Abstract
Purpose
The purpose of this study is to compare uveal melanomas (UMs) in men and women.
Methods
The Liverpool Ocular Oncology Centre (LOOC) database was reviewed. Patients treated for UM at the LOOC between 1993 and 2010 were selected. Differences between sexes were identified using the χ2-test for categorical variables and the Mann–Whitney test for continuous variables.
Results
The 3380 patients comprised 1685 women and 1695 men. The tumours were considered clinically to have arisen in choroid in 89.5%, ciliary body in 5.3%, and iris in 5.2%. Tumours in women were less likely to originate in choroid (87.2 vs91.7%; P<0.001) and showed more circumferential spread in ciliary body (P<0.001) and iris (P=0.003). Tumours in men were more likely to extend to within 3 mm of optic disc or fovea (46.3 vs39.0%, P<0.001), showing more extensive optic-disc involvement (P<0.001). The median largest basal tumour diameter was 12.2 mm in men and 11.9 mm in women (P=0.001). The tumour thickness had a median of 4.4 mm and 3.8 mm in men and women, respectively (P=0.015). The 180 ciliary body tumours occurred in 112 women and 68 men. In these, the prevalence of extraocular spread was higher in women (19.6 vs8.8%; P=0.052). The 175 iris melanomas were more common in women than men (103 vs72, respectively).
Conclusions
In men, UMs tend to be larger and more posterior than in women.
Similar content being viewed by others
Introduction
Uveal melanomas (UMs) are rare, with an incidence of approximately six per million per year.1 More than 90% of UMs involve the choroid. The age at diagnosis peaks at approximately 60 years.1 Most patients present with visual symptoms.2 In a significant minority of patients, the tumour is asymptomatic and detected on routine examination (eg, screening for diabetic retinopathy).2
Ocular treatment is aimed at conserving the eye and useful vision, and consists of various forms of radiotherapy, phototherapy, and surgical resection, which are administered individually or in combination.3 About 30–40% of patients require enucleation.4
Approximately 50% of patients develop metastatic disease, which almost always involves the liver, and which is usually fatal within a year of becoming symptomatic. Predictors of metastatic death include the following: advanced clinical stage, histological features indicating high grade of malignancy, and genetic abnormalities, such as chromosome 3 loss.5, 6
UMs affect both sexes in equal numbers, but males have been reported to show higher disease-specific mortality.7, 8 Lower survival rates in males have also been reported in cutaneous melanoma.9 This is believed to correlate with more aggressive histology in males.10 Males show higher rates of rhegmatogenous retinal detachment after trans-scleral local resection, and are more likely to require enucleation after proton-beam radiotherapy.11, 12 In view of such differences, there would seem to be scope for comparing UMs in males and females. Such investigation may provide insights into the biology of UMs and may help design outcomes analyses taking gender into account.
The aims of this study were to compare UMs in men and women in terms of age at presentation, clinical features, histological findings, and genetic abnormalities.
Patients and methods
Inclusion and exclusion criteria
Patients were included in this study if diagnosed clinically as having a UM, if assessed at the Liverpool Ocular Oncology Centre (LOOC) between January 1993 and December 2010, and if they resided in the British Isles. The patients were identified by searching the LOOC database. Some patients with a clinically suspected UM were excluded because they were not treated, for example, if they were observed because of an uncertain diagnosis or if they declined therapy. These patients were excluded to reduce the chances of including naevi in the sample. A few patients (ie, less than 20) were excluded because they had received treatment before referral to the LOOC, and the primary method of treatment for their UM was not known. This problem tended to occur when the initial surgical procedure was recorded as biopsy. Eleven patients were excluded because of missing data on anterior or posterior extent, and two patients were excluded because they had bilateral UMs.
