Abstract
Volumetric and morphometric studies have demonstrated structural abnormalities related to chronic epilepsies on a cohort- and population-based level. On a single-patient level, specific patterns of atrophy or cortical reorganization may be widespread and heterogeneous but represent potential targets for further personalized image analysis and surgical therapy. The goal of this study was to compare morphometric data analysis in 37 patients with temporal lobe epilepsies with expert-based image analysis, pre-informed by seizure semiology and ictal scalp EEG. Automated image analysis identified abnormalities exceeding expert-determined structural epileptogenic lesions in 86% of datasets. If EEG lateralization and expert MRI readings were congruent, automated analysis detected abnormalities consistent on a lobar and hemispheric level in 82% of datasets. However, in 25% of patients EEG lateralization and expert readings were inconsistent. Automated analysis localized to the site of resection in 60% of datasets in patients who underwent successful epilepsy surgery. Morphometric abnormalities beyond the mesiotemporal structures contributed to subtype characterisation. We conclude that subject-specific morphometric information is in agreement with expert image analysis and scalp EEG in the majority of cases. However, automated image analysis may provide non-invasive additional information in cases with equivocal radiological and neurophysiological findings.
Similar content being viewed by others
Introduction
High-resolution T1-weighted magnetic resonance imaging (MRI) is part of todays epilepsy protocol recommendations1, since they allow readers to identify structural abnormalities associated with temporal lobe epilepsy (TLE). Beyond expert rating, these datasets can be further used for computer-assisted quantitative image analysis to generate rater-independent biological fingerprints. In contrast to cohort-based identification of aberrant large-scale network structures, these fingerprints may provide additional diagnostic information for the individual patient suffering from epilepsy2,3 if expert readings and electroencephalographic (EEG) findings are equivocal.
Large-scale structural abnormalities suggest a common structural framework for TLE4,5,6. Several neuroimaging studies implicate that these abnormalities are not restricted to the hippocampus ipsilateral to seizure onset, but extend along the cingulate cortex, insula, thalamus and frontal lobes, even on the contralateral hemisphere7,8,9,10,11,12,13,14,15,16,17. While these findings pose a potential role for image-based classification, widespread application on the individual level is hampered by large inter-subject and cohort-dependent variability7. Findings are biased by sex, age, duration and hemispheric lateralization of the epilepsy subtype or by combinations with other conditions, as e.g. neurodegenerative disease.
So far, studies on the potential impact of automated analysis on individual diagnosis have provided conflicting results. While some authors demonstrated an additional yield of voxel based morphometry (VBM) for analysis2,18,19,20,21,22,23,24, others stressed the poor sensitivity and specificity of morphometric grey matter (GM) alterations7,25. Despite these limitations, Thesen et al.26 and Hong et al.3 suggested surface based morphometry (SBM) to detect focal cortical dysplasias in candidates for epilepsy surgery. Studies that demonstrated the feasibility of morphometric features (e.g. GM volume, cortical thickness, surface areas or curvatures) to classify patients with psychiatric disorders and epilepsy have recently been reported27,28,29,30,31.
In the present study, we suggest an automated analysis pipeline and statistical framework32 to generate personalised reports of brain morphometry without user intervention using the free software packages FSL33 and FreeSurfer34,35. The localizing value of the morphometric reports were compared against those of expert ratings of scalp EEG and MRI. Regional morphometric parameters of cortical and subcortical structures and their interhemispheric asymmetries (N = 2,976 features altogether) were extracted from single patient scans and statistically compared to 323 healthy control datasets accounting for age, sex and scanning parameters. The feasibility and validity of the proposed framework were evaluated on 47 T1-weighted high-resolution images from 37 patients with mesial temporal lobe epilepsies and hippocampal sclerosis (MTLE-HS) or lateral temporal lobe epilepsies (LTLE). FDG-PET or intracranial EEG information was not part of the standard evaluation programm at our center. Our study assessed the following questions: (1) How frequently are structural abnormalities obscured to visual rating? (2) Do structural abnormalities contribute to lateralization and sublobar determination of the seizure onset zone or of the resection site in individual patients?
Results
Clinical data and quality control
Clinical presentation and MR examinations of patients are summarized in Table S1 of the Supporting Information (SI). Statistical differences between subtypes of temporal lobe epilepsies were limited to the age distribution. Patients in the right LTLE subtype were significantly younger than in both MTLE-HS subtypes (Kruskal-Wallis test and post-hoc pair-wise Mann-Whitney-Wilcoxon tests). 5/47 MRIs (11%) did not pass our quality assessment due to failure of reconstruction or parcellation of the cortical surface and were excluded from further analysis, see Table S2 of the SI. Overall, 13/37 patients underwent epilepsy surgery (18/42 datasets with morphometry, i.e. 43%).
