Abstract
Background:
The importance of telomerase in multiple myeloma (MM) is well established; however, its response to bortezomib has not been addressed.
Methods:
The effect of bortezomib on telomerase activity and cell proliferation was evaluated in four MM cell lines and in myeloma cells obtained from eight patients. The mechanism of telomerase regulation on epigenetic, transcriptional, and post-translational levels was further assessed in two selected cell lines: ARP-1 and CAG. Clinical data were correlated with the laboratory findings.
Results:
Bortezomib downregulated telomerase activity and decreased proliferation in all cell lines and cells obtained from patients, albeit in two different patterns of kinetics. ARP-1 cells demonstrated higher and earlier sensitivity than CAG cells due to differential phosphorylation of hTERT by PKCα. Methylation of hTERT promoter was not affected. Transcription of hTERT was similarly inhibited in both lines by decreased binding of SP-1 and not of C-Myc and NFκB. The ex vivo results confirmed the in vitro findings and suggested existence of clinical relevance.
Conclusion:
Bortezomib downregulates telomerase activity in MM cells both transcriptionally and post-translationally. MM cells, both in vitro and in patients, exhibit different sensitivity to the drug due to different post-translational response. The effect of bortezomib on telomerase activity may correlate with resistance to bortezomib in patients, suggesting its potential utility as a pre-treatment assessment.
Similar content being viewed by others
Main
The ubiquitin–proteasome system has become a promising novel molecular target in cancer because of its critical role in cellular protein degradation and its interaction with cell cycle and regulation of apoptosis. It plays an important role in transcriptional regulation of the key transcription factor, nuclear factor-κB (NF-κB). The 26S proteasome, an adenosine triphosphate-dependent protease, is fundamental for the ubiquitin–proteasome pathway (Lenz, 2003). Proteasome inhibition is emerging as an effective treatment in several haematological malignancies, notably multiple myeloma (MM) (Anderson, 2004). Bortezomib is a 20S proteasome complex inhibitor that acts by disrupting various cell signalling pathways, thereby leading to cell cycle arrest, apoptosis, and inhibition of angiogenesis. The hallmark of bortezomib action is the inhibition of NFκB, thereby interfering with NFκB-mediated cell survival, tumour growth, and angiogenesis (Jackson et al, 2005). This is the first clinically used proteasome inhibitor and serves as an effective drug against MM. Although numerous of its cellular targets are well characterised, the whole spectrum of its targets is not yet fully understood.
The importance of telomerase in the biology and prognosis of many types of cancers in general and in MM specifically is well established (Akiyama et al, 2002; Akiyama et al, 2003). Telomerase is a unique reverse transcriptase, expressed almost exclusively in >90% of cancer cells. It synthesises TTAGGG repeats in telomeres, compensating for telomeric loss in each DNA replication (Blackburn and Collins, 2010). Telomerase activity confers endless replicative potential to the cancer cell. Owing to its essentiality and specificity to the malignant cells, it may serve as a valid anticancer drug target, and indeed active compounds that target telomerase are already in advanced phases of clinical trials (Shay and Wright, 2005). The importance of telomerase in MM has been demonstrated convincingly both in vitro and clinically. Telomerase activity has been found in myeloma cells of 90% of the newly diagnosed and relapsed patients, while only in 13% of patients in remission (Shiratsuchi et al, 2002). It is of prognostic value, as elevated activity of the enzyme is correlated with poor prognosis (Xu et al, 2001; Shiratsuchi et al, 2002; Gahrton, 2004). In addition, inhibition of telomerase activity has been shown to be effective in treating MM both in vitro and in vivo (Shammas et al, 2008). Although others and we have shown that numerous cytotoxic drugs target telomerase (Uziel et al, 2005; Dong et al, 2009; Mor-Tzuntz et al, 2010), its response to bortezomib has not yet been assessed. In light of common signalling pathways connecting telomerase regulation and bortezomib known mechanisms of action, such as the NFκB axis, we surmised that the drug may affect the activity of telomerase in MM cells. In the current paper, we present data regarding the effect of the drug on telomerase activity in MM cells and analyze the regulatory pathways leading to this inhibitory effect. Although most of the work was performed in vitro using MM cell cultures, we show here that the same mechanisms are also relevant in vivo, by analysing mononuclear cells isolated from bone marrow aspirates of MM patients before and after bortezomib treatment, and ex vivo exposure to the drug. In addition, we found that telomerase response to bortezomib may be correlated with clinical response in patients with MM.
Materials and methods
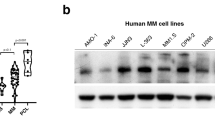
Cell lines
MM cell lines, CAG, ARP-1, U266, and RPMI 8226 were kindly provided by Professor M Lishner (Meir Medical Center, Kfar-Saba, Israel). All cell lines were maintained in RPMI 1640 supplemented with 15% heat-inactivated FCS, glutamine (2 mmol l−1), and penicillin/streptomycin (1%; Biological Industries, Beit Haemek, Israel).
Patients
The clinical part of the study was approved by the local Institutional Review Board (Helsinki Committee). All eight patients signed informed consent forms for participation in the study. Aliquots of bone marrow aspirates were obtained from patients with MM at diagnosis and after 2 weeks of treatment with bortezomib. Fifteen mililitre of anticoagulated aspirates were separated by Ficoll–Hypaque density gradient centrifugation. CD138+ subsets were isolated from the mononuclear cells fraction by using mouse antihuman CD138 antibodies (Miltenyi Biotech, Auburn, CA, USA) coupled to magnetic microbeads (Miltenyi Biotec), followed by magnetic column selection (magnetic-activated cell sorting, Miltenyi Biotec), as previously described (Matsui et al, 2004). Resulting cells were analysed by FACS to ensure proper enrichment with CD 138-positive cells. Cells were maintained in RPMI 1640 supplemented with 15% heat-inactivated FCS, glutamine (2 mmol l−1), and penicillin/streptomycin (1%; Biological Industries).