Clinical assessment
Clinical assessment included full ocular and systemic history and examination, including ocular B-scan ultrasonography. The likelihood of a clinical diagnosis of melanoma increased with the number of features suggestive of malignancy. For choroidal tumours, these were as follows: thickness exceeding 2 mm, basal tumour diameter exceeding 10 mm, serous retinal detachment, lipofuscin (ie, ‘orange pigment’), and/or a collar-stud shape. In the case of ciliary body tumours, malignancy was suspected if the tumour exceeded 2 mm in diameter and/or showed invasion into the anterior chamber or extraocularly (although these features can occur with melanocytoma). With iris melanocytic tumours, signs of malignancy were considered to be as follows: basal diameter exceeding 3 mm, thickness exceeding 1 mm, tumour vascularity, seeding, and diffuse spread. With all tumour locations, documented growth was considered indicative of melanoma. In some cases, the diagnosis was established by aspirational, incisional, or excisional biopsy.
Tumours were classified clinically according to their most likely site of origin within the uvea, which was determined by their ‘centre of gravity’. As the site of origin was not always identifiable, we also analysed anterior and posterior tumour margins. Choroidal tumours were categorised as involving the ciliary body if they extended anterior to the ora, and any tumour was categorised as involving the anterior chamber if visible in the iris or angle on slit-lamp examination.
With few exceptions, all patients were assessed at LOOC by the first author (BED), who also performed the ultrasonography. Ethics Committee approval was obtained (Number 11/NW/0179). The study was conducted in accordance with the ‘Declaration of Helsinki’.
Histological assessment
Histological examination was performed on all eyes that were treated by enucleation or local resection, and those that were biopsied. Until 2002, tumour specimens were routinely fixed in glutaraldehyde. After that date, buffered formalin was used. Histology was performed using sections stained with haematoxylin and eosin and, if necessary, immunohistochemistry using Melan A. Melanomas were categorised as being of spindle-cell, epithelioid, or mixed type, using the modified Callender system. They were recorded as having epithelioid cells irrespective of the proportion of such cells in the tumour. From 1994 onwards, extravascular matrix patterns were assessed so as to identify closed connective tissue loops, and this was done using the periodic-acid-Schiff reagent, without counterstaining. Mitoses were counted in 40 high-power fields ( × 40 objective) in haematoxylin and eosin sections. Extraocular extension was recorded as being present whether this was noted clinically or on pathological examination.
Genetic studies
We analysed tumours for chromosome 3 loss, chromosome 6p gain, and chromosome 8q gain. These studies were performed using microsatellite analysis between 1999 and 2000, fluorescence in situ hybridisation between 1999 and 2007, and with multiplex ligation-dependent probe amplification from 2006 onwards, with some overlap of techniques during transition periods.5, 13, 14 These tests were routinely performed on fresh tumour samples.
Statistical methods
Clinical, histological, and genetical data were documented synoptically on paper forms in the patients’ casenotes and were computerised prospectively using a customised database. Data analysis was performed using a statistical programme (SPSS, SPSS Inc., Chicago, IL, USA). Correlations between baseline factors and sex were analysed using the χ2-test (without Yates's adjustment) for categorical variables, and with the Mann–Whitney test for continuous variables. A P-value of less than 0.05 was considered to be statistically significant. All statistical tests were two-sided.
Results
All tumours
The 3380 patients comprised 1685 (49.9%) women and 1695 (50.1%) men, with a median age of 61.4 years (range 7.3–96.9; Table 1). Referral was from England in 2458 patients, Ireland in 294 patients, Wales in 293 patients, Scotland in 215 patients, and Northern Ireland in 120 patients. In men, the tumour was considered to originate in choroid in 1555 (91.7%) patients, the ciliary body in 68 (4.0%) patients, and in the iris in 72 (4.2%), whereas in women, the tumour appeared to originate in choroid in 1470 (87.2%) patients, the ciliary body in 112 (6.6%), and the iris in 103 (6.1%; χ2-test, P<0.001). The anterior tumour margin extended anterior to ora serrata in 33.8% of women and in 26.3% of men (χ2-test, P<0.001), with women showing greater involvement of ciliary body (Mann–Whitney, P<0.001) and iris (Mann–Whitney, P=0.004; Table 2). The posterior tumour margin extended to within 3 mm of optic disc or fovea in 39.0% of women and 46.3% of men (χ2-test, P<0.001), with the extent of optic-disc involvement being greater in men than women (Mann–Whitney, P<0.001). The median largest basal tumour diameter was 12.2 mm in men and 11.9 mm in women (Mann–Whitney, P=0.001), whereas the tumour thickness had a median of 4.4 and 3.8 mm in men and women, respectively (Mann–Whitney, P=0.015). No significant differences were found in age, laterality, initial visual acuity, angle involvement, coronal location, sagittal location, presence of extrascleral tumour extension, histology, and tumour genetic abnormalities (Tables 1,2,3).