Personalized analysis
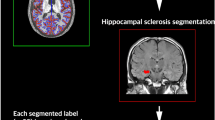
For illustration, a case of left-sided MTLE-HS is provided in Fig. 1 (dataset P005). Scalp EEG findings were not lateralizing. Expert analysis of the MRI identified left-hemispheric hippocampal as well as cortical atrophy (elevated cerebro-spinal fluid (CSF) and reduced GM volumes, pronounced in the left parietal and occipital lobe). The right hippocampus was considered normal by expert analyis. Automated morphometric analysis revealed reduced hippocampal volume on the left (2.1 ± 0.2 ml, volume estimate with uncertainty derived from repeated MRIs in the healthy control database32, p = 0.001). The volume of the left amygdala was at the lower end of the normal range (0.9 ± 0.2 ml, p = 0.034). The corresponding volumes on the right side were normal (hippocampus: 3.8 ± 0.3 ml, amygdala 1.5 ± 0.2 ml). Asymmetry of the hippocampus (p < 10−14), the pallidum (p < 10−16) and the putamen (p < 10−8, each of them smaller in the left hemisphere) were most significant. Morphometric analysis of cortical surface parcellations revealed widespread unilateral changes on the left hemisphere.
T1-weighted MRI and standardized result presentation for dataset P005, a MTLE-HS patient with left-sided seizure onset. In the top row three axial and two coronal slices are shown. The images are displayed according to “neurological” convention, i.e. the left side of the images corresponds to the left hemisphere. The gray-white matter interface found by FreeSurfer is displayed as a blue and the pial surface as a red line. Voxels corresponding to surface parcellations with abnormally high Gaussian curvature are highlighted with red-to-yellow coloring and voxels corresponding to reduced cortical thickness with blue-to-white coloring. The mean cortical thickness (middle row) was reduced in the left lateral occipito-temporal gyrus with and without eTIV normalization (p = 0.002). With odds of 17.2 the confidence in a valid (vs. artefactual) observation was high, especially after eTIV normalization. The corresponding structure on the right hemisphere and the asymmetry index were still within the normal range. The Gaussian curvature (bottom row) of the lateral aspect of the superior temporal gyrus was asymmetric (p = 0.005), with highly significantly increased curvature on the left (p < 10−6). Again, odds >8 gave confidence in reliable observations.
Elevated abnormality rates in patients with temporal lobe epilepsy
We detected significantly higher abnormality rates in patients with TLE than in a leave-one-out cross-validation dataset of healthy controls32 (Table 1). Moreover, in datasets that had to be excluded due to quality issues, the “abnormality detection rate” was erroneously three times higher than in the datasets passing the checks. A more detailed analysis of the different morphometric parameters (not shown) revealed that asymmetry of hippocampal volumes was the most frequent observation in MRIs of individual patients with TLE (detected in 48% of datasets after normalization to the estimated total intracranial volume, eTIV), followed by volume loss of the left pallidum (21%) and ipsilateral hippocampus (17%). The asymmetry indices of volume segmentations (15% overall) were about six times more frequently abnormal in patients with TLE than in healthy subjects. Hippocampal asymmetry was significant in 83% of datasets with MTLE-HS but in none with LTLE. This difference between TLE subtypes was highly significant (p < 10−5, randomization test).
Relation with epilepsy surgery
In patients who underwent successful epilepsy surgery, structural abnormalities were present at the site of resection on a sublobar level in 10/14 datasets that passed quality control (71%, see Table 2). All these detections were considered specific, since at least one of the three most significant abnormalities overlapped with the resected epiletogenic zone). There was a strong trend towards higher agreement in MTLE-HS than in LTLE (p = 0.015, randomization test). In surgery cases with consistent expert MRI and EEG rating an overlap of morphometric detections with the resection site was found in 5/5 datasets (100%). The overlap fraction in equivocal datasets (3/5 = 60%) was not significantly smaller (p = 0.333, exact test).
