Abstract
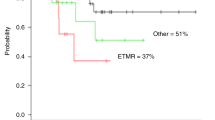
Germ cell tumors carry an excellent prognosis with platinum-based therapy upfront. The patients who either relapse or demonstrate refractoriness to platinum pose a challenge. There exist many reports in the literature on the use of high-dose chemotherapy and stem cell rescue improving the outcome in patients with relapsed germ cell tumors. However, the reports have great variability in the patient selection, prior treatments, the choice of the conditioning regimen and variability of the doses within the same regimen. In this report, we present 37 patients who underwent a uniform protocol of high-dose chemotherapy with stem cell rescue. Stem cell mobilization was performed with high-dose CY (4 g per m2) and we were able to collect adequate cells for marrow rescue in all patients. Patients received a high-dose regimen with etoposide (800 mg/m2 per day) days −6, −5 and −4 as a continuous infusion, carboplatin (667 mg/m2 per day) on days −6, −5 and −4 as a 1 h infusion, and CY (60 mg/kg per day) on days −3 and −2. In this high-risk group of patients, high-dose chemotherapy with autologous stem cell rescue led to a 3-year overall survival of 57% and a 3-year event-free survival of 49%. The results are reflective of a single procedure. No tandem transplants were performed. The treatment-related mortality was low at 3% in this heavily pretreated group.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Vaena D, Abonour R, Einhorn L . Long-term survival after high-dose salvage chemotherapy for germ cell malignancies with adverse prognostic variables. J Clin Oncol 2003; 15: 4100–4104.
Beyer J, Rick O, Siegert W, Bokemeyer C . Salvage chemotherapy in relapsed germ cell tumors. World J Urol 2001; 19: 90–93.
Rick O, Bokemeyer C, Beyer J, Hartmann J, Schwella N, Kingreen D et al. Salvage treatment with paclitaxel, ifosfamide, and cisplatin plus high-dose carboplatin, etoposide, and thiotepa followed by autologous stem-cell rescue in patients with relapsed or refractory germ cell cancer. J Clin Oncol 2001; 19: 81–88.
Einhorn LH, Williams SD, Chamness A, Brames MJ, Perkins SM, Abonour R . High-dose chemotherapy and stem-cell rescue for metastatic germ-cell tumors. N Engl J Med 2007; 357: 340–348.
Broun E, Nichols C, Gize G, Cornetta K, Hromas R, Schacht B et al. Tandem high dose chemotherapy with autologous bone marrow transplantation for initial relapse of testicular germ cell cancer. Cancer 1997; 79: 1605–1610.
Fosså S, Stenning S, Gerl A, Horwich A, Clark P, Wilkinson P et al. Prognostic factors in patients progressing after cisplatin-based chemotherapy for malignant non-seminomatous germ cell tumours. Br J Cancer 1999; 80: 1392–1399.
Loehrer PS, Lauer R, Roth B, Williams S, Kalasinski L, Einhorn L . Salvage therapy in recurrent germ cell cancer: ifosfamide and cisplatin plus either vinblastine or etoposide. Ann Intern Med 1998; 109: 540–546.
Motzer R, Nichols C, Margolin K, Bacik J, Richardson P, Vogelzang N et al. Phase III randomized trial of conventional-dose chemotherapy with or without high-dose chemotherapy and autologous hematopoietic stem-cell rescue as first-line treatment for patients with poor-prognosis metastatic germ cell tumors. J Clin Oncol 2007; 25: 247–256.
Chaudhary U, Damon L, Rugo H, Linker C, Navarro W, Small E . High-dose etoposide, thiotepa, and dose-adjusted carboplatin (TVCa) with autologous hematopoietic stem cell rescue as treatment of relapsed or refractory germ cell cancer. Am J Clin Oncol 2005; 28: 130–137.
Müller A, Ihorst G, Waller C, Dölken G, Finke J, Engelhardt M . Intensive chemotherapy with autologous peripheral blood stem cell transplantation during a 10-year period in 64 patients with germ cell tumor. Biol Blood Marrow Transplant 2006; 12: 355–365.
Lorch A, Kollmannsberger C, Hartmann T, Metzner B, Schmidt-Wolf I, Berdel W et al. Single vs high dose chemotherapy in patients with relapsed or refractory germ cell tumors: a prospective randomized multicenter trial of the German testicular cancer study group. J Clin Oncol 2007; 25: 2778–2784.
Motzer R, Mazumdar M, Bajorin D, Bosl G, Lyn P, Vlamis V . High-dose carboplatin, etoposide, and cyclophosphamide with autologous bone marrow transplantation in first-line therapy for patients with poor-risk germ cell tumors. J Clin Oncol 1997; 15: 2546–2552.
Motzer R, Mazumdar M, Bosl G, Bajorin D, Amsterdam A, Vlamis V . High-dose carboplatin, etoposide, and cyclophosphamide for patients with refractory germ cell tumors: treatment results and prognostic factors for survival and toxicity. J Clin Oncol 1996; 14: 1098–1105.
Mandanas R, Saez R, Epstein R, Confer D, Selby G . Long-term results of autologous marrow transplantation for relapsed or refractory male or female germ cell tumors. Bone Marrow Transplant 1998; 21: 569–576.
McNeish I, Kanfer E, Haynes R, Giles C, Harland S, Driver D et al. Paclitaxel-containing high-dose chemotherapy for relapsed or refractory testicular germ cell tumours. Br J Cancer 2004; 90: 1169–1175.
Hartmann T, Gauler T, Metzner B, Gerl A, Casper J, Rick O et al. Phase I/II study of sequential dose-intensified ifosfamide, cisplatin, and etoposide plus paclitaxel as induction chemotherapy for poor prognosis germ cell tumors by the German testicular cancer study group. J Clin Oncol 2007; 25: 5742–5747.
Rick O, Beyer J, Kingreen D, Schwella N, Krusch A, Schleicher J et al. High-dose chemotherapy in germ cell tumours: a large single centre experience. Eur J Cancer 1998; 34: 1883–1888.
Smith M, Rubinstein L, Ungerleider R . Therapy-related acute myeloid leukemia following treatment with epipodophyllotoxins: estimating the risks. Med Pediatr Oncol 1994; 23: 86–98.
Frisk P, Lönnerholm G, Oberg G . Disease of the liver following bone marrow transplantation in children: incidence, clinical course and outcome in a long-term perspective. Acta Paediatr 1998; 87: 579–583.
Barker C, Anderson R, Sauve R, Butzner J . GI complications in pediatric patients post-BMT. Bone Marrow Transplant 2005; 36: 51–58.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agarwal, R., Dvorak, C., Stockerl-Goldstein, K. et al. High-dose chemotherapy followed by stem cell rescue for high-risk germ cell tumors: the Stanford experience. Bone Marrow Transplant 43, 547–552 (2009). https://doi.org/10.1038/bmt.2008.364
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2008.364
Keywords
This article is cited by
-
Role of one, two and three doses of high-dose chemotherapy with autologous transplantation in the treatment of high-risk or relapsed testicular cancer: a systematic review
Bone Marrow Transplantation (2018)
-
Long-term follow-up of patients undergoing auto-SCT for advanced germ cell tumour: a multicentre cohort study
Bone Marrow Transplantation (2011)