Choroidal melanoma
Of the 3025 choroidal melanomas, 1470 (48.6%) affected women and 1555 (51.4%) occurred in men. The anterior tumour margin extended anterior to ora serrata in 24.1% of women as compared with 19.7% of men (χ2-test, P=0.012). The posterior tumour margin extended to within two disc diameters of the optic disc in 44.6% of women and 50.5% of men (χ2-test, P<0.001). Optic-disc involvement was more extensive in men (Mann–Whitney, P=0.003). Tumours in men also tended to have a wider base (Mann–Whitney, P=0.009), a greater height (Mann–Whitney, P=0.005), and therefore, a more advanced TNM size category (T3 or T4 in 35.1% men vs 20.2% women; χ2-test, P=0.013). Perforation of Bruch's membrane with development of a collar-stud tumour shape was more common in men (14.6% in men vs 11.4% in women; χ2-test, P=0.008). The prevalence of tumours with epithelioid melanoma cells was higher in men (64.3 vs 58.6%; χ2-test, P=0.027; Table 3). There were no significant differences in the prevalence of chromosome 3, 6p, and 8q abnormalities between the two sexes.
Ciliary body melanoma
The 180 ciliary body tumours occurred in 112 (62%) women and 68 (38%) men. Circumferential and antero-posterior extent did not show significant differences between the two sexes. There were also no significant differences in tumour dimensions, histological findings, or genetic results.
Iris melanoma
The 175 iris melanomas were more common in women than in men (ie, 103 vs 72, respectively). The only significant difference was in the age at presentation, which was slightly greater in men than women (median, 56.4 vs 51.8 years; Mann–Whitney, P=0.039). No significant differences were found in tumour dimensions, extent, and histology. The number of tumours examined genetically was too small for statistical analysis.
Discussion
This study found that UMs tended to more posterior in men than in women so that the tumour was more likely to involve the optic disc in men, and tended to show greater involvement of ciliary body and iris in women. Choroidal tumours in men tended to be larger and were more likely to rupture Bruch's membrane, and contain epithelioid cells. Men with iris melanoma tended to present at an older age; otherwise, there were no significant sex differences in iris and ciliary body melanomas, possibly because of smaller sample sizes. Interestingly, no significant differences were found in genetic tumour type.
The main strengths of the study are the large number of patients and the fact that almost all clinical and ultrasonographical examinations were performed by the same surgeon (BED). Another strength is that virtually all the data were collected and computerised prospectively. To our knowledge, no other studies have investigated these factors in such detail and on such a large number of cases. The large number of patients made it possible to perform correlations according to the uveal structure in which the tumour arose, thereby enhancing interpretation of the results. For example, women showed more extensive iris involvement, because their tumour tended to be more anterior and not because it was larger.
Our study has several weaknesses. The main weakness is that many tumours were not examined histologically so that some small tumours may have been benign. However, because the diagnosis was based on widely accepted clinical features, and as the same criteria were used in both sexes, the number of misdiagnoses and the chances of bias are likely to be small. With larger numbers of iris and ciliary body tumours, more of the variables may have shown a statistically significant difference between the sexes. Failure to detect genuine sex differences may also have occurred with rare features, such as retinal perforation. Conversely, because of the large number of analyses, it is possible that some of the differences may have been due to chance. Methods of genetic testing changed during the course of this study, but any resulting variations are likely to have affected both sexes equally. In some patients, it was difficult to determine clinically whether the tumour originated in choroid or ciliary body, or in ciliary body or iris, but the reporting of antero-posterior tumour extent should have mitigated this problem.
