Abstract
This study aimed to investigate the incidence, remission and risk factors of non-alcoholic fatty liver disease (NAFLD) among a general population with a 6-year follow-up. In total, 691 individuals from the general population in Jilin, China aged 20–75 years participated in two independent cross-sectional surveys carried out in 2007 and 2013. After excluding patients with alcoholism, viral hepatitis and other liver diseases, 646 individuals were finally enrolled in our study. Of the 646 subjects, 512 did not have NAFLD at baseline, while 134 did. Of the 512 individuals without NAFLD at baseline, 188 (36.7%) developed NAFLD during the six-year follow-up period. The baseline body mass index (BMI, OR = 1.49, 1.36–1.64), high-density lipoprotein cholesterol level(HDL-C) (OR = 0.35, 0.16–0.76) and weight gain (OR = 1.22, 1.16–1.29) were independent predictors for NAFLD incidence. Of the 134 subjects with NAFLD at baseline, 33 (24.6%) had no evidence of NAFLD after 6 years. Males (OR = 4.85, 1.98–11.92) and baseline BMI levels (OR = 0.81, 0.70–0.94) were associated with NAFLD remission. Among the general population, the incidence of NAFLD mainly depended on baseline weight and weight gain. Subjects with mild baseline weights and male subjects were prone to NAFLD remission.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD) is one of the most common liver diseases, currently affecting 25% of adults worldwide1. Although simple NAFLD is usually benign and does not frequently progress to more advanced stages of liver disease2, it is an increasing public health concern and has become a major risk factor for cardiovascular disease, cirrhosis and hepatocellular carcinoma (HCC) because of its high prevalence3,4. In terms of illness burden, strategies for the primary prevention and treatment of NAFLD are necessary, as they have the potential to save millions of patients’ lives worldwide. NAFLD is a slowly progressive disease, and detailed knowledge about its incidence rates and natural course of progression, which are not fully elucidated, is essential. A follow-up cohort programme is needed to ascertain NAFLD outcomes among the general population, including incidence, remission and related risk factors.
Hamaguchi et al. reported that the incidence and remission rates of NAFLD were 10% and 16%, respectively, and found metabolic syndrome to be a strong predictor of NAFLD among a convenience sample of 4401 Japanese employees during only a 1.1 year follow-up period5. Sung et al. revealed that the development of new fatty liver was associated with increased risks of hypertension in 11,448 patients without hypertension at baseline over a five year follow-up period6. During a relative long follow-up period (8.5 years), the Dionysos study reported that ethanol intake was the only risk factor for NAFLD incidence and for the resolution of existing fatty livers7. Although the above studies on NAFLD incidence and remission are available, drawing firm conclusions regarding people in the general population remains difficult. We selected subjects who participated in two surveys conducted among the general population in 2007 and 2013 in Dehui, Jilin Province of China. This study aimed to determine the incidence or remission of NAFLD and the related predictive factors during a 6-year prospective follow-up period.
Results
Characteristics of the study population
As outlined in Fig. 1, 691 subjects participated in both the 2007 and 2013 surveys, and 646 co-participants were enrolled our study after excluding individuals with viral hepatitis (hepatitis B surface antigen (HBsAg) +/anti-hepatitis C virus (anti-HCV) +, n = 34), alcohol abuse (mean ethanol consumption ≧140 g/week in men and ≧70 g/week in women during the past month, n = 10) and other known liver diseases (n = 1). To test for selection bias, the 646 subjects were compared to all subjects from 2007; subjects from the latter population with alcoholism, viral hepatitis and other known liver diseases were also excluded to ensure that the two groups were consistently composed. No differences in the main demographics, anthropometric parameters or biochemical parameters (selected variables are presented in Table 1) were observed between the two groups.
