Abstract
Aim
To describe the optical coherence topographic (OCT) characteristics and outcome of vitrectomy with triamcinolone acetonide (TA)-assisted epiretinal tissue removal and gas tamponade in eyes with myopic foveoschisis (MF).
Methods
We examined 101 myopic eyes, and the OCT characteristics of 18 eyes (18%) with an MF were studied. Six eyes underwent vitrectomy with TA-assisted epiretinal tissue removal and gas tamponade. The postoperative outcome measures were best-corrected visual acuity (BCVA), resolution of the MF as determined by OCT, and complications.
Results
OCT scans showed an isolated MF in three (17%) eyes, and the MF were associated with two or more macular anomalies in 15 (83%) eyes. A foveal detachment was found in 13 (72%), lamellar macular hole in 4 (22%), and a tractional epimacular membrane in 11 (61%) of the 18 eyes. Six eyes underwent surgery, in which the epiretinal tissue was made visible by intravitreal TA and completely removed. The median BCVA significantly improved from 20/400 preoperatively (range, 20/1000–20/160) to 20/160 postoperatively (range, 20/200–20/40; P=0.03, Wilcoxon signed-rank test). The mean VA improved by 5.6 lines. OCT showed a complete reattachment of the fovea in four (67%) eyes and a small subfoveal or parafoveal detachment in two (33%) eyes.
Conclusions
MF is commonly observed in highly myopic eyes and most are associated with one or more macular anomalies. Vitrectomy with TA-assisted complete removal of all tractional premacular structures followed by gas tamponade resulted in good visual and anatomical outcomes for treating MF.
Similar content being viewed by others
Introduction
Macular retinoschisis in highly myopic eyes is also known as myopic foveoschisis (MF). The prevalence, characteristics, and evolution of MF have been studied extensively since the first description by Takano and Kishi.1, 2, 3, 4, 5, 6, 7 MF is important because it has been postulated to precede the formation of a macular hole retinal detachment, which leads to a marked decrease in vision.
Traction on the retina by an epimacular structure in association with an elongation of the axial length, thinning of the retina, and a weak retinal adhesion at the posterior staphyloma has been considered to contribute to the formation of an MF. However, the pathogenesis of MF is still undetermined.
Surgical results have been fairly successful in treating and preventing the progression of an MF. However, the best surgical procedures remain to be determined.7, 8, 9, 10, 11, 12 Triamcinolone acetonide (TA) has been used during the vitrectomy for macular hole retinal detachments to make epiretinal membranes (ERMs) and the posterior vitreous cortex more visible. The increased visibility facilitates the complete removal of the ERMs and posterior hyaloid.13
The purpose of this study was to determine the OCT characteristics of 18 eyes with an MF and to evaluate the outcomes after vitrectomy with TA-assisted ERM removal and gas tamponade on six of these eyes.
Patients and methods
Data collection
We prospectively examined 101 highly myopic eyes of 54 consecutive patients (19 men and 35 women) who visited our eye centre with or without visual symptoms, for example, blurring of vision and central metamorphopsia, from April 2006 to August 2007. Approval of the study was obtained from the Ethics Committee of the School of Medicine, Zhejiang University, and the procedures conformed to the tenets of the Declaration of Helsinki.
The mean age of the patients was 53.7±9.9 years (±SD) with a range of 37 to 73 years. The mean refractive error in spherical equivalents was −13.9±4.9 D with a range of −6.5 to −23.0 D. The mean axial length was 28.1±1.7 mm with a range of 26.0–32.5 mm.
All patients underwent a standard ophthalmologic examination including, best-corrected Snellen visual acuity (BCVA), intraocular pressure measurement, slit-lamp examination of the anterior segment, fundus biomicroscopy, refractive examination, bidimensional ultrasonography, and colour photographs of the fundus. The status of the vitreous was determined by slit-lamp biomicroscopy.
After the standard ophthalmic evaluation, all patients were examined by OCT 3000 (Stratus OCT; Carl Zeiss Meditee, Dublin, CA, USA). Cross-sectional images of the posterior pole were obtained by six radial scans of 6 mm centred on the fovea. This was equivalent to one scan/30° of retina. The 8-mm scans were also performed in some of the eyes.
Surgical techniques
Six of the eyes with an MF had a progressive decrease of the VA and underwent standard 20-gauge, three port pars planar vitrectomy. Informed consent was obtained from all patients before surgery. Simultaneous phacoemulsification was performed on eyes with a cataract. A posterior vitreous detachment (PVD) was created by active aspiration in eyes without a PVD. Any visible vitreous was cut and removed with the vitrectomy probe.