We are unable to explain why UMs tended to be larger in men than in women. One would have expected men to have smaller tumours than in women, because of the relatively posterior extension, which should have facilitated detection and caused visual disturbances sooner, being closer to fovea; however, this was not the case. We plan to correlate tumour features with mode of presentation. An investigation on cutaneous melanoma suggests that the increased Breslow thickness in men reflects more aggressive tumour growth because their tumours show higher grade of malignancy than melanomas in women.10 In our study, choroidal melanomas were more likely to show epithelioid cells in men than in women (P=0.027); however, the mitotic count showed no significant difference between sexes. The relatively large size and the higher prevalence of epithelioid cells in men may have occurred because of a longer delay before treatment, or the larger tumour size in men may have been due to more rapid growth of epithelioid melanoma, without a demonstrable increase in the mitotic count.
We are also unable to explain why UMs in men tend to be more posterior than in women. This seems to be a genuine finding, supported by data showing more extensive optic-disc involvement in men and more extensive ciliary body involvement in women. Furthermore, in a study correlating tumour thickness with metastasis, choroidal melanomas were slightly more common in men (51 vs 49%), whereas ciliary body and iris melanomas were more common in women (41 vs 59% and 48 vs 52%, respectively).15
A surprising and unexplained finding of the current study was that, although the overall incidence of extraocular melanoma extension was the same in males and females, ciliary body melanomas were perhaps more likely to show extraocular extension in women than in men (19.6 vs 8.8%; χ2-test, P=0.052). This occurred despite the absence of significant differences in circumferential spread and tumour dimensions. These findings are in agreement with those of our previous report (incorporating the same patients as the present study), in which we demonstrated extraocular spread along aqueous drainage channels occurring in 15% of tumours involving ciliary body or angle.16
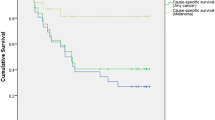
In view of the finding that chromosome 3 loss and chromosome 8q gain were not more common in men than women, one would not expect significances in the metastatic mortality in the long term, after taking any lead time bias into account. This finding is in keeping with a study by Kujala et al,17 which took competing risks into account, reporting no significant difference in survival when the analysis adjusted for death from other causes. We plan to perform our own studies correlating mortality with gender, using different methods for dealing with competing risks.
This study raises several questions. Why is there a tendency for UMs to be more anterior in women than in men? Why are choroidal melanomas larger in men than in women? Why do men with an iris melanoma tend to present at a greater age than women? Are these differences genuine, and if so, do they arise because of gender variation in behaviour or exposure to environmental pathogens? Answers to these questions may provide insights into the cause and behaviour of UVs. In any case, the information provided by this study should be useful in future research investigating the impact of treatment on survival and other outcomes.

References
Singh AD, Bergman L, Seregard S . Uveal melanoma: epidemiologic aspects. In: Singh AD, Damato B, Pe'er J et al (eds). Clinical Ophthalmic Oncology. Saunders Elsevier: Philadelphia, 2007, pp 198–204.
Damato B . Detection of uveal melanoma by optometrists in the United Kingdom. Ophthalmic Physiol Opt 2001; 21: 268–271.
Damato B . Treatment of primary intraocular melanoma. Expert Rev Anticancer Ther 2006; 6: 493–506.
Damato B, Lecuona K . Conservation of eyes with choroidal melanoma by a multimodality approach to treatment: an audit of 1632 patients. Ophthalmology 2004; 111: 977–983.
Damato B, Dopierala JA, Coupland SE . Genotypic profiling of 452 choroidal melanomas with Multiplex Ligation-Dependent Probe Amplification. Clin Cancer Res 2010; 16: 6083–6092.
Onken MD, Worley LA, Tuscan MD, Harbour JW . An accurate, clinically feasible multi-gene expression assay for predicting metastasis in uveal melanoma. J Mol Diagn 2010; 12: 461–468.