Comparison with expert image analysis
As expert image reading is part of the routine clinical workup of epilepsy patients, we assessed the performance of our framework to detect morphometric alterations with expert detections as ground truth (GT), see SI for details. The essence of abnormalities detected by our quantitative analysis pipeline in comparison to expert reading of the MRI and scalp EEG is provided in Table 2 and further information is available in Table S2 of the SI. Expert raters identified 6/37 patients as non-lesional (7/47 of MRI datasets, i.e. 15%). In contrast, automated morphometric analysis was normal only in two MRI datasets (2/42 = 5%). The overall detection rate of structural abnormalities was not significantly different between automated analysis and readers (p = 0.082, randomization test). While the expert readers reported a higher fraction of non-lesional MRIs in LTLE than in MTLE-HS (p = 0.001), automated detection was independent from the TLE subtype.
The overall sensitivity of automated detections with Lr ≥ 2 according to equation (2) (see Methods section for details) to abnormalities reported by the expert readers was 0.806 (29/36 lesional MRIs that passed quality control, see Table 2). The overall specificity was 0.694 (25/36 MRIs). Specificity tended to be higher in MTLE-HS than in LTLE (p = 0.019, randomization test), while sensitivities were similar. Top 3 abnormalities with Lr ≥ 2 that were overlooked by the expert reader were detected in 36/42 MR datasets (86%).
Regional diagnostic odds ratios (DOR, see Methods section for details) of automatic detections compared to the GT provided by expert reading are presented in Fig. 2 (volume segmentations) and Fig. 3 (surface parcellations). DOR ≫ 1 (red hue) indicate brain regions where the morphometric analysis matched the GT. The overall average DOR was 17.1 with range between 0.333 and 159. DORs ≤ 1 were observed in the thalamic nuclei and not specific for a TLE subtype. A subtype dependence of DOR was observed for surface parcellations, predominantly in the temporal and frontal lobes, see Fig. 3. In MTLE-HS with left-sided seizure onset the expert reported only a small fraction of abnormalities detected by the morphometry tool in the left lateral temporal lobe, which lowered the DOR.
Summaries of regional positive predictive values (PPV) are given in Figure S1 of the SI. In general, PPVs were moderate to small, (overall mean PPV was 0.113), meaning that the regional fraction of correct cases (“true positives” according to expert MRI assessment) among all cases rated abnormal by the morphometry tool (“test positives”) was considerably low. In contrast, negative predictive values (NPV) were in general very close to one, see Figure S2 of the SI, meaning that the vast majority of cases rated normal by the morphometry tool (“test negatives”) were also rated normal by the human expert (“true negatives”). The overall mean NPV was 0.974 and smallest values 0.6 < NPV < 0.7 were observed for atrophy of hippocampi and amygdalae as well as for volume increase of some ventricles, meaning that the informed expert did sometimes report abnormalities in these structures whereas the automated morphometry tool did not.
MRI vs EEG lateralisation
Thirty out of 36 patients with available EEG information (corresponding to 39/46 of MRI datasets, i.e. 85%) presented with focal interictal abnormalities on routine scalp EEG (i.e. focal epileptiform signals and/or focal slowing), see Table S2 of the SI. The sensitivity and specificity of MR matches with the EEG lateralization were considerably low (0.559 and 0.500, see Table 2).
MRI and EEG localization by the expert overlapped in 18/24 patients (75%). This corresponded to 17 datasets with morphometry and in 14 cases automated detections were consistent with MRI and EEG (82%). However, in 25% of patients the expert ratings of the MRI were either non-lesional or EEG diffuse or both contradictory. In 9/11 of corresponding datasets with available morphometry (82%) detected abnormalities were sensitive for MR lesions according to the expert and in 4/11 datasets (36%) for EEG lateralization. In 4/11 cases some abnormalities were sensitive for MRI lesions and different ones for the EEG lateralization.
Reproducibility of deviations from the norm
We constructed feature vectors of length 2,976 describing the direction and significance of regional deviations of morphometric parameters from the expectation in the healthy population (see Methods section for details) and assessed the reproducibility in repeated MRIs of the same patients by the Pearson correlation matrix (Fig. 4a). Within-patient correlation (median of the 12 off-diagonal matrix elements 0.436, 95% CI [−0.036,0.518]) was highly significantly larger than correlation between different patients (median of 849 matrix elements 0.032, CI [−0.183,0.273]) in a Mann-Whitney-Wilcoxon test (p < 10−6). Also, within-subtype correlation coefficients (repeated MRIs of the same patients excluded, median of 228 matrix elements 0.049, CI [−0.167,0.292]) were larger than between different TLE subtypes (median of 621 matrix elements 0.027, CI [−0.201,0.258], p < 10−3).
