Abstract
Purpose
To establish normative values for macular light sensitivity and to determine the intrasession fluctuation of perimetric responses using the OPKO/OTI microperimeter.
Methods
A total of 32 visually normal subjects participated in the study. A standardized grid pattern was used for testing, which consisted of 28 points arranged concentrically in three circles that occupied an area of 11° (in diameter) within the central macula. Each subject participated in at least two tests. Parameters evaluated included: overall mean macular sensitivity for test 1 and 2, overall difference in mean macular sensitivity between tests, and the mean sensitivity for each circle. The relationship between sensitivity and age was also examined.
Results
The overall median sensitivity for test 1 was 16.8 decibels (dB) and for test 2 was 16.9 dB. The median sensitivities for test 1 and test 2 were not significantly different (P=0.72). The mean intrasession sensitivity difference was 0.13 dB. The variability of the sensitivity difference between tests decreased as mean sensitivity increased. The sensitivity values averaged across the two tests for inner, middle, and outer circles ranged from 14.3 to 18.8 dB (median value of 16.9 dB), 13.8–18.3 dB (median value of 17.2 dB), and 11.3–18.3 dB (median value of 16.6 dB), respectively. Linear regression analysis showed a 0.5 dB sensitivity loss for each decade of life.
Conclusion
We documented a narrow range of intrasession fluctuation using the OPKO/OTI microperimeter. The establishment of normative sensitivity values will facilitate monitoring the loss of macular visual function in patients with retinal disease.
Similar content being viewed by others
Introduction
The introduction of microperimetry testing with a scanning laser ophthalmoscope (SLO) in 19821, 2 added a useful tool for clinicians to evaluate macular function and made possible direct correlations of structural and functional abnormalities. Simultaneous viewing of the retina during visual field (perimetry) testing is a key feature that facilitates the correlation of functional impairment (scotomas) with observed lesions in the fundus. A SLO3, 4 has been used for microperimetry testing in various retinal disorders. However, its use has been limited because of hardware reliability issues, cost, and lack of an eye tracking system (real-time image alignment) that would allow for an automated follow-up examination.
In 2003, Nidek Technologies (Padova, Italy) introduced the MP-1 microperimeter that used a liquid crystal display to project stimuli. This device incorporated an automatic eye tracking system, which permitted compensation for eye movements under real time conditions. In addition, the MP-1 tested a larger area of the retina.5 Recently, in 2006, OPKO/OTI (OPKO Instrumentation, Miami, FL, USA) developed a microperimeter in conjunction with spectral domain optical coherence tomography (SD-OCT). This newer modality offers the advantage of correlating functional deficits not only with SLO infrared images (retinal en face images), but also with cross sectional retinal images, as two images are simultaneously produced and displayed during the scanning mode. One is a spectral OCT image, whereas the other is a confocal image of the fundus.
The determination of intrasession fluctuation of perimetric measurements in normal individuals is paramount before attempting to evaluate patients with subtle or even severe fundus abnormalities. Normative values for the MP-1 device have been reported by Shah et al 6 in 37 healthy subjects and test-retest repeatability of the same device has also been demonstrated in patients with various macular disorders in a previous study by Chen et al. 7 In addition, Midena et al8 evaluated light sensitivity values and short-term repeatability using the MP-1 microperimeter in normally sighted volunteers. However, to our knowledge, there are no available published data in the ophthalmic literature concerning normative sensitivity values and intrasession repeatability using the OPKO/OTI SD-OCT/SLO microperimeter. The aim of the present study was to determine the macular sensitivity of visually normal subjects and to investigate the repeatability (intraexaminer, intrasession) using the SD-OCT/SLO microperimeter.
Materials and methods
Subjects
A total of 32 visually normal volunteers (13 females and 19 males) with a mean age of 41.6 years (range: 28–66 years) participated in the study. Our cohort of subjects included 21 Caucasians, 7 Asians, 3 African-Americans, and 1 Hispanic. The subjects had no previous history of ocular disease. Best corrected visual acuity was 20/25 or better, and a dilated fundus examination was unremarkable. Subjects were excluded from the study if they showed any lens or other ocular media opacities or if medical problems, such as diabetes or systemic hypertension, were present and were not well controlled. The study conformed to the tenets of the Declaration of Helsinki and the experiments were approved by an institutional review board at the University of Illinois at Chicago. Written informed consent was obtained from each subject. The study was Health Insurance Portability and Accountability Act compliant.