In preliminary studies, we compared telomerase activity in purified plasma cells vs total mononuclear cells obtained from the bone marrow. Telomerase activity was similar in purified plasma cells and total marrow mononuclear cells, probably due to negligible telomerase activity in the non-neoplastic marrow cells. Therefore, all further studies on ex vivo cells were performed on the mononuclear fraction.
The patients were treated with bortezomib 1.3 mg m−2 on days 1, 4, 8, and 11 every 21 days. In addition, they received 20 mg per week dexamethasone. Assessment of response performed after three cycles of therapy was based on the accepted criteria of International Myeloma Working Group (Kyle and Rajkumar, 2009).
Cell viability – WST-1
CAG or ARP-1 cells (1 × 104 per millilitre) were seeded in quadruplicates in 24-well plates. After addition of bortezomib the cells’ viability was measured by the WST-1 assay, according to the manufacturer’s instructions (Roche, Mannheim, Germany) and as described previously (Uziel et al, 2010).
Telomerase activity – the TRAP assay
Cells (5 × 104 per millilitre) were plated in 24-well plates and incubated with bortezomib as mentioned above. Each treatment was performed in duplicates. Measurement of telomerase activity was performed by the PCR-based TRAP assay, using the TRAPEZE telomerase detection kit (Intergene, Wilmington, DE, USA), according to the manufacturer’s instructions and as previously described (Ram et al, 2009). Briefly, cells were lysed with ice-cold CHAPS lysis buffer for 30 min at 4 °C and were subsequently centrifuged at 13 000 r.p.m. for 30 min at 4 °C. The supernatant was then collected and the protein concentration was determined by the Bradford assay (Bio-Rad Laboratories, Hercules, CA, USA). Each 25 μl reaction mixture contained 10 × TRAP buffer, dNTP mix, TS primer, TRAP primer mix, Taq polymerase, and 0.1 μg protein extract. Reactions were performed at 30 °C for 30 min and were then PCR amplified by 30 cycles of 94 °C, 58 °C, and 72 °C for 30 s, and were separated by electrophoresis on 12.5% polyacrylamide gels (Acryl/Bis 19 : 1 solution). Gels were stained with SYBER Green nucleic acid gel stain (Amresco, Solon, OH, USA). Quantifications were performed using the Quantity-one software for Bio-Rad’s Image analysis systems (Bio-Rad Laboratories, Rishon LeZion, Israel). Telomerase activity was calculated according to the following formula: TPG= [(X−B)/(C−B)]:[(r−B)/Cr × 100], where TPG is the total product generated, X signifies each sample signal, C represents the 36 bp internal PCR control, r is the TSR8 quantification control, and B is the global gel background.
DNA polymerase activity assay
The assay evaluates the ability of DNA polymeraseα to extend a radioactive-labelled oligonucleotide. The labelled primer was annealed to the template DNA as described (Ram et al, 1009) and subjected to DNA polymerisation reaction. Aliquots were removed and separated on PAGE using 16% gels. Quantification was performed by the VersaDoc software on the Gel Doc documentation system (Bio-Rad, Israel).
hTERT expression
Real-time PCR reaction was used to detect the expression of the hTERT gene. Total RNA isolation was done by using the EZ-RNA2 RNA isolation kit (Biological Industries) according to the manufacturer’s instructions. RNA (1 μg) was then reverse transcribed into single-stranded DNA with the cDNA reverse transcription kit (Applied Biosystems, Foster City, CA, USA). Each real-time PCR reaction was carried out with fluorescent gene-specific primers and HPRT primers as an internal control labelled with FAM (Applied Biosystems). The PCR reactions were performed with the readymix PCR master mix Taqman-based kit (Thermo Scientific, Worcester, MA, USA), run, and analysed on the prism 7700 sequence detection system (Applied Biosystems).
The chromatin immunoprecipitation assay
The binding levels of the hTERT transcription factors SP1, c-Myc, and NFκB to its promoter region was assessed by the chromatin immunoprecipitation (ChIP) assay by using the ChIP kit (Millipore, Billerica, MA, USA) according to the manufacturer’s instructions. Basically, cells were lysed and the DNA-binding proteins were cross-linked to the DNA by formaldehyde. Subsequently, the DNA was sheared by sonication. Antibodies against SP1 (Millipore), C-Myc (Millipore), and NFκB (Abcam, Cambridge, MA, USA) were added to the cell lysates and mixed with G-proteins-coated beads. The DNA and its binding protein complexes were immunoprecipitated and the cross-linking between the DNA and its cognate proteins were reversed. The resulted DNA fragments, which should have been enriched with the DNA-binding sites of SP1, c-Myc, and NFκB, were then subjected to a PCR reaction using primers that are homologous to the binding sites of these transcription factor. The primers with the following sequences were used:
For the region of c-Myc and SP-1 binding site:
Forward primer: 5′-AGTGGATTCGCGGGCACAGA-3′;
Reverse primer: 5′-TTCCCACGTGCGCAGCAGGA-3′
For the region of NFκB binding site:
Forward primer: 5′-GCCTCCTAGCTCTGCAGT-3′
Reverse primer: 5′-ACCCGAGGACGCATTGCT-3′
Because of the high GC content in the hTERT promoter region, PCR reactions included several additional temperature steps (in the polymerisation stage) to ensure proper products formation. PCR conditions were as follows:
94 °C, 3 min, followed by 36 cycles at 94 °C, 20 s; 58 °C, 30 s; 72 °C, 20 s; 76 °C, 20 s; 80 °C, 20 s; 84 °C, 20 s; and finally 72 °C, 5 min. The products were separated on a 1.5% agarose PAGE, and analysed by the VersaDoc software on the Gel Doc documentation system (Bio-Rad, Israel).