Pearson correlation matrices of feature vectors defined in equation (1). In panel a all 2,976 features are used, whereas panels b, c, e and f use only features representative for one TLE subtype. In panel d all features are used that were selected as representative for at least one subtype. Boundaries between datasets corresponding to different subtypes are indicated by black lines.
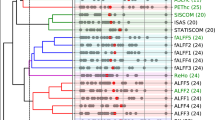
After determining subsets of relevant features (see Methods section), block patterns became apparent in the correlation matrices (Fig. 4b,c,e,f). Two key features for subtype characterization were hippocampal asymmetry and left-hemispheric volume. Surface parcellation features were selected from all morphometric parameters and distributed over large parts of the cortex, see Fig. 5 for the Destrieux altlas and Figure S3 of the SI for the Desikan-Killiany atlas. In addition to parcellations of the temporal lobes also central and parietal parcellations were selected, see Figures S4 to S6 of the SI for mappings of subtype-wise z-values of SBM parameters.
Cortical features of the Destrieux atlas selected to represent at least one of the TLE subtypes. The color coding represents the decadic logarithm of relative feature importances (values for all features add up to one). Abbreviations: A, asymmetry index; L/R, left/right; thicknessstd, standard deviation of cortical thickness; meancurv, mean curvature; gausscurv, Gaussian curvature; curvind, curvature index; foldind, folding index; pctmean, mean percentage change of the grey-white contrast.
Overall, 58/2976 features (1.9%) represented at least one TLE subtype. In contrast to the full feature vectors, the within-subtype correlation coefficients (median 0.347, CI [−0.124,0.869]) turned out highly significantly larger than between subtypes (median 0.009, CI [−0.627,0.335], p < 10−64). The MTLE-HS cases with left and right-sided seizure onset appeared highly anti-correlated in this feature selection (Fig. 4d).
Discussion
Lack of apparent structural epileptogenic lesions (in 15% of datasets in our study) and equivocal EEG findings (in 25% of patients in our study) are frequent observations in patients who are considered candidates for epilepsy surgery. Expert MRI analysis using higher field strength and dedicated epilepsy protocols has improved the detection rates of structural epileptogenic lesions considerably1,36. Modern MR imaging enables high-resolution image acquisition within reasonable acquisition times, enabling additional postprocessing of the structural datasets. Here, we aimed to investigate the additional yield of automated volumetric and morphometric image analysis, using high-resolution T1-weighted sequences32.
Main findings
In cases with consistent human MRI and EEG localization, agreement of morphometric abnormalities on a lobar level was 82%. In non-lesional or inconsistent datasets the morphometric abnormalities co-lateralized with EEG in 36% of cases. Partial overlaps with MRI lesions were 82% and with the resection site 60%.
The overall sensitivity and specificity of sublobar concordance with expert MRI inspection were 81% and 69% and larger for MTLE-HS than for LTLE. Widespread statistical abnormalities, even remote from the EEG focus, including abnormalities in the contralateral hemisphere were detected in the majority of datasets (86%), further supporting the concept of epilepsy as a widespread network disorder4,5.
Diagnostic odds ratios of automatic analysis using expert MRI as ground truth were in general high (Figs 2 and 3). The large negative vs. moderate positive predictive values of quantitative morphometric analysis (Figures S1 and S2 of the SI) fulfill the criteria of a screening test37,38. Volume segmentations and surface parcellations that were not flagged as suspicious by automated morphometric analysis were very likely also to be considered normal by the expert rater. In contrast, a positive detection through the morphometry pipeline did not necessarily imply that the region was also identified by the expert rater. During daily clinical workflow, such subtle morphometric changes31,39 may be overlooked despite being potential target regions that merit a second look by the human expert.
The morphometric feature vectors Lrm defined in equation (1) were highly reproducible and allowed to identify patients with repeated MRIs by elevated Pearson correlation coefficients (Fig. 4a). A similar observation has already been made by Rummel et al.32 for multiple sclerosis patients and healthy controls. As an outlook to forthcoming studies, we demonstrated that heuristic selection of a small number (1.9%) of representative features greatly enhanced the contrast between TLE subtypes (Fig. 4d). Importantly, the heuristic feature selection used hippocampal asymmetry in MTLE-HS patients, but was not limited to ipsilateral mesiotemporal structures. Rather, widespread and bilateral cortical features were selected (Fig. 5), including surface areas and curvatures, which easily escape expert inspection. We interpret this observation as a strong indication that the extracted features may serve as an excellent starting point for syndrome classification using machine learning approaches40.