A microhooked needle (20 gauge) was used to create a flap of the epiretinal tissue along the posterior retinal surface with the assistance of an intravitreal injection of TA (0.1 ml of 4 mg/0.1 ml; Kenalog-40, Bristol–Meyers Squibb). The preparation of the TA suspension has been described in detail.13 Then a horizontal forceps was used to grasp the flap, and the epiretinal tissure was removed in a curvilinear fashion from the retina. The residual epiretinal tissue around the staphyloma and posterior hyaloid was lifted by suction of the vitrectomy probe and cut as far peripherally as possible. The ILM was not intentionally peeled. The peripheral retina was carefully examined for retinal breaks with scleral depression. Laser photocoagulation was performed if a retinal break was found.
Fluid-air exchange was then performed, and then 14% perfluoropropane (C3F8) was injected to tamponade the retina. After surgery, all of the patients were instructed to maintain a face-down position as long as possible during the first 2 weeks.
The excised epimacular tissues from three eyes were fixed in 2% glutaraldehyde in 0.1 M phosphate buffer for the transmission electron microscopy (TEM).
The follow-up period ranged from 5 to 14 months. The postoperative outcome measures included BCVA, resolution of the MF as determined by OCT, and the postoperative complications.
Statistical analyses were performed with SPSS for Windows version 13.0 (SPSS Inc., Chicago, IL, USA). The BCVA was converted to logarithm of the minimum angle of resolution (logMAR) units for the analyses. Non-parametric Wilcoxon signed-rank test was used to analyse the pre- and postoperative BCVA. A P-value <0.05 was considered statistically significant.
Results
Data of patients with MF
An MF was found in 18 eyes of 11 patients and seven (63%) were bilateral. The clinical characteristics of patients with MF are shown in Table 1.
OCT Characteristics of MF
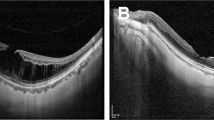
OCT scans disclosed a marked increase in the thickness of the retina in the posterior pole area in all 18 eyes. An outer retinoschisis with intraretinal columns was detected in 18 (100%) eyes and an inner retinoschisis in 8 (44%) of the 18 eyes. An isolated MF was observed in three (17%) eyes (Figure 1a).
Optic coherence tomograms of different eyes with myopic foveoschisis (MF). All scans were made in the horizontal meridian and 8 mm length. (a) An outer and inner retinoschisis. Inter-retinal columns are present in both the outer (long arrow) and inner (short arrow) retinoschisis. (b) An outer retinoschisis (arrow), a foveal detachment (asterisk), and epiretinal tractional tissue (arrowhead). (c) An outer retinoschisis (arrow), a foveal detachment (asterisk), and a lamellar macular hole (short arrow).
In 15 (83%) eyes, the MF was associated with one or more macular abnormalities; a foveal detachment was noted in 13 (72%) eyes (Figure 1b) and a lamellar macular hole was noted in 4 (22%) of the 18 eyes (Figure 1c). Tractional epimacular tissue was observed in 11 (61%) of the 18 eyes (Figure 1b; Table 1).
Intraoperative observations
The vision in six eyes of six patients with an MF progressively decreased and underwent vitrectomy. The patients of the remaining 12 eyes preferred to undergo a clinical observation. Vitrectomy was performed in five and simultaneous phacoemulsification without posterior chamber intraocular lens implantation was performed in one of the six eyes. During the vitrectomy, one case required a creation of a PVD by active aspiration (case 1 in Table 2), and in the other five eyes, a large posterior liquified cavity was present. Any visible vitreous was removed with the vitrectomy probe.
After the intravitreal injection of TA, a thin sheet of epiretinal tissue overlying the macular and posterior staphyloma area was made clearly visible by the white TA granules. The membrane was completely removed as a whole sheet in five eyes. The epiretinal tissue was found to extend towards the very thin posterior hyaloid beyond the staphyloma area. The residual epiretinal tissue and posterior hyaloid were lifted by suction from the vitrectomy probe and removed as far peripherally as possible. No intraoperative complications were observed during the surgery.
Visual and anatomical outcomes
The pre- and postoperative details of the six MF eyes that underwent vitrectomy are shown in Table 2. The mean postoperative follow-up period was 11.7±5.2 months (range, 5–14 months). Postoperatively, all eyes had an improvement in the visual symptoms. The median preoperative BCVA was 20/400 (range, 20/1000–20/160), and the final median postoperative BCVA significantly improved to 20/160 (range, 20/200–20/40; Wilcoxon signed-rank test, P=0.03). The mean improvement in the BCVA was 5.6 lines (range 3–7 lines).