DNA methylation assay
Isolation of genomic DNA after bortezomib treatments was done with the DNA isolation kit, Puregene (Qiagen, Valencia, CA, USA) according to the manufacturer’s instructions. The purified DNA underwent bisulfite conversion, by which all the unmethylated C nucleotides are converted to T by a specific reagent, using the EZ DNA methylation kit (Zymo Research, Irvine, CA, USA), according to the provided instructions. Briefly, 1 μg DNA was mixed with the CT conversion reagent and was incubated at 50 °C for 12–16 h. The converted DNA was then purified by Zymo-Spin IC columns, and were eluted and subjected to a specific PCR reaction to amplify the GC region in the promoter of hTERT.
PCR reaction conditions were as follows (Nomoto et al, 2002):
Forward primer: 5′-GGGTTTTTAGTGGATT-3′
Reverse primer: 5′-AAACTAAAAAATAAAAAAACAAAAC-3′
PCR programme: 94 °C, 2 min, followed by 40 cycles of 94 °C, 20 s; 48 °C, 30 s; 72 °C, 30 s; and finally 72 °C, 5 min.
The PCR products were then separated on a 1.5% agarose PAGE, gel purified using the Qiagen DNA purification kit, and sequenced (Hylabs, Rechovot, Israel). The DNA sequence of treated vs control samples were compared regarding the number of C to T conversions.
Western blotting
Levels of phosphorylated Akt (pAkt) and PKCα (pPKCα) were measured and compared with the total expression of both proteins. Protein extracts were prepared from the cells after starvation and bortezomib treatment as follows: after growth in RPMI 1640 deprived of serum for 24 h, FCS (15%) was added to induce phosphorylation of Akt and PKCα. Cells were then harvested, washed by PBS, and lysed using CHAPS lysis buffer (TRAPEZE kit). Protein concentration was determined by the Bradford assay (Bio-Rad Laboratories). Identical protein amounts of all samples were subjected to PAGE. The expression of all proteins was detected by specific monoclonal antibody (anti pPKCα and PKCα antibodies were purchased from Santa Cruz Biotechnology, Santa Cruz, CA, USA. Anti pAKT and AKT antibodies were purchased from Cell Signaling, Beverly, MA, USA) in 1 : 1000 dilution followed by fluorescence-labelled secondary antibodies (LI-COR Biosciences, Lincoln, NE, USA). Visualisation and quantification of the proteins levels was performed by using the Odyssey Infrared Imaging System (LI-COR Biosciences).
Immunoprecipitation
The expression of the phosphorylated form of hTERT was measured by immunoprecipitation followed by western blotting. hTERT was immuneprecipitated by anti phosphor-serine antibody (10 μg per 1 mg protein extract) and protein A/G-Sepharose beads (both from Santa Cruz Biotechnology) and was detected by anti hTERT antibody (Epitomics, Burlingame, CA, USA) as described above. Total hTERT was immuneprecipitated by anti hTERT and protein A/G-Sepharose beads (both from Santa Cruz Biotechnology) and was detected by anti hTERT antibody (Epitomics) as described above.
Results
Bortezomib differentially reduced cell viability in MM cell lines
Bortezomib reduced the viability of all MM cell lines in a dose-dependent manner. However, the kinetics and magnitude of this effect differed between the lines. Whereas ARP-1 cells exhibited higher sensitivity to bortezomib, CAG cells were more resistant. As shown in Figure 1A, the IC50 of bortezomib was 2.25 ng ml−1 for the ARP-1 cells and 2.8 ng ml−1 for the CAG cells after 24 h of exposure to the drug. For U266 and RPMI 8226 the IC50 of bortezomib was 3 ng ml−1 and 2.5 ng ml−1, respectively. After 48 h of exposure, this difference diminished and the IC50 value for all cell lines was 1.5–1.7 ng ml−1 (Figure 1A). According to these results, ARP-1 and RPMI 8226 cells are initially more sensitive to bortezomib and after treatment with bortezomib for 48 h all cell lines become equally sensitive.
The effect of bortezomib on MM cells viability and telomerase activity. (A) The effect of bortezomib on cells viability. MM cell lines, ARP-1, CAG, RPMI 8226, and U266 were exposed to bortezomib at the indicated concentrations for 24 and 48 h, and their viability was assessed by the WST-1 assay. 8226, RPMI 8226. The IC50 of each cell line is depicted below the graphs. (B) The effect of bortezomib on telomerase activity. ARP-1, CAG, RPMI 8226, and U266 cells were exposed to the indicated bortezomib concentrations for 24 and 48 h. Telomerase activity was measured by the TRAP assay.
Bortezomib differentially downregulated telomerase activity in all MM cells
Exposure of all four cell lines, ARP-1, CAG, U266, and RPMI 8226, to bortezomib resulted in a marked downregulation of telomerase activity, albeit the kinetics of telomerase downregulation differed among the cell lines. Whereas in ARP-1, U266, and RPMI 8226 cells telomerase activity decreased 24 h after exposure to bortezomib, in CAG cells the effect was observed only after 48 h (Figure 1B). These results correspond to the inhibition of proliferation depicted in the former paragraph. In ARP-1 cells telomerase activity was reduced to 65% of its original activity 24 h after exposure to 1 ng ml−1 bortezomib. At this dose cell viability decreased only by 20% (see Figure 1A). Exposure of the CAG cells to 1 ng ml−1 bortezomib (which did not affect their viability at all) resulted in only a minimal reduction of telomerase activity 24 h after exposure of the cells to bortezomib (Figure 1B). After 48 h of exposure to the drug, a concentration of 1 ng ml−1 did not affect the activity of the enzyme both in ARP-1 and CAG cells. However, the IC50 concentration of the drug resulted in significant repression of the enzymatic activity both in ARP-1 and CAG cells after 48 h (Figure 1B). Telomerase activity in U266 after bortezomib’s exposure in IC50 concentration for 24 and 48 h decreased to 65 and 70% of its original levels, similar to that of ARP-1 cells. Similar results were obtained for RPMI 8226 (60 and 40% reduction after exposure to IC50 concentration of the drug for 24 and 48 h, respectively). The activity of DNA polymeraseα did not decrease after treatment with bortezomib, proving that telomerase inhibition is specific and not due to general inhibition of cellular DNA polymerases (not shown). In addition, bortezomib did not inhibit telomerase directly, as the in vitro addition of an equal bortezomib concentration to cell extract before the TRAP assay did not affect its activity (not shown). Owing to the resemblance of U266 and RPMI 8226 to the ARP-1 cells with regard to telomerase activity after bortezomib treatment, we focused on ARP-1 and CAG cells for the elucidation of the mechanisms of action underlying the effect of bortezomib on telomerase activity.