Microperimetry testing
The dominant eye of each subject was tested following dilation with 2.5% phenylephrine. The non-examined eye was patched during testing. Each subject was seated in a dimly illuminated room for 5 min before testing was initiated, which was performed by a single examiner (AA). We attempted to perform three consecutive microperimetry tests for each subject. However, three tests were completed in only 16 of the 32 subjects, due to subjects’ fatigue, lack of concentration, or attention. Two tests were successfully performed in 16 of the 32 subjects.
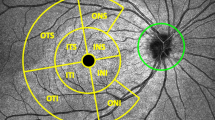
The Polar 3 testing pattern was used for all subjects. Polar 3 is a standardized grid composed of 28 points arranged in three concentric circles (2.3°, 6.6°, and 11° in diameter) within the central macula. The inner circle is composed of four points, whereas the middle and outer circles are each composed of 12 points. Figure 1 shows the Polar 3 test grid superimposed on the SLO infrared image of one representative subject. The size of the stimulus was equivalent to the Goldmann III, and the duration of presentation was 200 ms, with a 1.5 s interval between stimulus presentations. The stimulus was a luminance increment presented on an adapting field of 10 cd/m2. During sensitivity measurements, the luminance increments (difference between target luminance and background luminance) were changed in 2 decibel (dB) steps. The luminance calibrations were provided by the manufacturer.
Before testing, all subjects received standardized information by the examiner concerning the purpose of the test and underwent a practise test, in which stimuli of various intensities were presented while the patient focused on a fixation target. Subsequently, the test was initiated after a well-defined anatomical retinal locus was identified by the operator (usually the bifurcation of a main retinal vessel was chosen), which is required for the eye-tracking feature of the instrument. Between tests, subjects rested for 5 min. To determine if subjects preferred one fixation target over another, different fixation targets were used. The fixation targets included a white cross and a green spot, both subtending 3.3°, and a smaller red square, which subtended 0.66°. After the completion of the test, all participants reported whether the fixation target was suitable for fixation.
Parameters evaluated
The parameters that were evaluated included: overall mean macular sensitivity and SD for tests 1 and 2, overall difference in mean macular sensitivity between these tests, mean sensitivity for each circle, number of test points that showed less than a 4 dB difference between tests, and fixation stability (percent of fixation points within the central 2°). In addition, the overall mean macular sensitivity and the difference in mean macular sensitivity between the two tests with the largest sensitivity difference was determined for the 16 subjects who completed three measurements. The relationship between sensitivity and age was also examined.
Analysis
Normality of the data distributions was assessed with the Shapiro–Wilk test. Differences in sensitivity between tests were analysed using the Wilcoxon signed rank test, due to the non-normal distribution of the sensitivity values. Additional analyses were performed using the Mann–Whitney rank sum test and the Kruskal–Wallis one-way analysis of variance on ranks for variables that were not normally distributed, whereas an unpaired t-test was used for variables that were normally distributed. Statistical analyses were performed with commercial software (SigmaPlot ver. 11.1; Chicago, IL, USA). Statistical significance was defined as P<0.05.
The agreement between the sensitivity values obtained in test 1 and test 2 was analysed using the approach of Bland and Altman9, 10 as follows. First, a sensitivity difference in dB was defined for each subject by subtracting the sensitivity value obtained from test 2 from the value obtained from test 1. Second, the mean sensitivity value for tests 1 and 2 was determined for each subject. Then, for each subject, the sensitivity difference was plotted as a function of the mean sensitivity. The same procedure was used for examining the difference in sensitivity between the two tests with the largest sensitivity difference for the 16 subjects who completed three measurements.
Previous data obtained with the MP-1 show that mean sensitivity is related to the age of the subject.6, 8 To determine if this is also the case for the SD-OCT/SLO microperimeter, linear regression analysis was used to determine the mean sensitivity decline per decade of life.