Isager P, Ehlers N, Overgaard J . Prognostic factors for survival after enucleation for choroidal and ciliary body melanomas. Acta Ophthalmol Scand 2004; 82: 517–525.
Virgili G, Gatta G, Ciccolallo L, Capocaccia R, Biggeri A, Crocetti E et al. Survival in patients with uveal melanoma in Europe. Arch Ophthalmol 2008; 126: 1413–1418.
de Vries E, Nijsten TE, Visser O, Bastiaannet E, van Hattem S, Janssen-Heijnen ML et al. Superior survival of females among 10,538 Dutch melanoma patients is independent of Breslow thickness, histologic type and tumor site. Ann Oncol 2008; 19: 583–589.
Liu W, Dowling JP, Murray WK, Liu W, Dowling JP, Murray WK et al. Rate of growth in melanomas: characteristics and associations of rapidly growing melanomas. Arch Dermatol 2006; 142: 1551–1558.
Damato B, Groenewald CP, McGalliard JN, Wong D . Rhegmatogenous retinal detachment after transscleral local resection of choroidal melanoma. Ophthalmology 2002; 109: 2137–2143.
Egger E, Zografos L, Schalenbourg A, Beati D, Böhringer T, Chamot L et al. Eye retention after proton beam radiotherapy for uveal melanoma. Int J Radiat Oncol Biol Phys 2003; 55: 867–880.
Damato B, Duke C, Coupland SE, Hiscott P, Smith PA, Campbell I et al. Cytogenetics of uveal melanoma: a 7-year clinical experience. Ophthalmology 2007; 114: 1925–1931.
Scholes AG, Damato BE, Nunn J, Hiscott P, Grierson I, Field JK et al. Monosomy 3 in uveal melanoma: correlation with clinical and histologic predictors of survival. Invest Ophthalmol Vis Sci 2003; 44: 1008–1011.
Shields CL, Furuta M, Thangappan A, Nagori S, Mashayekhi A, Lally DR et al. Metastasis of uveal melanoma millimeter-by-millimeter in 8033 consecutive eyes. Arch Ophthalmol 2009; 127: 989–998.
Coupland SE, Campbell I, Damato B . Routes of extraocular extension of uveal melanoma: risk factors and influence on survival probability. Ophthalmology 2008; 115: 1778–1785.
Kujala E, Mäkitie T, Kivelä T . Very long-term prognosis of patients with malignant uveal melanoma. Invest Ophthalmol Vis Sci 2003; 44: 4651–4659.
Acknowledgements
We are grateful to Mr Gary Cheetham for database management, Dr Ian Campbell for statistical advice, Miss Nicola Longrigg for administrative assistance, and the National Specialist Commissioning Team for supporting our oncology service. This study is sponsored by the Research and Development Unit of the Royal Liverpool University Hospital.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented orally at the Ophthalmic Oncolology Group Meeting, Crete, October 2010.
Rights and permissions
About this article
Cite this article
Damato, B., Coupland, S. Differences in uveal melanomas between men and women from the British Isles. Eye 26, 292–299 (2012). https://doi.org/10.1038/eye.2011.272
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2011.272
Keywords
This article is cited by
-
Socket outcomes following enucleation for uveal melanoma: post enucleation socket syndrome can be challenging
Eye (2024)
-
Ocular oncology service during the COVID-19 outbreak: uveal melanoma characteristics presenting in 2019 compared to 2020
Irish Journal of Medical Science (1971 -) (2023)
-
Topography and clinical features of iris melanoma
BMC Ophthalmology (2022)
-
Radiation Dose Aspects of Hepatic Artery Infusion Chemotherapy in Uveal Melanoma Patients with Liver Metastases
CardioVascular and Interventional Radiology (2022)
-
The epidemiology of uveal melanoma in Germany: a nationwide report of incidence and survival between 2009 and 2015
Graefe's Archive for Clinical and Experimental Ophthalmology (2022)