Abstract
OBJECTIVE: Several investigators have focused on obesity as a specific risk factor for mortality in patients undergoing bypass surgery, but few have examined it as a risk factor among patients undergoing percutaneous coronary interventions (PCI). In addition, none have evaluated the impact of obesity on post-PCI quality of life or disease-specific health status. This study examined whether obesity is a risk factor for poor quality of life or diminished health status 12-months postprocedure among a large cohort of PCI patients.
RESEARCH METHODS AND PROCEDURES: A total of 1631 consecutive PCI patients were enrolled into the study and classified as underweight (BMI <20 kg/m2), normal weight range (BMI ≥20 and <25 kg/m2), overweight (BMI ≥25 and <30 kg/m2), class I obese (BMI ≥30 kg/m2), or class II and III obese (BMI ≥35 kg/m2). The 12-month postprocedure outcomes included need for repeat procedure, survival, quality of life and health status, assessed using the Seattle Angina Questionnaire (SAQ) and the Short Form-12.
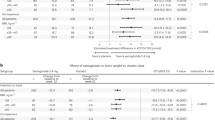
RESULTS: Obese patients with and without a history of revascularization were significantly younger than overweight, normal weight range, or underweight patients at the time of PCI. However, obese patients demonstrated similar long-term recovery and improved disease-specific health status and quality of life when compared to patients in the normal weight range after PCI. In addition, mortality and risk for repeat procedure was similar to those patients in the normal weight range patients at 12-months postrevascularization. Underweight patients who had no previous history of revascularization reported lower quality of life (F=3.02; P=0.018) and poorer physical functioning (F=2.82; P=0.024) than other BMI groups.
CONCLUSION: Obese patients presenting for revascularization were younger when compared to patients in the normal weight range, regardless of previous history of revascularization. However, weight status was not a significant predictor of differences in long-term disease-specific health status, quality of life, repeat procedures, or survival. Underweight patients demonstrated less improvement in quality of life and physical functioning than other BMI groups.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Flegal KM, Carroll MD, Ogden CL, Johnson CL . Prevalence and trends in obesity among US adults, 1999–2000. JAMA 2002; 288: 1723–1727.
Colditz GA . Economic costs of obesity and inactivity. Med Sci Sports Exerc 1999; 31: S663–S667.
Allison DB, Fontaine KR, Manson JE, Stevens J, VanItallie TB . Annual deaths attributable to obesity in the United States. JAMA 1999; 282: 1530–1538.
Eckel RH, Krauss RM . American Heart Association call to action: obesity as a major risk factor for coronary heart disease. Circulation 1998; 97: 2099–2100.
Suwaidi JA, Wright RS, Grill JP, Hensrud DD, Murphy JG, Squires RW, Kopecky SL . Obesity is associated with premature occurrence of acute myocardial infarction. Clin Cardiol 2001; 24: 542–547.
Birkmeyer NJO, Charlesworth DC, Hernandez F et al. Obesity and risk of adverse outcomes associated with coronary artery bypass surgery. Circulation 1998; 97: 1689–1694.
Schindler RFM, Schumacher B, Schlaudraff K, Hannes W, Seitelberger R, Schlosser V . The influence of obesity on perioperative morbidity: retrospective study of 502 aortocoronary bypass operations. Thorac Cardiovasc Surg 1991; 40: 126–129.
Kurki TSO, Kataja M . Preoperative prediction of postoperative morbidity in coronary artery bypass grafting. Ann Thorac Surg 1996; 61: 1740–1745.
Prasad, US, Walker WS, Sang CTM, Campanella C, Cameron EWJ . Influence of obesity on the early and long term results of surgery for coronary artery disease. Eur J Cardiothorac Surg 1991; 5: 67–73.
Sabourin CB, Fun M . Readmission of patients after coronary artery bypass graft surgery. Heart Lung 1999; 28: 243–250.
Christakis GT, Weisel RD, Buth KJ, Fremes SE, Rao V, Panagiotopoulos K, Ivanov J, Goldman BS, David TE . Is body size the cause for poor outcomes of coronary artery bypass operations in women? J Thorac Cardiovasc Surg 1995; 110: 344–1358.
