire retinal periphery which may be montaged). Sedation will be required more frequently to acquire high-quality images with RetCam than with Optos P200MA, due to a combination of ocular contact, eye steering, duration of imaging, and importance of ocular akinesia for image quality. Neurological observations are essential in infants with AHT due to intracranial haemorrhage; sedation may interfere with neurological parameters used to monitor infants, and presents risks related to the mechanism of action of the sedative drug (hypoventilation, hypotension etc.). Large infants and those over 6 months of age may require oral sedation for Optos P200MA retinal imaging.
Confocal optics
The Optos P200MA scanning laser ophthalmoscope is able to produce a uniform focus to multiple retinal locations, simultaneously increasing clarity of documentation across the retinal field. This is not the case with RetCam; multiple images are required with manual focus of the lens system using a foot pedal, adding time to the process of image capture. AHT may be characterised by subretinal haemorrhages, retrohyaloid haemorrhage, schisis cavities, retinal or macular folds, retinal detachment, and papilloedema.1 Confocal optics may produce clearer documentation of such AHT features, which are elevated from the retinal plane.
Speed of image acquisition and optics
Dual wavelength laser illumination of the Optos P200MA imaging system permits rapid image acquisition (0.25 s), overcoming the challenges to retinal imaging in mobile, non-sedated infants. The RetCam may suffer from image degradation in the setting of media opacity, such as vitreous haemorrhage in AHT.1 Image acquisition time is prolonged by the need to replenish coupling media, and requirement for manual focusing.
Ultra-widefield fluorescein angiography
Ultra-widefield fluorescein angiography may increase diagnostic yield vs RetCam-assisted FFA as all retinal locations may be captured simultaneously at all time points in the study. Confocal FFA imaging ensures focus is maintained on all structures in the examination. This advantage changed the course of management in one of the presented infants (case 5). A fine retinal vessel overlying a pre-macular haemorrhage was identified by Optos-assisted FFA, indicating that the haematoma was located in the subretinal space. Vitrectomy to clear a presumed retrohyaloid haemorrhage was subsequently not advised and the haemorrhage cleared spontaneously. The plane of retinal haemorrhage carries distinct implications in the likelihood of AHT1: the prevalence of multi-layered retinal haemorrhages is 77% in AHT and 73% of infants with AHT have evidence of retinal haemorrhages in all three layers (subretinal, intra-retinal, and subhyaloid).1 We have demonstrated that confocal Optos-assisted FFA can accurately characterize the anatomical location of retinal haemorrhages in a single frame.
The RetCam has several advantages over the Optos P200MA imaging system in the setting infants with AHT:
-
1
Portability. Severe AHT may necessitate intubation to maintain the airway of infants secondary to impaired consciousness from intracranial bleeding. The RetCam is required to image the retina of a supine infant too unstable to transfer, or who is pharmacologically sedated or mechanically ventilated. The Optos P200MA is not portable and is not currently capable of imaging an infant required to remain in a supine position. A dedicated P200MA imaging system on a neonatal high dependency unit—as has now become the case in our centre for the management of ROP—may permit ultra-widefield retinal imaging in unstable infants with AHT by eliminating the need for transfer to the ophthalmic office setting.
-
2
Access to and familiarity with RetCam. RetCam is widely used for paediatric retinal imaging. Many ophthalmic departments possess the RetCam, and paediatric ophthalmologists are familiar and comfortable with its use. Retinal imaging in infants with the Optos P200MA using the ‘flying baby position’ involves a learning curve for both ophthalmologist, imaging technician and paediatric nursing staff during the process of imaging. In our experience, imaging of 3–5 infants is typically required to become familiar and competent with the technique.
This observational series is the first to demonstrate that the Optos P200MA scanning laser ophthalmoscope can provide high-quality, ultra-widefield retinal images in infants with suspected AHT using a non-contact technique. We suggest that paediatricians and ophthalmologists should be aware that non-contact imaging without sedation in stable infants with suspected AHT may be the preferred modality to document and record any abnormalities.