Of the 646 repeat participants, 512 (79.3%) did not have NAFLD, and 134 (20.7%) were classified as having NAFLD at baseline (Fig. 1). The characteristics of the repeat population are shown in Table 2. In all patients, the body mass index (BMI), waist circumference (WC), systolic blood pressure (SBP), alanine transaminase (ALT), aspartate transaminase (AST), γ-glutamyl transpeptidase (GGT), total cholesterol (TC), triglycerides (TG) and fasting blood glucose (FBG) parameters increased significantly in all patients, but the low-density lipoprotein cholesterol (LDL-C) and high-density lipoprotein cholesterol (HDL-C) statistics decreased significantly in the 2013 subjects compared to those in the 2007 subjects. The prevalence of diabetes, dyslipidaemia, NAFLD, hyper-TC, hyper-TG and hypo-HDL-C increased significantly, while the prevalence rates of obesity, overweight and hypertension showed slight increases (significance was not observed). However, the prevalence of hyper-LDL-C decreased significantly. In subjects with NAFLD at baseline (n = 134), the BMI and overweight/obesity rates showed slight decreases, though the changes were not significant. The WC, diastolic blood pressure (DBP), and TG measurements as well as the prevalence of hypertension, dyslipidaemia, hyper-TC and hyper-TG were not significantly different among the two groups, and the prevalence of diabetes increased after 6 years. In subjects without NAFLD at baseline (n = 512), the BMI, WC, SBP, GGT, ALT, AST, TC, TG, FBG measurements and the prevalence of overweight, obesity, dyslipidaemia, hyper-TC, hyper-TG and hypo-HDL-C were increased significantly. The prevalence rates of hypertension, diabetes and hyper-LDL-C were not significantly different.
Factors predicting NAFLD incidence
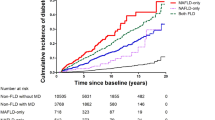
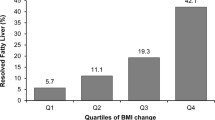
In a sub-analysis of the 512 subjects without NAFLD at baseline, the NAFLD incidence rate at the 6-year follow-up was 36.7% (188/512, annual incidence: 6.1%). The baseline characteristics of the incidence group and the group remaining free from NAFLD are shown in Table 3. Subjects with NAFLD at the 6-year follow-up had higher baseline BMI, WC, TG and LDL-C measurements. The obesity prevalence of the subjects (188) who developed NAFLD was more than eight times that of the other group (324) at baseline (10.1% vs. 1.2%, p < 0.001, Table 3). Notably, the subjects with NAFLD gained significantly more weight than those who did not have NAFLD (2.8 (0, 5.1) vs. 0.5 (1.5, 2.7), Fig. 2). In multivariate logistical regression analysis, the baseline BMI, HDL-C and weight gain measurements remained significantly and independently associated with NAFLD incidence after adjusting for age and gender (Table 4).
Weight changes in subjects with NAFLD incidence vs. subjects who did not develop NAFLD (based on the cohort with normal livers at baseline, n = 512) and remitted NAFLD patients vs. subjects with sustained NAFLD (based on the cohort with NAFLD at baseline, n = 134). The results are expressed as median values (25th quartile, 75th quartile); NAFLD, non-alcoholic fatty liver disease.
Factors predicting complete NAFLD remission
In a sub-analysis of 134 subjects diagnosed with NAFLD at baseline, the NAFLD remission rate during this period was 24.6% (33/134, annual remission: 4.1%). The baseline characteristics of the subjects who achieved or failed to achieve remission are presented in Table 5. The prevalence of obesity in subjects who still had NAFLD was higher than that of subjects in remission, while there were no differences in the prevalence rates of diabetes, hypertension and dyslipidaemia among the two groups (Table 4). In addition, there were no significant differences in weight changes between the subjects still having NAFLD and those in remission (−0.7 (−4.15, 2.2) vs 0.9 (−4.5, 3.25), Fig. 2). Though the subjects in remission maintained the same weight (from 70 (61.5, 77.5) to 70.8 (60.4, 77.9), their TG levels slightly decreased (from 2.14 (1.35, 2.90) to 1.91 (1.31, 2.83), p = 0.743) after 6 years. The baseline BMI measurements and male sex were independently associated with NAFLD remission in multiple logistical regression analysis using a forward (likelihood ratio) approach (Table 4).
Moreover, the weight gain of the subjects with NAFLD at baseline (−0.45 (−4.35, 2.70)) was significantly lower than that of subjects free from NAFLD at baseline (1.35 (−1.00, 3.98)).