Milano CA, Kesler K, Archibald N, Sexton DJ, Jones RH . Mediastinitis after coronary artery bypass graft surgery. Risk factors and long-term survival. Circulation 1995; 92: 2245–2251.
Zacharias A, Habib RH . Factors predisposing to median sternotomy complications: deep vs superficial infection. Chest 1996; 110: 1173–1178.
Lahey SJ, Borlase BC, Lavin PT, Levitsky S . Preoperative risk factors that predict hospital length of stay in coronary artery bypass patients >60 years old. Circulation 1992; 86 (Suppl II): II-181–II185.
Eisenstein EL, Shaw LK, Nelson CL, Anstrom KJ, Hakim Z, Mark DB . Obesity and long-term clinical and economic outcomes in coronary artery disease patients. Obes Res 2002; 10: 83–91.
Edwards FH, Clark RE, Schwartz M . Coronary artery bypass grafting: The Society of Thoracic Surgeons National Database experience. Ann Thorac Surg 1994; 57: 12–19.
Hannan EL, Kilburn H, O'Donnell J, Lukacik G, Shields EP . Adult open heart surgery in New York State. An analysis of risk factors and hospital mortality rates. JAMA 1990; 264: 2768–2774.
Reeves BC, Ascione R, Chamberlin MH, Angelini GD . Effect of body mass index on early outcomes in patients undergoing coronary artery bypass surgery. J Am Coll Cardiol 2003; 42: 668–676.
American Heart Association (AHA). Heart disease and stroke statistics – 2003 update. American Heart Association: Dallas, TX; 2002.
Ellis SG, Elliot J, Horrigan M, Raymond RE, Howell G . Low-normal or excessive body mass index: newly identified and powerful risk factors for death and other complications with percutaneous coronary intervention. Am J Cardiol 1996; 78: 642–646.
Gruberg L, Weissman NJ, Waksman R, Fuchs S, Deible R, Pinnow EE, Ahmed LM, Kent KM, Pichard AD, Suddath WO, Satler LF, Lindsay J . The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: the obesity paradox? J Am Coll Cardiol 2002; 39: 578–584.
Powell BD, Lennon RJ, Lerman A, Bell MR, Berger PB, Higano ST, Holmes DR, Rihal CS . Association of body mass index with outcome after percutaneous coronary intervention. Am J Cardiol 2003; 91: 472–476.
Gurm HS, Whitlow PL, Kip KE . The impact of body mass index on short- and long-term outcomes in patients undergoing coronary revascularization. Insights from the Bypass Angioplasty Revascularization Investigation (BARI). J Am Coll Cardiol 2002; 39: 834–840.
Gurm HS, Brennan DM, Booth J, Tcheng JE, Lincoff M, Topol EJ . Impact of body mass index on outcome after percutaneous coronary intervention (the obesity paradox). Am J Cardiol 2002; 90: 42–45.
Zhang Z, Mahoney EM, Stables RH, Booth J, Nugara F, Spertus JA, Weintraub WS . Disease-specific health status after stent-assisted percutaneous coronary intervention and coronary artery bypass surgery. One-year results from the stent or surgical trial. Circulation 2003; 108: 1694–1700.
World Health Organization (WHO). Obesity: preventing and managing the global epidemic. Report of a WHO consultation on obesity. World Health Organization: Geneva, Switzerland; 1998.
National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI). Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity: the evidence report. U.S. Government Press: Washington, DC; 1998.
Bourassa MG, Detre KM, Johnston JM, Vlachos HA, Holubkov R . Effect of prior revascularization on outcome following percutaneous coronary intervention; NHLBI Dynamic Registry. Eur Heart J 2002; 23: 1546–1555.
Spertus JA, Bliven BD, Farner M, Gillen A, Hewitt T, Jones P, McCallister BD . Integrating baseline health status data collection into the process of care: A case study and descriptive summary. Jt Comm J Qual Improv 2001; 27 (7): 369–380.