References
Maguire SA, Watts PO, Shaw AD, Holden S, Taylor RH, Watkins WJ et al. Retinal haemorrhages and related findings in abusive and non-abusive head trauma: a systematic review. Eye 2013; 27 (1): 28–36.
Carty H, Ratcliffe J . The shaken infant syndrome. BMJ 1995; 310 (6976): 344–345.
Tandon A, McIntyre S, Yu A, Stephens D, Leiby B, Croker S et al. Retinal haemorrhage description tool. Br J Ophthalmol 2011; 95 (12): 1719–1722.
Nakagawa TA, Skrinska R . Improved documentation of retinal hemorrhages using a wide-field digital ophthalmic camera in patients who experienced abusive head trauma. Arch Pediatr Adolesc Med 2001; 155 (10): 1149–1152.
Blair MP, Shapiro MJ, Hartnett ME . Fluorescein angiography to estimate normal peripheral retinal nonperfusion in children. J AAPOS 2012; 16 (3): 234–237.
Saleh M, Schoenlaub S, Desprez P, Bourcier T, Gaucher D, Astruc D et al. Use of digital camera imaging of eye fundus for telemedicine in children suspected of abusive head injury. Br J Ophthalmol 2009; 93 (4): 424–428.
Mulvihill AO, Jones P, Tandon A, Fleck BW, Minns RA . An inter-observer and intra-observer study of a classification of RetCam images of retinal haemorrhages in children. Br J Ophthalmol 2011; 95 (1): 99–104.
Fung TH, Muqit MM, Mordant DJ, Smith LM, Patel CK . Noncontact high-resolution ultra-wide-field oral fluorescein angiography in premature infants with retinopathy of prematurity. JAMA Ophthalmol 2014; 132 (1): 108–110.
Patel CK, Fung TH, Muqit MM, Mordant DJ, Brett J, Smith L et al. Non-contact ultra-widefield imaging of retinopathy of prematurity using the Optos dual wavelength scanning laser ophthalmoscope. Eye 2013; 27 (5): 589–596.
Patel CK, Fung TH, Muqit MM, Mordant DJ, Geh V . Non-contact ultra-widefield retinal imaging and fundus fluorescein angiography of an infant with incontinentia pigmenti without sedation in an ophthalmic office setting. J AAPOS 2013; 17 (3): 309–311.
Fung TH, Yusuf IH, Smith LM, Brett J, Weston L, Patel CK . Outpatient ultra wide-field intravenous fundus fluorescein angiography in infants using the Optos P200MA scanning laser ophthalmoscope. Br J Ophthalmol 2014; 98 (3): 302–304.
Kemper AR, Wallace DK, Quinn GE . Systematic review of digital imaging screening strategies for retinopathy of prematurity. Pediatrics 2008; 122 (4): 825–830.
Castellanos MA, Schwartz S, Leal R, Chan RV, Quiroz-Mercado H . Pain assessment in premature infants treated with intravitreal antiangiogenic therapy for retinopathy of prematurity under topical anesthesia. Graefes Arch Clin Exp Ophthalmol 2013; 251 (2): 491–494.
Adams GG, Clark BJ, Fang S, Hill M . Retinal haemorrhages in an infant following RetCam screening for retinopathy of prematurity. Eye 2004; 18 (6): 652–653.
Acknowledgements
CK Patel had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author contributions
Design and conduct of the study: IHY, THMF, JSE, CKP. Collection, management, analysis, and interpretation of data: IHY, JKB, THMF, JSE, CKP. Preparation, review, or approval of the manuscript: IHY, JKB, THMF, JSE, CKP.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Yusuf, I., Barnes, J., Fung, T. et al. Non-contact ultra-widefield retinal imaging of infants with suspected abusive head trauma. Eye 31, 353–363 (2017). https://doi.org/10.1038/eye.2017.2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2017.2
This article is cited by
-
The role of retinal imaging in the management of abusive head trauma cases
International Journal of Legal Medicine (2022)