Limitations
One major limitation of this study is that our pipeline missed a proportion of hippocampal scleroses identified by the expert (8/31, i.e. 26%, see Table S2 of the SI). Expert raters detected predominantly signal changes on T2-weighted and FLAIR images, whereas morphometric analysis by FSL and FreeSurfer was restricted to T1-weighted images. The shortcoming of our morphometric analysis is consistent with Pardoe et al.41, who observed that manual hippocampus segmentation in patients with TLE yielded lower hippocampal volumes and a larger size difference between affected and non-affected hemispheres than automated segmentation. A similar observation was recently made by Kim et al.42, who also found that hippocampal developmental abnormalities and atrophy had a negative impact on the segmentation performance of three state-of-the-art automated methods (including FreeSurfer). Despite these possible negative biases in the methodology, abnormal hippocampal asymmetry or ipsilateral atrophy were the most frequent deviations of the patients observed in temporal lobe epilepsies compared to controls in our study. To overcome the current limitations of morphometric analysis based on FSL and FreeSurfer, specialized tools43,44 may further improve automated analysis. For these approaches, higher volumetric accuracies were reported for hippocampi and amygdalae and detection of hippocampal sclerosis was 100% in nine patients43. Alternatively, combinations with machine learning methods taking into account different imaging modalities and feature maps are expected to overcome this limitation in the near future.
Conclusion
We aimed to investigate the applicability of case–control analyses to identify structural abnormalities in patients with epilepsy using surface-based morphometry and a framework of a customized statistical analysis. A similar approach with VBM volumes has previously been followed by Huppertz et al.2,18,19. Our approach did not outperform expert assessment in terms of lesion detection and subsequent classification of the underlying TLE subtype. In particular, our automated morphometry pipeline shares typical features of screening tests and must not be clinically applied without caution. Rather, automated detections must be followed-up with reinspection by the human experts. Notwithstanding, the fact that our heuristic feature selection enhanced subtype separation (see Fig. 4b–f) is an indication that widespread and subtle alterations escaping the expert’s eye carry information that might be exploited in future attempts to classification. Research in this direction is ongoing.
The fully automated analysis is computationally extensive (approximately ten hours for FreeSurfer and FSL, and two hours for statistics and figure generation), but it does not require time-consuming user intervention. In our study, launching the analysis and performing quality control took approximately three and ten minutes, respectively. Whereas these steps could be done by a technician, reviewing and interpreting the standardized result display requires an expert. It took approximately half an hour in our study. In our view, this means that incorporating the automated pipeline into clinical routine should be feasible without straining available resources. As it passes quality assessment in 89% of cases and can help to exclude non-suspicious brain regions, this tool could potentially be used to support the expert in the identification of structural abnormalities associated with structural epileptogenic lesions. Further studies including a larger cohort of surgery patients with different types of epilepsy are mandatory.
Materials and Methods
This study was approved by the Ethics Committee of the Kanton of Bern in accordance with the Declaration of Helsinki. All patients and healthy controls signed informed consent for usage of their data for research. Any clinical decision making was done prior to and completely independent from the present study. For our retrospective analysis, MRI datasets were evaluated quantitatively, and MRI and EEG exams were re-assessed by neuroradiologists and neurologists. Experts were blinded to morphometric results and MR and EEG analysis techniques are described in detail in the SI. For comparison with automated detections, the neuroradiologist annotated regions with visually detectable abnormalities using the Destrieux atlas45 of surface parcellations.
Patients and healthy controls
We analyzed high-resolution T1-weighted datasets of 37 patients with temporal lobe epilepsies scanned between 2009 and 2015 (17 male and 20 female, age range 18–76 years, see Table S1 of the SI for detailed patient characteristics and Table S3 for scanners and sequence parameters). Epilepsy surgery was not an inclusion criterion. For patients who underwent repeated scanning during their clinical workup at our institution, all available high-resolution T1-weighted MRI datasets were analyzed, resulting in a total of 47 datasets. The repeated MR datasets were used to evaluate the intra-patient reproducibility of our approach.