The above findings imply different regulatory mechanisms for the cell lines. Telomerase is regulated at several levels; epigenetic (methylation status of the CpG island in hTERT promoter), transcriptional, and post-translational. The most important post-translational regulations involve phosphorylation of hTERT by AKT or PKCα (Dong et al, 2005; Wang and Bennett, 2010).
Transcriptional regulation
The methylation status of the hTERT core promoter did not change in response to bortezomib
To evaluate the epigenetic regulation of the hTERT promoter in response to bortezomib in the two cell lines, we assessed the methylation status in response to the drug in both cell lines. As shown in Figure 2A, there was no difference in the level of methylation following bortezomib treatment in the two MM cell lines, ARP-1 and CAG.
The effect of bortezomib on the transcriptional regulation of the hTERT gene. (A) Epigenetic changes of the promoter region of hTERT in response to bortezomib. CAG and ARP-1 cell lines were treated with the IC50 of bortezomib for 24 h and then subjected to bisulfite conversion assay as described in the Materials and Methods. PCR reaction was performed using primers that are homologous to the methylated portion of the hTERT promoter (see Materials and Methods) and was then sequenced. The sequence of the control cells (C) is above that of the treated cells (B). Each methylated residue is shown in bold black and is marked by an asterisk. Unmethylated C’s that were converted to T’s are shown in bold grey, and the rest of the nucleotides are marked in black. The rectangular frame depicts the single difference detected between the control and the bortezomib treated cells. The results were similar for both ARP-1 and CAG cells. (B) hTERT gene expression in MM cells after exposure to bortezomib. Both ARP-1 and CAG MM cells were treated with bortezomib (1 ng ml−1 and IC50 determined for 24 h) for 14 or 24 h and the gene expression of hTERT was assessed by real-time PCR as described in the Materials and Methods. The bars represent the ratio of the expression of hTERT to that of the control gene, HPRT. (C) The binding of SP1, c-Myc and NFκB to the hTERT promoter. ARP-1 and CAG cells were treated with IC50 concentrations of bortezomib for 24 h and the binding of the three transcription factors SP1, c-Myc, and NFκB to the hTERT promoter was measured by the ChIP assay. On the left panel a representative result of the PCR products at each transcription factor binding site separated on a PAGE is shown. B, bortezomib-exposed cells; C, control cells; TI, total input DNA. On the right, a summary of three independent experiments is shown. In each case, the level of the specific signal was calculated relatively to the total input DNA, which was not immunoprecipitated with the specific antibody (see Materials and Methods for more details). (D) The levels of SP-1 after exposure of MM cells to bortezomib. ARP-1 and CAG MM cells were treated with two doses of bortezomib for 24 h, and the levels of total cellular SP-1 were determined by western blotting relatively to that of a control protein, GAPDH. B3, cells treated with 3 ng ml−1 of bortezomib; B5, cells treated with 5 ng ml−1 of bortezomib. A representative blot is shown on the upper panel, and a summary of three independent experiments is shown on the bottom panel comparing SP1 levels in treated vs untreated cells.
Bortezomib decreased the hTERT expression
In both lines bortezomib transcriptionally downregulated telomerase activity by inhibiting hTERT expression. This inhibition was quite similar in the two cell lines. Both of them showed a reduction of about 50% in hTERT expression upon exposure to the IC50 of the drug, whereas their exposure to a lower bortezomib concentration did not affect hTERT gene expression (Figure 2B).
Bortezomib reduced Sp1 binding to hTERT promoter but not of NFkB and c-Myc
To identify the transcription factor that may be involved in downregulation of promoter activity, we assessed the binding of its three major transcription factors: SP-1, c-Myc, and NFκB. The ChIP analysis showed that decrease in binding of SP-1 transcription factor is responsible for the transcriptional downregulation of telomerase. SP1 binding to the hTERT promoter was reduced (50%) after bortezomib treatment. This effect was similar in both cell lines. The binding of c-Myc and NFκB to the hTERT promoter was not affected by treatment with bortezomib (Figure 2C).The decrease in SP-1 binding was concomitant with the total cellular decrease in SP-1 levels in the cells following the administration of bortezomib (Figure 2D). For the detection of cellular SP-1 levels, we exposed the cells to higher bortezomib concentrations to see the drug’s maximal effect.
Post-translational modifications
Bortezomib inhibited the phosphorylation of hTERT only in ARP-1 cells
The identical degree of transcriptional inhibition of hTERT does not explain the differential kinetics of telomerase activity inhibition in the two cell lines. Therefore, an additional regulatory level should account for this difference. Consequently, the phosphorylation of telomerase was measured by immunoprecipitation. The phosphorylation status of hTERT in the ARP-1 cells markedly decreased (65% reduction compared with the untreated cells), whereas it did not changed in the CAG cells. This was the case even at very high bortezomib concentrations (Figure 3A). The differential downregulation of hTERT phosphorylation can explain the different response of telomerase activity to bortezomib of these two cell lines, as post-translational modification results in an immediate effect on telomerase activity, whereas the transcriptional effect is only manifest after half-life of the enzyme.