Discussion
In this study, we took advantage of the availability of a relatively large cohort of people from the general population who participated in both surveys. Unlike previous large follow-up studies performed on patients, none of the subjects enrolled in our study abused alcohol, and their liver enzymes were mostly normal7.
Our results clearly showed that the prevalence of NAFLD increased from 20.7% to 44.7% after 6 years, which was significantly higher than the world average level1. During the 6-year period, 36.7% of the subjects free from NAFLD at baseline ultimately developed NAFLD, as evidenced by regular ultrasonography. This incidence rate was obviously higher than those among the general populations utilized in Zelber-Sagi’s study (20% with 7-year follow up, annual incidence: 2.86%)8 and Hamaguchi’s study (8.6%/year)5. At first glance, the incidence rate the among general population was expected to be lower than that in the Dionysos study, which did not exclude alcohol drinkers and was performed on patients with elevated liver enzymes (10% incidence rate with 8.5-year follow up)7. However, we observed the opposite result, which could have been due to differences in the demographical characteristics, race and gender distributions, or most importantly, in the economic areas. The incidence rate in our study was still higher than that found in a Hong Kong study (13.5% developed NAFLD in 3–5 years) even though the racial characteristics of the two studies were close9. However, the incidence rate in our current study was close to that found in a Sri Lankan study (43.4% incidence rate with a 7-year follow up, annual incidence: 6.2%)10, which may be related to the fact that both Sri Lanka and China are developing countries.
Because previous studies have demonstrated that both NAFLD and NAFLD incidence are intimately connected with obesity, diabetes and metabolic syndrome9,11, it was not surprising that various parameters, such as BMI, LDL-C, and weight gain, were found to be independent predictors for NAFLD in this 6-year follow-up study. Thus, our findings implied that baseline weight and weight gain are more risky for NAFLD incidence than other metabolic risk factors, such as diabetes and hypertriglyceridemia, which may be explained be the fact that overweight/obese subjects have a higher prevalence rate than subjects with a normal BMI12. While the importance of obesity for NAFLD development has been demonstrated in previous studies8,10,13,14, NAFLD incidence cannot be prevented by regulating body weight within the normal range. Indeed, insulin resistance develops during weight gain even if the subject is within the normal range of weight15. Therefore, having a BMI within the normal limit does not guarantee the prevention of NAFLD development9, which is improperly called “lean NAFLD”. Younsossi et al. found that “lean NAFLD” patients were independently associated with diabetes when compared to lean controls and with female sex, dyslipidaemia and insulin resistance when compared with obese/overweight NAFLD patients16.
The high prevalence and incidence of NAFLD highlights its growing burden in developing economies, such as China. Thus, in addition to controlling weight gain, targeting more community-based effective measures to reduce other metabolic risk factors, such as diabetes and dyslipidaemia, appears to be a critical method for decreasing the prevalence and incidence of NALFD. If not controlled, NAFLD is expected to become the most common indication of chronic liver disease11.
Regarding NAFLD remission, 24.6% of our study population with NAFLD at baseline were in remission after 6 years (annual remission: 4.1%), which was somewhat lower than the one third of individuals achieving NAFLD remission after 7 years8 and the 50% of the study population achieving this status after 8 years7 in other studies.
NAFLD is more likely to develop and less likely to regress5. As we mentioned that weight gain was a predictor of NAFLD incidence in the previous paragraph, we also investigated whether weight loss was a predictor of NAFLD remission. This view has been confirmed by many studies. Some studies suggested that a 5% weight reduction may be sufficient for improving histological steatosis17 and serum ALT levels18. Zelber-Sagi et al. revealed that a weight loss of 2.7 ± 5.0 kg was significantly associated with NAFLD remission, and a 75% remission rate was observed among NAFLD subjects who lost more than 5% of their baseline weight. Therefore, weight reduction is considered the best available treatment option for NAFLD8. However, the regression of NAFLD is not entirely dependent on weight loss. For instance, one study found that serum uric acid levels were associated with NAFLD remission in Chinese males19. In addition, Korean data implied that moderate-to-vigorous exercise is beneficial for improving the resolution of an existing fatty liver regardless of BMI changes during the follow-up period20. Thus, controlling or reducing the metabolic factors associated with NAFLD development and strengthening exercise regimes should promote NAFLD regression. Our current study showed that some NAFLD subjects in remission did not lose weight during the 6-year period. Indeed, we found that the baseline BMI measurement was associated with NAFLD remission, as the NAFLD subjects with relatively mild baseline weights that maintained their weight throughout the 6-year period had a high probability of NAFLD remission. Our study could not deny that slightly decreased TG levels may have contributed to NAFLD remission to some extent. Additionally, our study results showed that males were prone to NAFLD remission, and the female sex was previously demonstrated to be an NAFLD risk factor in other studies16,20. The reason underlying this association may be related to the hormone levels in women. However, the cohort sample size of 134 subjects was relatively small and needs to be expanded in additional studies to validate this result.