The normative database is described in detail in Rummel et al.32. It was generated from region-specific morphometric and volumetric parameters evaluated in a control group encompassing 323 high-resolution T1-weighted MRI datasets of 267 neurologically healthy subjects (142 datasets from male and 181 from female subjects, age range 7–79 years). The MRIs of healthy controls (HC) had been acquired during previous studies performed at the Inselspital Bern. Repeated MRIs from the same HCs within less than three years were used to estimate the region and parameter specific measurement errors32. The normative database was fully anonymized after its generation. Only age, sex, MR manufacturer/model and acquisition sequence were retained as confounding variables in anonymized form.
Automated image processing and quality control
All image processing was performed on a quad-core workstation under Ubuntu Linux, release 14.04 LTS using the free software packages FSL and FreeSurfer. For statistics and result display according to Rummel et al.32, self-written Octave scripts were used (CR). Decisions were made at a significance level α = 0.01 and values p < 0.05 were interpreted as marginally significant (trends).
The total volumes of CSF, GM and WM were estimated using FSL (http://fsl.fmrib.ox.ac.uk/fsl/fslwiki/, version 5.033). As additional volume parameters the whole brain volume (i.e. GM + WM) and the intracranial volume (ICV = GM + WM + CSF) were used. For estimation of the volumes of GM, WM and CSF segmentations including the hippocampus and the amygdala, the thalamus, the basal ganglia, the ventricles, the corpus callosum and the cerebellum we used FreeSurfer (https://surfer.nmr.mgh.harvard.edu, version 5.3.0), for details see Fischl et al.34,35. For surface-based morphometry, the interfaces between WM and GM as well as between GM and CSF were estimated with FreeSurfer and the cortex was parcellated automatically46 according to the atlases by Desikan et al.47 and Destrieux et al.45 providing 34 and 74 parcellations per hemisphere, respectively.
Abnormality detection is highly sensitive to errors occurring during FreeSurfer’s automatic surface tesselation, segmentation and parcellation procedures. Any patient datasets that did not pass the automated quality checks described in detail in the SI, and conditional secondary visual controls, were excluded from further analysis. In the healthy controls (N = 323) we did not perform these labor-intensive procedures. Rather, we rejected region and parameter specific statistical outliers, and estimated artifact probabilities as well as odds for valid vs. artifactual measurements following procedures described in detail in Rummel et al.32.
Statistical analysis and standardized result presentation
To account for the physiological age-dependence affecting most morphometric parameters48,49,50,51,52,53, low order polynomial age trends were fitted to the estimates of all 323 members of the normative dataset according to Rummel et al.32. We calculated the probability p that a fit residue of observed magnitude occurred by chance, given the width of the distribution in healthy controls and the estimated measurement error.
Inter-individual differences in general head/brain size54 were accounted for by normalizing raw estimates of the regional morphometric parameters GM volume, cortical surface area, mean and standard deviation of the cortical thickness and all four curvature parameters to FreeSurfer’s estimated total intracranial volume (eTIV). We performed isometric normalization with different scaling exponents n to account for the different scaling relationships between morphometric parameters and head size (n = 1 for volumes, n = 2/3 for areas, n = 1/3 for thicknesses and accordingly for the curvature measures, see Rummel et al.32 for details). Grey-white contrast mainly depends on the MR sequence and thus it was instead regionally normalized to the same mean for each scanner-sequence combination. In brain regions appearing in both hemispheres, we also calculated asymmetry indices for all morphometric parameters. Their range is between −1 for extremely left-dominated and + 1 for extremely right-dominated structures, respectively. For regions with complete morphological symmetry, asymmetry indices equal zero.
To ease clinical translation of high-dimensional morphometric output, we generated standardized morphometry reports32. All regional morphometric parameters were compiled and displayed as a function of age with standardized layout (see Figure S7 of the SI). Brain regions and morphometric parameters with potential abnormalities were highlighted with a yellow figure background if deviations between the patient and the healthy controls had uncorrected significance p < 0.01. Correction for multiple comparisons during extensive testing (2,976 tests for raw and eTIV normalized parameters in each dataset) was performed using the false-discovery rate (FDR)55. Differences that remained significant after FDR correction were highlighted with a red figure background.
Construction of feature vectors
To assess the agreement between automated morphometry and human rating, as well as between patients with repeated MRIs, we converted the normalized p-values of all brain regions r and morphometric parameters m into feature vectors:
of length 2,976 (60 whole brain partial volumes and volume segmentations, 34 plus 74 surface parcellations of the Desikan-Killiany and Destrieux atlases, evaluated on the left and right brain hemisphere plus the asymmetry index, all evaluated for 9 cortical morphometric parameters). In equation (1) the negative sign (resulting in positive L because p < 1) was used if the fit residue was positive (i.e. observation larger than expected), and the positive sign (negative L) if the residues were negative (i.e. observation smaller than expected).