The effect of bortezomib on the post-translational regulation of telomerase. (A) The effect of bortezomib on the phosphorylation of telomerase. ARP-1 and CAG cells were treated with the IC50 of bortezomib for 24 h, and the levels of phospho-telomerase were determined by immunoprecipitation followed by western blotting as described in the Materials and Methods. Phosphorylated telomerase was precipitated with an anti phosphor-serine antibody and was blotted with an anti-telomerase antibody, and total telomerase was precipitated and blotted with anti-telomerase antibody. C, control cells; B, cells treated with bortezomib; p-hTERT, phosohprylated form of telomerase; t-hTERT, total levels of telomerase. A representative result is shown on the upper part. The experiment was repeated twice with similar results as shown in the bottom part. (B) The effect of bortezomib on the phosphorylation of AKT. ARP-1 and CAG cells were serum starved for 24 h with or without the IC50 dose of bortezomib and then stimulated with serum for 2 h. The levels of the phosphorylated form of AKT were determined by western blotting. B, cells treated with bortezomib; C, control cells; p-AKT, phosphorylated AKT; t-AKT, total levels of AKT. A representative blot is shown. The levels of AKT phosphorylation was calculated relatively to the total amounts of the protein and are shown on the bottom part of the figure. (C) The effect of bortezomib on the phosphorylation of PKCα. ARP-1 and CAG cells were serum starved for 24 h with or without the IC50 dose of bortezomib and then stimulated with serum for 2 h. The levels the phosphorylated form of PKCα were determined by western blotting. p, PKCα- phosphorylated PKCα; t- PKCα, total levels of PKCα. A representative blot is shown. The levels of PKCα phosphorylation was calculated relatively to the total amounts of the protein and is shown on the bottom panel.
AKT phosphorylation did not account for the decrease in telomerase activity
AKT is considered a major kinase that phosphorylates hTERT. As shown in Figure 3B, bortezomib caused a very small decrease in AKT phosphorylation in the two cell lines. Therefore, AKT does not have a significant role in the post-translational regulation of telomerase by bortezomib.
Bortezomib differentially decreased PKCα phosphorylation in MM cells
The kinase PKCα has been previously shown to act as an additional post-translational modulator of hTERT by phosphorylation of the enzyme. The phosphorylated form of PKCα in ARP-1 cells was downregulated in response to bortezomib (40% reduction compared with the control untreated cells), whereas there was no effect of the drug on PKCα phosphorylation status in CAG cells (Figure 3C). These findings suggest that the different kinetics of telomerase downregulation by bortezomib are caused by differential effect on PKCα phosphorylation.
The degree and mode of regulation of telomerase inhibition by bortezomib in myeloma patients correlated with the in vitro results and with the clinical response
Bone marrow aspirates were obtained from eight patients with myeloma. Four of these patients responded very well to treatment with bortezomib whereas the others were resistant to treatment with this drug. We defined the patients as ‘good’ and ‘poor’ responders according to the above-mentioned criteria.
Ex vivo exposure of eight MM patients’ cells to bortezomib resulted in a differential response of cell viability and telomerase activity termed ‘good responders’ and ‘poor responders’.
As shown in Figure 4A, cell viability markedly decreased in the responsive patients, whereas in ‘poor’ responders viability was reduced only at high concentrations of bortezomib and did not reach 50% inhibition even at those doses. Similar results were obtained regarding telomerase activity (Figure 4). The cells of ‘sensitive’ patients exhibited about 70% reduction in telomerase activity after exposure to bortezomib, while in the cells of resistant patients a negligible response was noted. Importantly, the initial telomerase activity of these samples was different, as the responsive patients exhibited lower telomerase activity vs the refractory ones (80% on average compared with the refractory patients).
The effect of bortezomib on cells isolated from MM patients: viability, telomerase activity, and the expression of the phosphorylated form of PKCα. (A) The ex vivo effect of bortezomib on the viability of cells isolated from MM patients. Mononuclear cells were isolated from bone marrow aspirates of eight MM patients at diagnosis and were exposed ex vivo to the drug (1–3 ng ml−1) for 24 h. Their viability was assessed by the WST-1 assay. Viability of cells with no bortezomib was defined as 100%. Good, good responders (see text for definition). Bad, poor responders (see text for definition). (B) The ex vivo and in vivo effect of bortezomib on telomerase activity of cells isolated from MM patients. Mononuclear cells were isolated from bone marrow aspirates of eight MM patients, and were exposed ex vivo for 24 h (left) or in vivo after two consecutive cycles of bortezomib (right). Telomerase activity was measured by the TRAP assay. The gel in the middle represents telomerase activity of cells exposed ex vivo to bortezomib isolated from a MM patient refractory to the drug. N, negative control containing no protein extracts; R8, standard TRAP assay control. The graph below depicts the quantitation of telomerase activity in response to the drug in all 8 patients. All telomerase activities are shown in percentages, while the initial telomerase activity of refractory patients is considered 100%. (C) The ex vivo effect of bortezomib on the phosphorylated form of PKCα in cells isolated from MM patients. Mononuclear cells were isolated from bone marrow aspirates of two MM patients: sensitive (left) and resistant (right) to bortezomib. The isolated cells were exposed ex vivo to bortezomib (5–7 ng ml−1) for 24 h. The levels the phosphorylated form of PKCα were determined by Western blotting. The quantitation of the effect describing the % decrease of PKCα expression relatively to that of the control gene, GAPDH is shown on the bottom. Abbreviations: B5 and B7, cells treated with 5 and 7 ng ml−1 of bortezomib; Brt, bortezomib; C, control cells; M, molecular size protein marker.
In two patients belonging to the ‘good’ responders group, we were also able to measure the in vivo telomerase activity in marrow cells after three cycles of bortezomib treatment. These in vivo results demonstrated a marked reduction in telomerase activity verifying the ex vivo data (Figure 4B).
As the difference between the more sensitive (ARP-1) and less sensitive (CAG) cells stemmed from the degree of PKCα dephosphorylation, we assessed this aspect in the ex vivo cells.