Results
The overall mean sensitivity value for each subject was calculated automatically by the instrument by taking the average of all 28-test locations. For test 1, the overall mean sensitivity for the 32 subjects ranged from 13.4 to 18.2 dB (median value of 16.8 dB). For test 2, the overall mean sensitivity ranged from 12.7 to 18.3 dB (median value of 16.9 dB). The median sensitivity values for these two tests were not significantly different (Wilcoxon test, P=0.72). Given the negligible overall mean sensitivity difference between the two tests, the data of tests 1 and 2 were combined for the calculation of the mean sensitivity for each circle (inner, middle, outer). The sensitivity values for the inner circle ranged from 14.3 to 18.8 dB (median value of 16.9 dB), the middle circle ranged from 13.8 to 18.3 dB (median value of 17.2 dB), and the outer circle ranged form 11.3 to 18.3 dB (median value of 16.6 dB). A Kruskal–Wallis one-way analysis of variance on ranks indicated that the median sensitivities of the three circles were not significantly different (Kruskal–Wallis, P=0.17). For subjects tested with the small red spot, there was a trend for the median sensitivity to be higher in the central circle (17.8 dB) and lower for the middle (17.2 dB) and outer circles (16.5 dB). However, these differences were not statistically significant (Kruskal–Wallis, P=0.10). For subjects tested with the larger fixation targets (white cross and green spot), there was no systematic decrease in sensitivity as eccentricity increased. The median sensitivity for the inner, middle, and outer circles was 16.3, 17.3, and 16.8 dB, which did not differ significantly (Kruskal–Wallis, P=0.06).
Figure 2 plots the overall sensitivity difference between tests 1 and 2 as a function of the overall mean sensitivity for tests 1 and 2, for each subject. The overall mean sensitivity difference between the two tests averaged across subjects was 0.13 dB. To determine if the sensitivity difference between tests 1 and 2 varied as a function of the overall mean sensitivity, the data in Figure 2 were fit by linear regression. The slope of the best-fit regression line fit to the sensitivity difference vs mean sensitivity data was not significantly different from zero (t=−0.88, P=0.39). The nonsignificant slope indicates that the sensitivity difference between the two tests did not vary as a function of the mean sensitivity. Thus, a straight line with a slope of zero and a y-intercept of 0.13 was fit to the data, represented by the dashed horizontal line in Figure 2.
The variability of the sensitivity difference between the two tests was then examined using the approach of Bland and Altman.9, 10 In this analysis, the value of each data point in Figure 2 was subtracted from the overall mean sensitivity value pooled across subjects (0.13 dB). The result of this computation is equivalent to calculating the residuals from the dashed line in Figure 2. A linear regression line was then fit to the absolute value of these residuals. Following Bland and Altman,9 the 95% limits of repeatability were given by:

where D is the sensitivity difference between the two tests and R=b0+ b1A. The constants b0 and b1 are the y-intercept and slope from the linear regression line fit to the absolute value of the residuals vs mean sensitivity, and A is the mean sensitivity value for tests 1 and 2 for a given subject. The 95% limits of repeatability are shown as the solid grey lines in Figure 2. These lines represent the limits within which 95% of the intrasession sensitivity differences are expected to fall and indicate that the variability of the sensitivity differences decreased as mean sensitivity increased. Although the difference in sensitivity between the two tests did not vary as a function of the mean of the two tests (dashed line in Figure 2), the variability of the sensitivity difference between the tests was dependent on mean sensitivity (solid lines in Figure 2).
A similar analysis was conducted for the 16 subjects who completed three sensitivity measurements. The results for these subjects are presented in Figure 3, which plots the sensitivity difference between the two tests with the greatest difference as a function of the mean sensitivity for these tests. In this plot, positive values indicate that the test with greater sensitivity was obtained before the test with poorer sensitivity, whereas negative values indicate the test with greater sensitivity was obtained after the test with poorer sensitivity. The overall mean sensitivity difference between the two tests averaged across subjects was 0.20 dB. Because the slope of the linear regression line fit to these data was not significantly different from zero (t=0.76, P=0.46), a straight line with a slope of zero and a y-intercept of 0.20 was fit to the data, represented by the dashed horizontal line in Figure 3. Equation (1) was used to calculate the 95% limits of repeatability, which are shown as solid gray lines in Figure 3. Of note, the Bland–Altman plot for the difference between tests 1 and 2 (Figure 2) was highly similar to that for the difference between the tests with the maximum difference (Figure 3). This finding indicates that there was good intrasession repeatability, regardless of whether the first two tests were compared or the two tests with the largest sensitivity difference were compared.