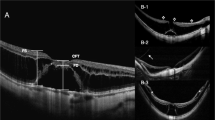
The postoperative OCT showed a complete resolution of the MF with complete foveal reattachment in four eyes (67%; Figure 2b). In the other two (33%) eyes, a complete reattachment of the MF was obtained, but a small subfoveal or parafoveal detachment persisted. In one eye, a minor parafoveal fold with peaks pointing to the vitreous cavity was observed (Figures 3 and 4).
Pre- and postoperative optic coherence tomograms of case 2. (a) The preoperative 6-mm horizontal scan of the macula showing an extensive foveal detachment (asterisk) and epiretinal tractional tissue (arrowheads). The BCVA was 20/1000. (b) Three months after surgery, a complete foveal reattachment and the resolution of the retinoschisis can be seen. The BCVA improved to 20/160.
Pre- and postoperative optic coherence tomograms of case 1. (a) The preoperative 6-mm horizontal scan of the macula showing an outer and inner retinoschisis (arrow) with a foveal retinal detachment (asterisk). The BCVA was 20/200. (b) Two months after vitrectomy, the outer and inner retinoschisis has regressed. The BCVA was 20/160. (c) Five months after vitrectomy, the inner and outer retinoschisis has nearly disappeared. The centre of the foveola is reattached; however, a small parafoveal retinal detachment still exists with a minor fold with the peaks pointing to the vitreous cavity (arrow). The BCVA was 20/40. (d) Ten months after vitrectomy, the OCT image is similar to the one shown in panel c. The BCVA was 20/40.
Pre- and postoperative optic coherence tomograms of case 3. (a) The preoperative 6-mm horizontal scan of the macula showing an outer retinoschisis (arrow) with a foveal retinal detachment (asterisk). Premacular tractional tissue (arrowheads) is present. The BCVA was 20/160. (b) One month after vitrectomy, foveal retinoschisis has completely regressed. A very shallow subfoveal detachment is still present. The BCVA improved to 20/80.
Postoperative complications
Two patients (cases 1 and 2 in Table 2) developed nuclear sclerosis at 5 and 12 months after surgery. Cataract surgery was not performed because of insignificant visual decrease.
TEM
TEM showed that the excised epiretinal tissues from the three eyes were made up of fibroblast-like cells, for example, elongated cells with large nuclei and small amount of cytoplasm, collagen matrix, and a very thin posterior hyaloid. Tissues resembling the ILM were not detected in any of the three excised tissues (Figure 5).
Transmission electron microscopy of the excised specimens (a and b). The excised epiretinal tissue is made up of fibroblast-like cells (arrows in panels a and b, elongated cell shape with large nuclear and small cytoplasm), the collagen matrix (asterisk in panel a) and a very thin posterior hyaloid (arrowheads in panel b). Tissues resembling the ILM were not detected.
Discussion
In all, 18 of 101 (18%) highly myopic eyes had an MF as determined by OCT. An outer retinoschsis was found in 18 (100%), inner retinoschisis in 8 (44%), a foveal detachment in 14 (78%), a lamellar macular hole in 4 (22%), and premacular tractional tissue in 11 (61%) of the 18 eyes. An isolated MF was found in only 3 (17%) of 18 eyes. Taken together with published results, an MF seems to be a relatively common complication in highly myopic eyes and is mostly associated with one or more macular abnormalities.1, 2, 3, 4, 5, 6, 11
The degree of visual impairment in patients with an MF varied considerably. It has been shown that an MF can remain stable in some eyes for many years without affecting the vision. However, the combination of MF with a foveal detachment or premacular structures is indicative for poor prognosis.2, 7 Gaucher et al7 examined 29 eyes with an MF and reported that the 10 of 20 eyes that worsened had a premacular structure. In addition, six of nine eyes that evolved into a macular hole had a foveal detachment during the follow-up period of 31.2 months. Benhamou et al2 reported that among 21 eyes, two of four MF eyes with an epiretinal structure developed into a full-thickness macular hole after a follow-up period of more than 12 months. Thus, an MF has been postulated to precede the formation of a macular hole in highly myopic eyes.
A very high prevalence of epimacular tractional tissue has been noted in eyes with an MF in our and other reported series.2, 7 Thus, there is a rationale to perform vitrectomy and peel the epimacular tractional tissue in an attempt to treat and prevent the progression of an MF.