The results of the PKCα analyses after ex vivo exposure of cells isolated from MM patients to bortezomib showed that in ‘good’ clinical responders PKCα phosphorylation was markedly downregulated, whereas in resistant patients PKCα phosphorylation remained almost unchanged (Figure 4C) validating the significance of these findings.
Discussion
Our results shed light on the effects, mechanism, and potential clinical implications of bortezomib on telomerase activity in MM. Together with its expected effect on the viability of the cells, bortezomib inhibited the activity of telomerase, albeit with different kinetics in the two different cell lines. This inhibition was specific to telomerase and not to other DNA polymerases, as DNA polymeraseα was not affected by the highest drug concentration and is not caused by direct chemical interaction. Bortezomib inhibited telomerase independently of cell death, as the effect on hTERT expression was detected 14 h after the exposure to the drug, even in concentrations that do not harm cell viability (Figure 2B). In addition DNA polymeraseα activity was not affected by bortezomib attesting to the fact that telomerase inhibition is a specific effect.
The differential sensitivity to bortezomib was more pronounced between ARP-1 cells (more sensitive) and CAG cells. This difference probably stems from variations between these two lines. Several studies have shown various differences between these two cell lines. For example, they significantly differ in the expression of CD74 (Yaccoby et al, 2004) and sensitivity to fenretinide (Li et al, 2009). None of these features, however, is directly related to bortezomib resistance as far as we know. In addition, ARP-1 cells are non-adherent whereas CAG adhere to the growth surface. Adherence to the stroma is known as a feature related to cancer cell aggressiveness and resistance to several chemotherapeutic drugs (Rafii et al, 2008).
The diverse kinetics of telomerase inhibition between the two cell lines, ARP-1 and CAG, imply different regulatory mechanisms in each cell type. Telomerase is regulated at several levels from epigenetic to post-translational; among those, the transcriptional level is considered to be the most important one (Cairney and Keith, 2008).
The methylation pattern of the hTERT promoter region differs from the common epigenetic repression of a gene promoter (Nomoto et al, 2002). Recent reports suggest that there is a core region in the hTERT promoter in which methylation represses hTERT expression (Chen et al, 2010; Choi et al, 2010). The results of our study show that in both cell lines the methylation status of this core region in the hTERT promoter region did not change after exposure to bortezomib showing that the effect of the drug on the activity of telomerase is probably not mediated by epigenetic methylation of the hTERT promoter. A similar independence of hTERT expression on the methylation status of its promoter was shown in pre-malignant cervical lesions (Oikonomou et al, 2007).
In both cell lines, the expression of the hTERT gene was markedly downregulated as a result of bortezomib treatment. SP-1 and c-Myc are considered the most important transcription factors of hTERT (Dong et al, 2005), while NFκB is a well-established target of proteasome inhibitors and has been also shown to activate the hTERT promoter (Wang and Bennett, 2010). The results of the ChIP assay showed that in both cell lines the binding of c-Myc and NFκB were not affected by the drug, but SP1 binding was markedly decreased by exposure to bortezomib. This reduction of SP1 binding might be caused by either the inhibition of its binding to the promoter, or by the general decrease in cellular SP1 levels. In our system and in another report (Liu et al, 2008) bortezomib treatment resulted in a significant decrease in total cellular SP1.
Many reports show that NFκB levels are decreased by bortezomib (Hideshima et al, 2002). Therefore, it is somewhat surprising that the binding of NFκB did not decrease in our system. This can be explained by the fact that the effect of bortezomib on NFκB function is complex. Recent reports claim that in MM cells bortezomib induces canonical NFκB activation via the downregulation of the IκBα (Hideshima et al, 2009).
The transcriptional inhibition could not account for the differential response of telomerase to the drug in these two lines because it was similar in both. We therefore analysed the phosphorylation status of the enzyme after exposure to bortezomib. The phosphorylation of telomerase markedly decreased in response to bortezomib in the ARP-1 cell line, but not in the CAG cell. This difference may explain the differential kinetics of telomerase downregulation.
Two main kinases are known to phosphorylate telomerase: AKT and PKCα (Dong et al, 2005, Wang and Bennett, 2010). The very mild change in the phosphorylation levels of AKT in response to bortezomib suggests that this pathway is not involved in the effect of the drug on telomerase activity, at least in the two examined cell lines. These results are consistent with other reports, showing that AKT is not a target of bortezomib in MM cells (Hideshima et al, 2006). However, other studies reported an inhibitory effect of bortezomib on the activation of AKT in hepatocellular carcinoma cells (Chen et al, 2008), or a combination of bortezomib and a farnesyl transferase inhibitor, which caused apoptosis via downregulation of pAKT in MM cells (David et al, 2005). These differing results may reflect the heterogeneity of AKT pathways in MM cells. For example, a differential dependency of MM cells on pAKT, which correlated with the sensitivity of the cells to the drug has been reported (Zöllinger et al, 2008). We did not find such a correlation in our experimental system but rather with the phosphorylation of PKCα in response to bortezomib. PKCα phosphorylation differed in the two cell lines, whereas in the ARP-1 cells bortezomib downregulated the phosphorylation of PKCα, there was no such effect on phosphorylation in the CAG cells. We concluded that the differential effect of bortezomib on hTERT phosphorylation was mediated by PKCα.
In this study, we demonstrated that telomerase inhibition by bortezomib also occurred in the clinical setting. Telomerase activity was downregulated in myeloma cells exposed to bortezomib either in vivo or ex vivo. Interestingly, the degree and mode of regulation of telomerase inhibition by bortezomib might correlate with the clinical response. Cells extracted from the bone marrow of patients responding well to bortezomib also showed a reduction in telomerase activity after ex vivo exposure to the drug. In contrast, in cells taken from bortezomib-resistant patients telomerase activity was not affected by ex vivo exposure to the drug. It seems that the regulatory pathways and their variations in these cells are similar to those of the in vitro system. Whereas in cells from the ‘good responders’ phosphorylation of the PKCα was markedly downregulated after the ex vivo exposure to the drug, there was no effect on that enzyme in cells extracted from the bone marrow compartment of the bortezomib-resistant patients. The patients differed also in their initial telomerase activity, which was lower in the responsive and higher in the refractory samples. Similar diversities in the degree of telomerase activity among MM patients have been reported (Xu et al, 2001; Wu et al, 2003; Panero et al, 2010).