In contrast to volumes of brain segmentations the morphometry pipeline yields nine parameters per surface parcellation. For comparison with expert rating of morphometric abnormalities and accuracy assessment we condensed them into a single statement per cortex region. Asymmetry indices were counted half for each hemisphere. To suppress the influence of potentially artifactual measurements we calculated a weighted average using the odds for valid vs. artifactual measurement32 as weights
Selection of subtype-specific features
The full feature vectors may contain many brain regions and morphometric parameters that are rather unspecific for temporal lobe epilepsies. To explore whether feature vectors Lrm of equation (1) could discriminate TLE subtypes, we evaluated the performance gain expected by filtering out unrepresentative features with low specificity and discriminative power. In a heuristic exploration we employed two principles. Features were required to be (i) highly reproducible within the TLE subtype of interest and (ii) highly unique in the sense that they differentiated between the subtype of interest and all other subtypes.
To assess reproducibility, we searched features where the absolute value of the subtype-wise mean in units of the standard deviation was extraordinarily large. As thresholds the upper and lower quartile ±1.5 inter quartile ranges were used, respectively. To estimate uniqueness, we checked which features had significantly different mean between the TLE subtype of interest and all other subtypes (p < 0.01). Finally, the intersection of both feature sets was used as heuristic feature selection.
Accuracy assessment and statistical testing
To quantify the overall accuracy of automated detections with Lr ≥ 2 according to the human rater, we used the diagnostic odds ratio (DOR)56 defined as the fraction LR + /LR- of the positive to the negative likelihood ratio. LR + is the ratio of probabilities that the morphometry tool correctly detects an abnormality to the tool erroneously claiming a detection if the structure is in fact normal. Conversely, LR- is the ratio of probabilities that the morphometry tool erroneously judges a structure as normal when it is in fact abnormal to a correct normal classification. Important advantages of the DOR are its independence from the prevalence of abnormal structures and the approximately normal distribution of its logarithm. As secondary accuracy statistics, we calculated the positive predictive value (PPV) and the negative predictive value (NPV), yielding (prevalence-dependent) indicators for the fraction of correctly classified abnormal/normal brain regions, respectively.
Throughout the paper between-group differences were assessed by sequential testing. For ordinal data, 1st level testing of the medians was performed using the nonparametric Kruskal-Wallis test. If the differences between all TLE subtypes were at least marginally significant (p < 0.05) the nonparametric Mann-Whitney-Wilcoxon U-test was used in a pairwise manner as a 2nd level test to reveal which subsets differed. For categorial data randomization tests with N = 10,000 resamplings were used for 1st and 2nd level testing of distributional differences. We always tested whether quantifiers depended on the TLE subtype. For brevity we discuss only significant differences in the main text.
Ethics statement
This study was approved by the Ethics Committee of the Kanton of Bern.
Change history
09 January 2018
A correction to this article has been published and is linked from the HTML version of this paper. The error has been fixed in the paper.
References
Wellmer, J. et al. Proposal for a magnetic resonance imaging protocol for the detection of epileptogenic lesions at early outpatient stages. Epilepsia 54, 1977–1987 (2013).
Huppertz, H. J. et al. Enhanced visualization of blurred gray-white matter junctions in focal cortical dysplasia by voxel-based 3D MRI analysis. Epilepsy Res. 67, 35–50 (2005).
Hong, S. J. et al. Automated detection of cortical dysplasia type II in MRI-negative epilepsy. Neurology 83, 48–55 (2014).
Richardson, M. P. Large scale brain models of epilepsy: dynamics meets connectomics. J. Neurol. Neurosurg. Psychiatry 83, 1238–1248 (2012).
Wiest, R. et al. Widespread grey matter changes and hemodynamic correlates to interictal epileptiform discharges in pharmacoresistant mesial temporal epilepsy. J. Neurol. 260, 1601–1610 (2013).
Fornito, A., Zalesky, A. & Breakspear, M. The connectomics of brain disorders. Nature Rev. Neurosci. 16, 159–172 (2015).
Keller, S. S. & Roberts, N. Voxel-based morphometry of temporal lobe epilepsy: an introduction and review of the literature. Epilepsia 49, 741–757 (2008).
Santana, M. T. et al. Auras and clinical features in temporal lobe epilepsy: a new approach on the basis of voxel-based morphometry. Epilepsy Res. 89, 327–238 (2010).