An accurate identification of an epiretinal structure is essential for its complete removal. Most epiretinal tissues are not clearly visible during surgery and might be overlooked or left attached to the retina. Even though experienced retinal surgeons can detect epiretinal tissue, it is still technically difficult to differentiate the border between the epiretinal structure and the underlying retina. However, the injected TA granules that become stuck to the rough surface of the epiretinal tissue overlying the macula and posterior staphyloma area, and the residual vitreous made the structures clearly visible. This ensured the complete removal of the epiretinal tissue and the posterior hyaloid.
The epiretinal tissue was found intraoperatively to extend towards the very thin posterior hyaloid around the staphyloma in the periphery. Our observations are consistent with the findings of our earlier study.13 The presence of an ERM and posterior hyaloid in highly myopic eyes with a macular hole retinal detachment was mostly noted during vitrectomy even in eyes with a complete PVD. The epiretinal tissue was postulated to be the posterior wall of the posterior precortical vitreous pocket and some proliferating cells.13, 14, 15, 16
ILM peeling during vitrectomy is still controversial; similar anatomical and visual outcomes have been obtained with9, 10, 17 and without ILM removal.7, 11 Gaucher et al7 reported that the visual improvement was statistically significant with logMAR values from 0.97 to 0.63 before and after surgery, respectively, without ILM removal. Kwok et al11 reported that the median BCVA improved from 20/80 to 20/50 and the mean line of visual improvement was 3.6 lines after surgery without ILM removal. In our case series, the mean BCVA improved by 5.6 lines; however, the median postoperative BCVA was 20/160. The lower postoperative BCVA might be attributable to the poor preoperative BCVA (20/400, median) in our study. The removal of the ILM in eyes with an MF was assumed to ensure complete removal of any overlying residual vitreous cortex and ERM, collagen fibre, and cellular components. This should lead to a better conformation of the retina to the posterior staphyloma as in the cases of an idiopathic ERM and a macular hole.18, 19, 20 However, ILM removal in highly myopic eyes is technically challenging because of its transparency and fragility. In addition, ILM peeing during vitrectomy for an MF may be a risk causing a macular hole.9, 16
Intravitreal TA ensured the complete removal of the epiretinal tissue and the posterior vitreous cortex as a whole sheet. TEM of the three excised epiretinal tissues in our study showed fibroblast-like cells, collagen matrix, and a very thin posterior hyaloid. No ILM was observed. Our results, in combination with published reports, suggest that vitrectomy without ILM peeling may be useful for the treatment of MF eyes. However, more controlled studies and longer follow-up periods are needed to support our conclusions.
A very shallow subfoveal or parafoveal retinal detachment persisted in two eyes during the follow-up; one was a parafoveal minor fold with the peaks pointing to the vitreous cavity. The incidence of a parafoveal minor fold was reported to be 24, 43, and 62% after 1, 3, and 6 months, respectively in 21 highly myopic eyes with an MF even with ILM peeling.21 After a closer examination of three-dimensional OCT images, the investigators suggested that the minor folds might result from a weak traction caused by an imbalance in the extension of retinal vessels and retinal tissues during the development of a posterior staphyloma.
An evolution into macular hole has been reported in eyes with an MF even after undergoing vitrectomy. Gaucher et al7 reported that three of 11 MF eyes developed a macular hole after vitrectomy. None of the six eyes in our cases evolved into a macular hole during the follow-up. TA-associated elevated intraocular pressure was not found in any of our cases.
In conclusion, MF is commonly observed in highly myopic eyes and most are associated with one or more macular anomalies. Vitrectomy with TA-assisted complete removal of all tractional premacular structures followed by gas tamponade resulted in good visual and anatomical outcomes for treating MF.
References
Takano M, Kishi S . Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol 1999; 128: 472–476.
Benhamou N, Massin P, Haouchine B, Erginay A, Gaudric A . Macular retinoschisis in highly myopic eyes. Am J Ophthalmol 2002; 133: 794–800.
Baba T, Ohno-Matsui K, Futagami S, Yoshida T, Yasuzumi K, Kojima A et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol 2003; 135: 338–342.
Panozzo G, Mercanti A . Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol 2004; 122: 1455–1460.
Shimada N, Ohno-Matsui K, Baba T, Futagami S, Tokoro T, Mochizuki M . Natural course of macular retinoschisis in highly myopic eyes without macular hole or retinal detachment. Am J Ophthalmol 2006; 142: 497–500.