Additionally, the subjects with NAFLD at baseline controlled their weight better than others, perhaps because they had better health awareness than subjects without NAFLD at baseline.
To our knowledge, this is the first study on the incidence and remission of NAFLD performed on a representative sample from the general Chinese population. However, this study does have several limitations. First, certain risks for selection bias remained even though the main parameters of the repeat population did not differ from those of the total population.
Second, the presence or absence of NAFLD was diagnosed by ultrasonography, which may be less sensitive than the liver biopsy method if the levels of liver fat are approximately 30%. Moreover, ultrasonography cannot detect inflammation and/or fibrosis. Third, information on exercise and alcohol consumption was obtained only by directly questioning the participants. Fourth, the sample size of 134 NAFLD patients was relatively small, and the exercise time classification was not sufficiently precise.
In conclusion, this cohort study showed that the incidence of NAFLD among a general Chinse population was high during a 6-year follow-up period. NAFLD incidence was associated with baseline BMI, HLD-C and weight gain measurements, and 24.6% of the patients who had NAFLD at baseline had no evidence of the disease after 6 years. Subjects that had mild baseline weights and subjects that were male had the highest probabilities of achieving NAFLD remission.
Materials and Methods
Study population and data collection
In both 2007 and 2013, two independent population-based cross-sectional surveys were conducted with a two-stage stratified sampling method to recruit participants aged 20–75 years in Dehui City, which is representative of Jilin province in terms of economic and cultural development, as described in our previous study21. The designs of both studies were similar, and 691 individuals who completed the first survey (2007) also participated in the 2013 survey. A total of 646 residents were enrolled in our study after excluding subjects with viral hepatitis and other known liver diseases as well as those on medication for liver disease and those abusing alcohol.
On both occasions, all subjects were fasted overnight (between 12 and 14 h) prior to undergoing a comprehensive medical examination, including a face-to-face interview by a trained interviewer, clinical and anthropometric measurements (weight, height, WC and BP), biochemical and serological tests (liver enzymes, serum lipid profile, FBG, and HBsAg/anti-HCV tests), and liver ultrasound for the diagnosis of NAFLD. Some of the questionnaire items were as follows: (i) Assess your physical activity level (1. never; 2. <2 hour/day; 3. ≥2 hour/day). (ii) Do you smoke? If yes, have you stopped smoking or how long have you smoked? (iii) Do you drink alcohol? If yes, how long have you been drinking alcohol, and how much do you drink per day? (iv) Describe your diet habits, i.e., do you eat salty, greasy or lighter food? The participants were instructed to take off heavy clothing and shoes before the anthropometric measurements were taken. The BMI was equated to body weight in kilograms divided by height squared in metres. BP was measured two times at 2-min intervals after a 10-minute rest, and the SBP and DBP were calculated based on the average of the two readings. Blood examinations were completed by The First Hospital of Jilin University laboratory department. Ultrasonography was performed on all subjects participating in the two surveys by experienced radiologists who were blinded to individual subject data using the same equipment (180 ultrasound machine with a 3.5 MHz probe, GE Health Care, Wilmington, MA, USA). This study protocol was approved by The First Hospital of Jilin University Ethics Committee, and all methods were carried out in accordance with approved guidelines. Moreover, all the participants provided written informed consent.
Disease definitions
Diabetes was defined as an FPG ≥7.0 mmol/L, a self-reported history, or the use of insulin or oral hypoglycaemic agents22.