Deyo RA, Diehr P, Patrick DL . Reproducibility and responsiveness of health status measures: statistics and strategies for evaluation. Control Clin Trials 1991; 12: 14S–58S.
Dougherty CM, Dewhurst T, Nichol WP, Spertus J . Comparison of three quality of life instruments in stable angina pectoris: Seattle Angina Questionnaire, Short Form Health Survey (SF-36), and Quality of Life Index-Cardiac Version III. J Clin Epidemiol 1998; 51: 569–575.
Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Fihn SD . Monitoring the quality of life in patients with coronary artery disease. Am J Cardiol 1994; 74: 1240–1244.
Spertus JA, Winder JA, Dewhurst TA, Deyo RA, Prodzinski J, McDonell M, Fihn SD . Development and evaluation of the Seattle Angina Questionnaire: a new functional status measure for coronary artery disease. J Am Coll Cardiol 1995; 25: 333–341.
Spertus JA, Jones P, McDonell M, Fan V, Fihn SD . Health status predicts long-term outcomes in outpatients with coronary disease. Circulation 2002; 106: 43–49.
McHorney CA, Ware JE, Raczek AE . The MOS-36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Med Care 1993; 31: 247–263.
Ware J, Kosinski M, Keller SD . A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–233.
Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, Bullinger M, Kaasa S, Leplege A, Prieto L, Sullivan M . Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 1998; 51: 1171–1178.
Delate T, Coons SJ . The discriminative ability of the 12-item short form health survey (SF-12) in a sample of persons with HIV. Clin Ther 2000; 22: 1112–1120.
Lim LL, Fisher JD . Use of the 12-item short-form (SF-12) Health Survey in an Australian heart and stroke population. Qual Life Res 1999; 8: 1–8.
Ni H, Tow W, Burgess D, Wise K, Nauman DJ, Crispell K, Hershberger RE . Comparative responsiveness of the Short-Form 12 and Minnesota Living with Heart Failure Questionnaire in patients with heart failure. J Card Fail 2000; 6: 83–91.
Pickard AS, Johnson JA, Penn A, Lau F, Noseworthy T . Replicability of SF-36 summary scores by the SF-12 in stroke patients. Stroke 1999; 30: 1213–1217.
Block PC, Peterson ED, Krone R, Kesler K, Hannan E, O'Connor GT, Detre K, Peterson EC . Identification of variables needed to risk adjust outcomes of coronary interventions: evidence-based guidelines for efficient data collection. J Am Coll Cardiol 1998; 32: 275–282.
Psaty BM, Furberg CD, Kuller LH, Bild DE, Rautaharju PM, Polak JF, Bovill E, Gottdiener JS . Traditional risk factors and subclinical disease measures as predictors of first myocardial infarction in older adults: The Cardiovascular Health Study. Arch Intern Med 1999; 159: 1339–1347.
Eckel R . Obesity in heart disease. A statement for healthcare professionals from the Nutrition Committee, American Heart Association. Circulation 1997; 96: 3248–3250.
Haddock CK, Poston WSC, Taylor JE, Conard M, Spertus J . Smoking and health outcomes following percutaneous coronary intervention. Am Heart J 2003; 145: 652–657.
Acknowledgements
This study was supported partially by a grant awarded by the Searle Pharmaceutical entitled ‘Post-Revascularization and Recovery Study.’ Work on this manuscript was supported by grants from the Agency for Healthcare Research and Quality (AHRQ – 3RO1 HS011282-02S1) and the National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK – 1RO1 DK064284-01).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Carlos Poston, W., Haddock, C., Conard, M. et al. Impact of obesity on disease-specific health status after percutaneous coronary intervention in coronary disease patients. Int J Obes 28, 1011–1017 (2004). https://doi.org/10.1038/sj.ijo.0802703
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802703
Keywords
This article is cited by
-
Association between obesity and health-related quality of life in patients with coronary artery disease
International Journal of Obesity (2010)
-
Effect of Obesity on Short‐ and Long‐term Mortality Postcoronary Revascularization: A Meta‐analysis
Obesity (2008)