Wu PC, Chen YJ, Chen YH, Chen CH, Shin SJ, Tsai CL et al. Factors associated with foveoschisis and foveal detachment without macular hole in high myopia. Eye 2007 (in press).
Gaucher D, Haouchine B, Tadayoni R, Massin P, Erginay A, Benhamou N et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol 2007; 143: 455–462.
Ikuno Y, Tano Y . Vitrectomy for macular holes associated with myopic foveoschisis. Am J Ophthalmol 2006; 141: 774–776.
Kobayashi H, Kishi S . Vitreous surgery for highly myopic eyes with foveal detachment and retinoschisis. Ophthalmology 2003; 110: 1702–1707.
Ikuno Y, Sayanagi K, Ohji M, Kamei M, Gomi F, Harino S et al. Vitrectomy and internal limiting membrane peeling for myopic foveoschisis. Am J Ophthalmol 2004; 137: 719–724.
Kwok AK, Lai TY, Yip WW . Vitrectomy and gas tamponade without internal limiting membrane peeling for myopic foveoschisis. Br J Ophthalmol 2005; 89: 1180–1183.
Baba T, Yanaka S, Maesawa A, Teramatsu T, Noda Y, Yamamoto S . Scleral buckling with macular plombe for eyes with myopic macular retinoschisis and retinal detachment without macular hole. Am J Ophthalmol 2006; 142: 483–487.
Fang X, Zheng X, Weng Y, Chen Z, Liu J, Chen B et al. Anatomical and visual outcome after vitrectomy with triamcinolone acedonide-assisted epiretinal membrane removal in highly myopic eyes with retinal detachment due to macular hole. Eye 2007 (in press).
Tamura T, Kishi S . Membranous nature of premacular vitreous cortex in the human eye. Jpn J Ophthalmol 1996; 40: 181–186.
Ishida S, Yamazaki K, Shinoda K, Kawashima S, Oguchi Y . Macular hole retinal detachment in highly myopic eyes: ultrastructure of surgically removed epiretinal membrane and clinicopathologic correlation. Retina 2000; 20: 176–183.
Spaide RF, Fisher Y . Removal of adherent cortical vitreous plaques without removing the internal limiting membrane in the repair of macular detachments in highly myopic eyes. Retina 2005; 25: 290–295.
Kanda S, Uemura A, Sakamoto Y, Kita H . Vitrectomy with internal limiting membrane peeling for macular retinoschisis and retinal detachment without macular hole in highly myopic eyes. Am J Ophthalmol 2003; 136: 177–180.
Bando H, Ikuno Y, Choi TS, Tano Y, Yamanaka I, Ishibashi T . Ultrastructure of internal limiting membrane in myopic foveoschisis. Am J Ophthalmol 2005; 139: 197–199.
Sayanagi K, Ikuno Y, Tano Y . Reoperation for persistent myopic foveoschisis after primary vitrectomy. Am J Ophthalmol 2006; 141: 414–417.
Fang X, Chen Z, Weng Y, Shu Z, Ni H, Jiang J et al. Surgical outcome of idiopathic macular epiretinal membrane in young patients. Eye 2007 (in press).
Ikuno Y, Gomi F, Tano Y . Potent retinal arteriolar traction as a possible cause of myopic foveoschisis. Am J Ophthalmol 2005; 139: 462–467.
Acknowledgements
This study was supported by a grant from the National Natural Science Foundation (No. 60671005), China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interests: None
Rights and permissions
About this article
Cite this article
Fang, X., Weng, Y., Xu, S. et al. Optical coherence tomographic characteristics and surgical outcome of eyes with myopic foveoschisis. Eye 23, 1336–1342 (2009). https://doi.org/10.1038/eye.2008.291
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2008.291
Keywords
This article is cited by
-
Vitreoretinal Interface Changes After Anti-vascular Endothelial Growth Factor Treatment in Highly Myopic Eyes: A Real-World Study
Ophthalmology and Therapy (2023)
-
Vitrectomy with internal limiting membrane peeling and gas tamponade for myopic foveoschisis
BMC Ophthalmology (2022)
-
Anatomical and visual outcomes of fovea-sparing internal limiting membrane peeling with or without inverted flap technique for myopic foveoschisis
BMC Ophthalmology (2022)
-
Long-term surgical outcomes and prognostic factors of foveal detachment in pathologic myopia: based on the ATN classification
BMC Ophthalmology (2022)
-
Long-term results and risk factors influencing outcome of gas tamponade for myopic foveoschisis with foveal detachment
Eye (2020)