This study establishes telomerase as an additional target of bortezomib in MM. The differential mechanism of inhibition in various cell lines and cells obtained from different patients may indicate that similar differences between patients with MM may also be translated into the clinical setting. Telomerase inhibition by bortezomib may vary in subsets of MM patients in relation to their pPKCα dependency and serve a potential clinical use. As such, the ex vivo assessment of telomerase activity response to bortezomib treatment may serve as a prognostic feature and add to the therapeutic armamentarium by the addition of telomerase inhibitors in defined subsets of patients.
Future studies will have to be undertaken to validate the clinical data reported here and explore the possibility of incorporating treatment with telomerase inhibitors in patients whose telomerase is resistant to the effect of bortezomib.
Change history
09 November 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Akiyama M, Hideshima T, Hayashi T, Tai YT, Mitsiades CS, Mitsiades N, Chauhan D, Richardson P, Munshi NC, Anderson KC (2002) Cytokines modulate telomerase activity in a human multiple myeloma cell line. Cancer Res 62 (13): 3876–3882
Akiyama M, Hideshima T, Shammas MA, Hayashi T, Hamasaki M, Tai YT, Richardson P, Gryaznov S, Munshi NC, Anderson KC (2003) Effects of oligonucleotide N3'-->P5' thio-phosphoramidate (GRN163) targeting telomerase RNA in human multiple myeloma cells. Cancer Res 63 (19): 6187–6194
Anderson KC (2004) Bortezomib therapy for myeloma. Curr Hematol Rep 3 (1): 65
Blackburn EH, Collins K (2010) Telomerase: an RNP enzyme synthesizes DNA. Cold Spring Harb Perspect Biol 3 (5): pii: a003558
Cairney CJ, Keith WN (2008) Telomerase redefined: integrated regulation of hTR and hTERT for telomere maintenance and telomerase activity. Biochimie 90 (1): 13–23
Chen KF, Yeh PY, Yeh KH, Lu YS, Huang SY, Cheng AL (2008) Down-regulation of phospho-Akt is a major molecular determinant of bortezomib-induced apoptosis in hepatocellular carcinoma cells. Cancer Res 68 (16): 6698–6707
Chen W, Dong Q, Shin KH, Kim RH, Oh JE, Park NH, Kang MK (2010) Grainyhead-like 2 enhances the hTERT gene expression by inhibiting DNA methylation at the 5'-CpG island in normal human keratinocytes. J Biol Chem 285 (52): 40852–40863
Choi JH, Min NY, Park J, Kim JH, Park SH, Ko YJ, Kang Y, Moon YJ, Rhee S, Ham SW, Park AJ, Lee KH (2010) TSA-induced DNMT1 down-regulation represses hTERT expression via recruiting CTCF into demethylated core promoter region of hTERT in HCT116. Biochem Biophys Res Commun 391 (1): 449–454
David E, Sun SY, Waller EK, Chen J, Khuri FR, Lonial S (2005) The combination of the farnesyl transferase inhibitor lonafarnib and the proteasome inhibitor bortezomib induces synergistic apoptosis in human myeloma cells that is associated with down-regulation of p-AKT. Blood 106 (13): 4322–4329
Dong CK, Masutomi K, Hahn WC (2005) Telomerase: regulation, function and transformation. Crit Rev Oncol Hematol 54 (2): 85–93
Dong X, Liu A, Zer C, Feng J, Zhen Z, Yang M, Zhong L (2009) siRNA inhibition of telomerase enhances the anti-cancer effect of doxorubicin in breast cancer cells. BMC Cancer 9: 133–143
Gahrton G (2004) New therapeutic targets in multiple myeloma. Lancet 364 (9446): 1648–1649
Hideshima T, Catley L, Yasui H, Ishitsuka K, Raje N, Mitsiades C, Podar K, Munshi NC, Chauhan D, Richardson PG, Anderson KC (2006) Perifosine, an oral bioactive novel alkylphospholipid, inhibits Akt and induces in vitro and in vivo cytotoxicity in human multiple myeloma cells. Blood 107: 4053–4062
Hideshima T, Chauhan D, Richardson P, Mitsiades C, Mitsiades N, Hayashi T, Munshi N, Dang L, Castro A, Palombella V, Adams J, Anderson KC (2002) NF-kappa B as a therapeutic target in multiple myeloma. J Biol Chem 277 (19): 16639–16647
Hideshima T, Ikeda H, Chauhan D, Okawa Y, Raje N, Podar K, Mitsiades C, Munshi NC, Richardson PG, Carrasco RD, Anderson KC (2009) Bortezomib induces canonical nuclear factor-kappaB activation in multiple myeloma cells. Blood 114 (5): 1046–1052
Jackson G, Einsele H, Moreau P, Miguel JS (2005) Bortezomib, a novel proteasome inhibitor, in the treatment of hematologic malignancies. Cancer Treat Rev 31 (8): 591–602
Kyle RA, Rajkumar SV (2009) Criteria for diagnosis, staging, risk stratification and response assessment of multiple myeloma. Leukemia 23 (1): 3–9
Lenz HJ (2003) Clinical update: proteasome inhibitors in solid tumors. Cancer Treat Rev 29 (suppl 1): 41–48
Li X, Ling W, Pennisi A, Khan S, Yaccoby S (2009) Fenretinide inhibits myeloma cell growth, osteoclastogenesis and osteoclast viability. Cancer Lett 284 (2): 175–181