Sensitivity difference between the two tests with the largest difference in sensitivity compared with the mean sensitivity for these two tests. The horizontal dashed line represents the overall mean sensitivity difference between the two tests, whereas the gray lines represent the 95% limits of repeatability.
Figure 4 plots the mean overall sensitivity value for tests 1 and 2 combined as a function of age for each subject. The data were fit with a linear regression line with a slope of −0.05 and a y-intercept of 18.73 (solid line in Figure 4). Although the slope of the line was shallow, it was significantly different from zero (t=−3.64, P<0.01), indicating that there is approximately a 0.5 dB sensitivity loss for each decade of life.
Discussion
In the present study, macular sensitivity of 32 normal subjects was evaluated with a SD-OCT/SLO microperimeter. The OPKO microperimeter has been used by other investigators to evaluate patients with various retinal disorders and glaucoma.11, 12 The device used in our study not only enables the operator to evaluate macular sensitivity, but also to view high resolution SLO infrared images during testing and observe, in vivo, responses from the macular area. Following testing, the instrument superimposes perimetric sensitivity values on an SLO infrared image, thus offering the opportunity to view and correlate functional responses with anatomical structures. The clinical value of overlaying microperimetry responses on an SLO infrared image is demonstrated by a clinical example of a Stargardt patient shown in Figure 5. Retinal regions that appear hypopigmented, with poorly defined borders on fundus examination, present as hyporeflective (dark) zones with well defined borders on SLO infrared imaging. In addition, the software of the device provides a topographic map of the macula that shows the thickness values of the retina in every test point location, enabling direct correlations of functional responses with areas of either retinal thickening or thinning.
Our results showed a relatively narrow range of sensitivity fluctuation with the SD-OCT/SLO microperimeter. None of the subjects showed a difference in overall mean sensitivity between the first two tests >1.5 dB, and the 95% limits of repeatability did not exceed 3 dB . The mean sensitivity difference between the two tests was small, particularly in light of the 2 dB step size of the threshold algorithm. For subjects with higher overall macular sensitivity, the differences between the first two tests were even smaller, typically <1 dB. Of note, when considering individual test locations rather than the overall mean sensitivity, 91.3% of the test locations evaluated (for all subjects) showed less than ±2 dB difference between the first two tests. Repeatability of responses in psychophysical tests is an important issue and our results suggest that the SD-OCT/SLO microperimeter shows a narrow range of intrasession fluctuation, at least in our cohort of normal subjects. Nonetheless, it is conceivable that the range of fluctuation may be greater in patients with retinal disease, as it has been demonstrated that the variability of responses in psychophysical tests can be greater in patients than in normal subjects.7 This result is consistent with Figure 2, which shows that although the overall sensitivity difference between the two tests was ∼0.13 dB, regardless of the mean sensitivity of the two tests, the intrasession variability increased as the mean sensitivity decreased.
Of interest, in our study, the sensitivity values did not show significant differences between the inner circle of the test grid (more central) and the outer circles. This finding differs from what was observed in other studies,6, 13 where the highest sensitivity values were achieved in the central visual field and sensitivity decreased towards the periphery. However, there was a nonstatistically significant trend for sensitivity to be higher in the central circle when a small (0.66°) red spot was used as a fixation target in comparison to those obtained when either a white cross or a green spot (both 3.3°) was used (Mann–Whitney, P=0.10). Despite not reaching statistical significance, this finding suggests that the size of the fixation target used might have had an impact on the sensitivity measurements of the central circle in some subjects. Subjects tested with the white cross reported that it caused a ‘bleaching’ effect and also that the projected stimuli were presented from within the fixation target as a negative (dark) stimulus. Although we used different fixation targets among subjects, the mean fixation was stable for all subjects (average of 90.6% within a 2° diameter circle).
Comparison of the sensitivity values as a function of age showed that mean sensitivity decreased with age. For the subjects in the present study, a loss of mean sensitivity of ∼0.5 dB per decade was found. Although this value is slightly higher than that reported in similar studies using the MP-1,6, 8 the loss of sensitivity with age is minimal, compared with the 2 dB step size of the threshold algorithm. In future studies, it would be useful to expand upon the number of normal subjects within various decades being evaluated.
