Abstract
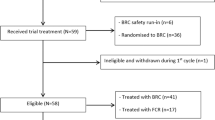
Busulfan (BU) has a narrow therapeutic window and the average concentration of BU at steady state (Css) is critical for successful engraftment in children receiving BU as part of the preparative regimen for allogeneic transplants. Sixteen patients with sickle cell disease (SCD) underwent allogeneic bone marrow transplant (BMT) from HLA-identical siblings. The preparative regimen consisted of intravenous BU 0.8–1 mg/kg/dose for 16 doses, cytoxan (CY) of 50 mg/kg daily for four doses and equine anti-thymocyte globulin (ATG) 30 mg/kg daily for three doses. BU levels were adjusted to provide a total exposure Css of 600–700 ng/mL. The median age at the time of transplant was 6.2 years (range 1.2–19.3). Fourteen (87%) patients required adjustment of the BU dose to achieve a median Css of 652 ng/mL (range 607–700). All patients achieved neutrophil and platelet engraftment without significant toxicity. Median donor engraftment at the last follow-up was 100% (range 80–100). None of the patients experienced sickle cell-related complications post transplant. With a median follow-up of 3 years (range 1.3–9), the event-free survival (EFS) and overall survival (OS) are both 100%. We conclude that targeting of BU Css between 600 and 700 ng/mL in this regimen can result in excellent and sustained engraftment in young patients with SCD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Hulbert ML, McKinstry RC, Lacey JL, Moran CJ, Panepinto JA, Thompson AA et al. Silent cerebral infarcts occur despite regular blood transfusion therapy after first strokes in children with sickle cell disease. Blood 2011; 117: 772–779.
Locatelli F, Pagliara D . Allogeneic hematopoietic stem cell transplantation in children with sickle cell disease. Pediatr Blood Cancer 2012; 59: 372–376.
Vermylen C, Cornu G, Ferster A, Brichard B, Ninane J, Ferrant A et al. Haematopoietic stem cell transplantation for sickle cell anaemia: the first 50 patients transplanted in Belgium. Bone Marrow Transplant 1998; 22: 1–6.
Walters MC, Patience M, Leisenring W, Eckman JR, Scott JP, Mentzer WC et al. Bone marrow transplantation for sickle cell disease. N Engl J Med 1996; 335: 369–376.
Bernaudin F, Socie G, Kuentz M, Chevret S, Duval M, Bertrand Y et al. Long-term results of related myeloablative stem-cell transplantation to cure sickle cell disease. Blood 2007; 110: 2749–2756.
Panepinto JA, Walters MC, Carreras J, Marsh J, Bredeson CN, Gale RP et al. Matched-related donor transplantation for sickle cell disease: report from the Center for International Blood and Transplant Research. Br J Haematol 2007; 137: 479–485.
Bolinger AM, Zangwill AB, Slattery JT, Glidden D, DeSantes K, Heyn L et al. An evaluation of engraftment, toxicity and busulfan concentration in children receiving bone marrow transplantation for leukemia or genetic disease. Bone Marrow Transplant 2000; 25: 925–930.
DeLeve LD, Shulman HM, McDonald GB . Toxic injury to hepatic sinusoids: sinusoidal obstruction syndrome (veno-occlusive disease). Semin Liver Dis 2002; 22: 27–42.
McCune JS, Gooley T, Gibbs JP, Sanders JE, Petersdorf EW, Appelbaum FR et al. Busulfan concentration and graft rejection in pediatric patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant 2002; 30: 167–173.
Slattery JT, Risler LJ . Therapeutic monitoring of busulfan in hematopoietic stem cell transplantation. Ther Drug Monit 1998; 20: 543–549.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J et al1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant 1995; 15: 825–828.
Grochow LB, Krivit W, Whitley CB, Blazar B . Busulfan disposition in children. Blood 1990; 75: 1723–1727.
Bolinger AM, Zangwill AB, Slattery JT, Risler LJ, Sultan DH, Glidden DV et al. Target dose adjustment of busulfan in pediatric patients undergoing bone marrow transplantation. Bone Marrow Transplant 2001; 28: 1013–1018.
Nguyen L, Fuller D, Lennon S, Leger F, Puozzo C . I.V. busulfan in pediatrics: a novel dosing to improve safety/efficacy for hematopoietic progenitor cell transplantation recipients. Bone Marrow Transplant 2004; 33: 979–987.
Michel G, Valteau-Couanet D, Gentet JC, Esperou H, Socie G, Mechinaud F et al. Weight-based strategy of dose administration in children using intravenous busulfan: clinical and pharmacokinetic results. Pediatr Blood Cancer 2012; 58: 90–97.
Nagasawa M, Mitsuiki N, Ono T, Takagi M, Oda H, Yasuhara M et al. Pharmacokinetic monitoring is still required for intravenous busulfan in SCT for small children. Int J Hematol 2010; 91: 728–730.
Veal GJ, Nguyen L, Paci A, Riggi M, Amiel M, Valteau-Couanet D et al. Busulfan pharmacokinetics following intravenous and oral dosing regimens in children receiving high-dose myeloablative chemotherapy for high-risk neuroblastoma as part of the HR-NBL-1/SIOPEN trial. Eur J Cancer 2012; 48: 3063–3072.
McPherson ME, Hutcherson D, Olson E, Haight AE, Horan J, Chiang KY . Safety and efficacy of targeted busulfan therapy in children undergoing myeloablative matched sibling donor BMT for sickle cell disease. Bone Marrow Transplant 2011; 46: 27–33.
Walters MC, Hardy K, Edwards S, Adamkiewicz T, Barkovich J, Bernaudin F et al. Pulmonary, gonadal, and central nervous system status after bone marrow transplantation for sickle cell disease. Biol Blood Marrow Transplant 2010; 16: 263–272.
Acknowledgements
We would like to thank Alisha McCord and Ryan Frangoul for the administrative support. This project was supported by the Carolyn Perot Rathjen Chair in Pediatrics, Nashville, TN, USA (Haydar Frangoul, MD).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Maheshwari, S., Kassim, A., Yeh, R. et al. Targeted Busulfan therapy with a steady-state concentration of 600–700 ng/mL in patients with sickle cell disease receiving HLA-identical sibling bone marrow transplant. Bone Marrow Transplant 49, 366–369 (2014). https://doi.org/10.1038/bmt.2013.188
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2013.188
Keywords
This article is cited by
-
Review of the Pharmacokinetics and Pharmacodynamics of Intravenous Busulfan in Paediatric Patients
Clinical Pharmacokinetics (2021)
-
Busulfan systemic exposure and its relationship with efficacy and safety in hematopoietic stem cell transplantation in children: a meta-analysis
BMC Pediatrics (2020)
-
Population pharmacokinetics of busulfan in Saudi pediatric patients undergoing hematopoietic stem cell transplantation
International Journal of Clinical Pharmacy (2020)