Hypertension was defined as an SBP ≥140 mmHg, a DBP ≥90 mmHg, a previous diagnosis disease by a physician, and/or the use of an antihypertensive medication within the past 2 weeks regardless of BP readings23.
We referred to the Chinese standards for adult obesity as follows: 18.5 kg/m2 ≤ BMI <24 kg/m2 was considered normal, 24 kg/m2 ≤ BMI <28 kg/m2 was considered overweight, and a BMI ≥28 kg/m2 was considered obese24.
Dyslipidaemia was defined as meeting at least one of the following criteria: TC ≥5.18 mmol/L, TG ≥1.7 mmol/L, HDL-C <1.04 mmol/L or LDL-C ≥3.37 mmol/L25.
According to criteria from the “Chinese guidelines on non-alcoholic fatty liver disease (2010)”, NAFLD was diagnosed if the following conditions were met: 1) mean ethanol consumption <140 g/week in men and <70 g/week in women during the past month, 2) negative for HBsAg and anti-HCV, 3) fatty liver diagnosed by ultrasound, and 4) no other liver diseases26.
Statistical analysis
Data were collected and analysed using SPSS 20 (SPSS, Inc., Chicago, IL, USA). Continuous variables were tested using the Kolmogorov-Smirnov test for normality, and non-normal data were presented as medians and quartiles. The Mann-Whitney U test and Wilcoxon signed ranks test were used to assess differences between two independent samples and paired samples, respectively. Categorical variables were presented as frequencies (percentages) and analysed using the Chi-squared test. Multivariate logistical regression analysis was used to identify candidate predictors of NAFLD incidence and remission using a forward (likelihood ratio) approach, whereas the goodness-of-fit of the model was assessed by Hosmer-Lemeshow statistics. P values < 0.05 were considered statistically significant.
References
Younossi, Z. M. et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 64, 73–84 (2016).
Hardy, T., Oakley, F., Anstee, Q. M. & Day, C. P. Nonalcoholic Fatty Liver Disease: Pathogenesis and Disease Spectrum. Annu Rev Pathol 11, 451–496 (2016).
Targher, G., Day, C. P. & Bonora, E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med 363, 1341–1350 (2010).
Pais, R. et al. Temporal trends, clinical patterns and outcomes of NAFLD-related HCC in patients undergoing liver resection over a 20-year period. Aliment Pharmacol Ther (2017).
Hamaguchi, M. et al. The metabolic syndrome as a predictor of nonalcoholic fatty liver disease. Ann Intern Med 143, 722–728 (2005).
Sung, K. C., Wild, S. H. & Byrne, C. D. Development of new fatty liver, or resolution of existing fatty liver, over five years of follow-up, and risk of incident hypertension. J Hepatol 60, 1040–1045 (2014).
Bedogni, G. et al. Incidence and natural course of fatty liver in the general population: the Dionysos study. Hepatology 46, 1387–1391 (2007).
Zelber-Sagi, S. et al. Predictors for incidence and remission of NAFLD in the general population during a seven-year prospective follow-up. J Hepatol 56, 1145–1151 (2012).
Wong, V. W. et al. Incidence of non-alcoholic fatty liver disease in Hong Kong: a population study with paired proton-magnetic resonance spectroscopy. J Hepatol 62, 182–189 (2015).
Niriella, M. A. et al. Incidence and risk factors for non-alcoholic fatty liver disease: A 7-year follow-up study among urban, adult Sri Lankans. Liver Int 37, 1715–1722 (2017).
Marchesini, G. & Mazzotti, A. NAFLD incidence and remission: only a matter of weight gain and weight loss? J Hepatol 62, 15–17 (2015).
Vos, B. et al. Lean non-alcoholic fatty liver disease (Lean-NAFLD): a major cause of cryptogenic liver disease. Acta Gastroenterol Belg 74, 389–394 (2011).
Kim, H. K. et al. Effect of body weight and lifestyle changes on long-term course of nonalcoholic fatty liver disease in Koreans. Am J Med Sci 337, 98–102 (2009).