In summary, intrasession repeatability and normative sensitivity values were obtained using a SD-OCT/SLO microperimetry device, which allows for a direct correlation of structural abnormalities with functional defects. These features can assist clinicians in monitoring the natural history of structural and functional loss in macular diseases and the response to treatment. The establishment of a normative database for sensitivity values and intrasession repeatability will be useful for interpreting visual function loss in patients with various macular disorders.

References
Mainster MA, Timberlake GT, Webb RH, Hughes GW . Scanning laser ophthalmoscopy. Clinical applications. Ophthalmology 1982; 89: 852–857.
Timberlake GT, Mainster MA, Webb RH, Hughes GW, Trempe CL . Retinal localisation of scotomata by scanning laser ophthalmoscopy. Invest Ophthalmol Vis Sci 1982; 22: 91–97.
Sunness JS, Schuchard RA, Shen N, Rubin GS, Dagnelie G, Haselwood DM . Landmark-driven fundus perimetry using the scanning laser ophthalmoscope. Invest Ophthalmol Vis Sci 1995; 36: 1863–1874.
Schneider U, Inhoffen W, Gelisken F, Kreissig I . Assessment of visual function in choroidal neovascularisation with scanning laser microperimetry and simultaneous indocyanine green angiography. Graefes Arch Clin Exp Ophthalmol 1996; 234: 612–617.
Rohrschneider K, Springer C, Bultman S, Volcker HE . Microperimetry-comparison between the microprimeter 1 and the scanning laser ophthalmoscope-fundus perimetry. Am J Ophthalmol 2005; 139: 125–134.
Shah VA, Chalam KV . Values for macular perimetry using the MP-1 microperimeter in normal subjects. Ophthalmic Res 2009; 41: 9–13.
Chen FK, Patel PJ, Xing W, Bunce C, Egan C, Tufail AT et al. Test-retest variability of microperimetry using Nidek MP-1 in patients with macular disease. Invest Ophthlmol Vis Sci 2009; 50: 3464–3472.
Midena E, Vujosevic S, Cavarzeran F, Microperimetry Study Group. Normal values for fundus perimetry with the microperimeter MP1. Ophthalmology 2010; 117 (8): 1571–1576, 1576.e1. Epub 15 May 2010.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1: 307–310.
Bland JM, Altman DG . Measuring agreement in method comparison studies. Stat Methods Med Res 1999; 8: 135–160.
Landa G, Rosen RB, Garcia PMT, Seiple WH . Combined three-dimensional spectral OCT/SLO topography and microperimetry: steps toward achieving functional spectral OCT/SLO. Ophthalmic Res 2010; 43: 92–98.
Lima VC, Prata TS, De Moraes CG, Kim J, Seiple W, Rosen RB et al. A comparison between microperimetry and standard achromatic perimetry of the central visual field in eyes with glaucomatous paracentral visual-field defects. Br J Ophthalmol 2010; 94: 64–67.
Rohrschneider K, Becker M, Schumacher N, Fendrich T, Völcker HE . Normal values for fundus perimetry with the scanning laser ophthalmoscope. Am J Ophthalmol 1998; 126: 52–58.
Acknowledgements
Foundation Fighting Blindness, Owing Mills, Maryland, and Grant Healthcare Foundation, Chicago, Illinois (GAF); NIH core Grant EY01792; NIH research Grant EY019510 (JJM) and an unrestricted departmental grant from Research to Prevent Blindness.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Anastasakis, A., McAnany, J., Fishman, G. et al. Clinical value, normative retinal sensitivity values, and intrasession repeatability using a combined spectral domain optical coherence tomography/scanning laser ophthalmoscope microperimeter. Eye 25, 245–251 (2011). https://doi.org/10.1038/eye.2010.158
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2010.158
Keywords
This article is cited by
-
Evaluation of the microperimetry in eyes with cuticular drusen
Scientific Reports (2022)
-
Test–retest variability of microperimetry in geographic atrophy
International Journal of Retina and Vitreous (2020)
-
Longitudinal comparison of visual acuity as measured by the ETDRS chart and by the potential acuity meter in eyes with macular edema, and its relationship with retinal thickness and sensitivity
Eye (2014)