Liu S, Liu Z, Xie Z, Pang J, Yu J, Lehmann E, Huynh L, Vukosavljevic T, Takeki M, Klisovic RB, Baiocchi RA, Blum W, Porcu P, Garzon R, Byrd JC, Perrotti D, Caligiuri MA, Chan KK, Wu LC, Marcucci G (2008) Bortezomib induces DNA hypomethylation and silenced gene transcription by interfering with Sp1/NF-kappaB-dependent DNA methyltransferase activity in acute myeloid leukemia. Blood 111 (4): 2364–2373
Matsui W, Huff CA, Wang Q, Malehorn MT, Barber J, Tanhehco Y, Smith BD, Civin CI, Jones RJ (2004) Characterization of clonogenic multiple myeloma cells. Blood 103 (6): 2332–2336
Mor-Tzuntz R, Uziel O, Shpilberg O, Lahav J, Raanani P, Bakhanashvili M, Rabizadeh E, Zimra Y, Lahav M, Granot G (2010) Effect of imatinib on the signal transduction cascade regulating telomerase activity in K562 (BCR-ABL-positive) cells sensitive and resistant to imatinib. Exp Hematol 38 (1): 27–37
Nomoto K, Maekawa M, Sugano K, Ushiama M, Fukayama N, Fujita S, Kakizoe T (2002) Methylation status and expression of human telomerase reverse transcriptase mRNA in relation to hypermethylation of the p16 gene in colorectal cancers as analyzed by bisulfite PCR-SSCP. Jpn J Clin Onco 32 (1): 3–8
Oikonomou P, Messinis I, Tsezou A (2007) DNA methylation is not likely to be responsible for hTERT expression in premalignant cervical lesions. Exp Biol Med (Maywood) 232 (7): 881–886
Panero J, Arbelbide J, Fantl DB, Rivello HG, Kohan D, Slavutsky I (2010) Altered mRNA expression of telomere-associated genes in monoclonal gammopathy of undetermined significance and multiple myeloma. Mol Med 16 (11-12): 471–478
Ram R, Uziel O, Eldan O, Fenig E, Beery E, Lichtenberg S, Nordenberg Y, Lahav M (2009) Ionizing radiation up-regulates telomerase activity in cancer cell lines by post-translational mechanism via ras/phosphatidylinositol 3-kinase/Akt pathway. Clin Cancer Res 15 (3): 914–923
Rafii A, Mirshahi P, Poupot M, Faussat A-M, Simon A, Ducros E, Mery E, Couderc B, Lis R, Capdet J, Bergalet J, Querleu D, Dagonnet F, Fournié J-J, Marie J-P, Pujade-Lauraine E, Favre G, Soria J, Mirshahi M (2008) Oncologic trogocytosis of an original stromal cells induces hemoresistance of ovarian tumours. PLoS ONE 3 (12): e3894
Shammas MA, Koley H, Bertheau RC, Neri P, Fulciniti M, Tassone P, Blotta S, Protopopov A, Mitsiades C, Batchu RB, Anderson KC, Chin A, Gryaznov S, Munshi NC (2008) Telomerase inhibitor GRN163L inhibits myeloma cell growth in vitro and in vivo. Leukemia 22 (7): 1410–1418
Shay JW, Wright WE (2005) Mechanism-based combination telomerase inhibition therapy. Cancer Cell 7 (1): 1–2
Shiratsuchi M, Muta K, Abe Y, Motomura S, Taguchi F, Takatsuki H, Uike N, Umemura T, Nawata H, Nishimura J (2002) Clinical significance of telomerase activity in multiple myeloma. Cancer 94 (8): 2232–2238
Uziel O, Beery E, Dronichev V, Samocha K, Gryaznov S, Weiss L, Slavin S, Kushnir M, Nordenberg Y, Rabinowitz C, Rinkevich B, Zehavi T, Lahav M (2010) Telomere shortening sensitizes cancer cells to selected cytotoxic agents: in vitro and in vivo studies and putative mechanisms. PLoS One 5 (2): e9132
Uziel O, Fenig E, Nordenberg J, Beery E, Reshef H, Sandbank J, Birenbaum M, Bakhanashvili M, Yerushalmi R, Luria D, Lahav M (2005) Imatinib mesylate (Gleevec) downregulates telomerase activity and inhibits proliferation in telomerase-expressing cell lines. Br J Cancer 92 (10): 1881–1891
Wang JC, Bennett MR (2010) Nuclear factor-{kappa}B-mediated regulation of telomerase: the Myc link. Arterioscler Thromb Vasc Biol 30 (12): 2327–2328
Wu KD, Orme LM, Shaughnessy J, Jacobson J, Barlogie B, Moore MA (2003) Telomerase and telomere length in multiple myeloma: correlations with disease heterogeneity, cytogenetic status, and overall survival. Blood 101 (12): 4982–4989
Xu D, Zheng C, Bergenbrant S, Holm G, Björkholm M, Yi Q, Gruber A (2001) Telomerase activity in plasma cell dyscrasias. Br J Cancer 84 (5): 621–625
Yaccoby S, Wezeman MJ, Henderson A, Cottler-Fox M, Yi Q, Barlogie B, Epstein J (2004) Cancer and the microenvironment: myeloma-osteoclast interactions as a model. Cancer Res 64 (6): 2016–2023
Zöllinger A, Stühmer T, Chatterjee M, Gattenlöhner S, Haralambieva E, Müller-Hermelink HK, Andrulis M, Greiner A, Wesemeier C, Rath JC, Einsele H, Bargou RC (2008) Combined functional and molecular analysis of tumor cell signaling defines two distinct myeloma subgroups: Akt-dependent and Akt-independent multiple myeloma. Blood 112 (8): 3403–3411
Author information
Authors and Affiliations
Corresponding author
Additional information
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Weiss, C., Uziel, O., Wolach, O. et al. Differential downregulation of telomerase activity by bortezomib in multiple myeloma cells-multiple regulatory pathways in vitro and ex vivo. Br J Cancer 107, 1844–1852 (2012). https://doi.org/10.1038/bjc.2012.460
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2012.460