Chang, Y. et al. Weight gain within the normal weight range predicts ultrasonographically detected fatty liver in healthy Korean men. Gut 58, 1419–1425 (2009).
Erdmann, J. et al. Development of hyperinsulinemia and insulin resistance during the early stage of weight gain. Am J Physiol Endocrinol Metab 294, E568–575 (2008).
Younossi, Z. M. et al. Nonalcoholic fatty liver disease in lean individuals in the United States. Medicine (Baltimore) 91, 319–327 (2012).
Harrison, S. A., Fecht, W., Brunt, E. M. & Neuschwander-Tetri, B. A. Orlistat for overweight subjects with nonalcoholic steatohepatitis: A randomized, prospective trial. Hepatology 49, 80–86 (2009).
Suzuki, A. et al. Effect of changes on body weight and lifestyle in nonalcoholic fatty liver disease. J Hepatol 43, 1060–1066 (2005).
Zhou, Z. et al. Associations between Serum Uric Acid and the Remission of Non-Alcoholic Fatty Liver Disease in Chinese Males. PLoS One 11, e0166072 (2016).
Sung, K. C. et al. Effect of exercise on the development of new fatty liver and the resolution of existing fatty liver. J Hepatol 65, 791–797 (2016).
Wu, J. et al. Six-year changes in the prevalence of obesity and obesity-related diseases in Northeastern China from 2007 to 2013. Sci Rep 7, 41518 (2017).
American Diabetes, A. Standards of medical care in diabetes–2011. Diabetes Care 34(Suppl 1), S11–61 (2011).
Chobanian, A. V. et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 42, 1206–1252 (2003).
Zhou, B. F. & Cooperative Meta-Analysis Group of the Working Group on Obesity in, C. Predictive values of body mass index and waist circumference for risk factors of certain related diseases in Chinese adults–study on optimal cut-off points of body mass index and waist circumference in Chinese adults. Biomed Environ Sci 15, 83–96 (2002).
Joint Committee for Developing Chinese guidelines on, P. & Treatment of Dyslipidemia in, A. Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi 35, 390–419 (2007).
Fan, J. G. et al. Guidelines for the diagnosis and management of nonalcoholic fatty liver disease: update 2010: (published in Chinese on Chinese Journal of Hepatology 2010; 18:163-166). J Dig Dis 12, 38–44 (2011).
Acknowledgements
This study was supported by the National Science and Technology Major Project (2014ZX10002002), the National Basic Research Program of China (973 program) (2015CB554304), the National Natural Science Foundation of China (grants 81373057, 81301472, 81270484, and 81301415), the Finance Department Program of Jilin Province (grant 3D5148193428), the Finance Department Program of Jilin Province (grant D5157453428) and the Finance Department Program of Jilin Province (grant 3D5148503428). We would like to thank our colleagues at The First Hospital of Jilin University for contributing their professional skills, making this study possible.
Author information
Authors and Affiliations
Contributions
Junqi Niu and Chunyan Wang: Conceived and designed the whole study. Jing Wu: (1) Member of the investigation group in 2007 and 2013; (2) Collected and analyzed the research data; (3) Wrote the manuscript. Shumei He: (1) Member of the investigation group in 2007 and 2013; (2) give some advice on NAFLD, especially revisions. Hongqin Xu: (1) Member of laboratory group; (2) give some suggestions of the statistical aspects of revision manuscript. Xiumei Chi: The leader of laboratory group. Jie Sun: Member of the investigation group in 2007 and 2013. Xiaomei Wang, Xiuzhu Gao and Ruihong Wu: Members of laboratory group. Mingbai Shao and Heng Zhao: Members of the investigation group in 2013. Jing Jia: Ultrasound doctor. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, J., He, S., Xu, H. et al. Non-alcoholic fatty liver disease incidence, remission and risk factors among a general Chinese population with a 6-year follow-up. Sci Rep 8, 7557 (2018). https://doi.org/10.1038/s41598-018-25641-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-018-25641-z
This article is cited by
-
The associations between changes in hepatic steatosis and heart failure and mortality: a nationwide cohort study
Cardiovascular Diabetology (2022)
-
Danshao Shugan Granule therapy for non-alcoholic fatty liver disease
Lipids in Health and Disease (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.