Li, J., Zhang, Z. & Shang, H. A meta-analysis of voxel-based morphometry studies on unilateral refractory temporal lobe epilepsy. Epilepsy Res. 98, 97–103 (2011).
Bernhardt, B. C., Hong, S., Bernasconi, A. & Bernasconi, N. Imaging structural and functional brain networks in temporal lobe epilepsy. Front. Hum. Neurosci. 7, 624 (2013).
Coan, A. C. et al. Frequent seizures are associated with a network of gray matter atrophy in temporal lobe epilepsy with or without hippocampal sclerosis. PLoS One 9, e85843 (2014).
Campos, B. M. et al. White matter abnormalities associate with type and localization of focal epileptogenic lesions. Epilepsia 56, 125–132 (2015).
McDonald, C. R. et al. Regional neocortical thinning in mesial temporal lobe epilepsy. Epilepsia 49, 794–803 (2008).
Woermann, F. G., Free, S. L., Koepp, M. J., Ashburner, J. & Duncan, J. S. Voxel-by-voxel comparison of automatically segmented cerebral gray matter-A rater-independent comparison of structural MRI in patients with epilepsy. Neuroimage 10, 373–84 (1999).
Dupont, S. et al. Temporal pole hypometabolism may be linked to a reduction of grey matter in temporal lobe epilepsy. Neuroreport 13, 2537–2541 (2002).
Bernasconi, N. et al. Whole brain voxel-based statistical analysis of gray matter and white matter in temporal lobe epilepsy. NeuroImage 23, 717–723 (2004).
Bonilha, L. et al. Voxel-based morphometry reveals gray matter network atrophy in refractory medial temporal lobe epilepsy. Arch. Neurol. 61, 1379–1384 (2004).
Huppertz, H. J. et al. Voxel-based 3D MRI analysis helps to detect subtle forms of subcortical band heterotopia. Epilepsia 49, 772–785 (2008).
Huppertz, H. J., Kurthen, M. & Kassubek, J. Voxel-based 3D MRI analysis for the detection of epileptogenic lesions at single subject level. Epilepsia 50, 155–156 (2009).
House, P. M. et al. Comparison of morphometric analysis based on T1- and T2-weighted MRI data for visualization of focal cortical dysplasia. Epilepsy Res. 106, 403–409 (2013).
Wang, Z. I. et al. Voxel-based morphometric MRI post-processing in MRI-negative focal cortical dysplasia followed by simultaneously recorded MEG and stereo-EEG. Epilepsy Res. 100, 188–193 (2012).
Wang, Z. I. et al. Neuroimaging characteristics of MRI-negative orbitofrontal epilepsy with focus on voxel-based morphometric MRI postprocessing. Epilepsia 54, 2195–2203 (2013).
Wang, Z. I. et al. Linking MRI postprocessing with magnetic source imaging in MRI-negative epilepsy. Ann. Neurol. 75, 759–770 (2014).
Wang, Z. I. et al. Voxel-based morphometric magnetic resonance imaging (MRI) postprocessing in MRI-negative epilepsies. Ann. Neurol. 77, 1060–1075 (2015).
Eriksson, S. H. et al. Cortical neuronal loss and hippocampal sclerosis are not detected by voxel-based morphometry in individual epilepsy surgery patients. Hum. Brain Mapp. 30, 3351–3360 (2009).
Thesen, T. et al. Detection of epileptogenic cortical malformations with surface-based MRI morphometry. PLoS One 6, e16430 (2011).
Ecker, C. et al. Investigating the predictive value of whole-brain structural MR scans in autism: a pattern classification approach. NeuroImage 49, 44–56 (2010).
Qiu, L. et al. Characterization of major depressive disorder using a multiparametric classification approach based on high resolution structural images. J. Psychiatry. Neurosci. 39, 78–86 (2014).
Bernhardt, B. C., Hong, S. J., Bernasconi, A. & Bernasconi, N. Magnetic resonance imaging pattern learning in temporal lobe epilepsy: Classification and prognostics. Ann. Neurol. 77, 436–446 (2015).
Peng, X., Lin, P., Zhang, T. & Wang, J. Extreme learning machine-based classification of ADHD using brain structural MRI data. PLoS One 8, e79476 (2013).
Ahmed, B. et al. Cortical feature analysis and machine learning improves detection of “MRI-negative” focal cortical dysplasia. Epilepsy Behav. 48, 21–28 (2015).
Rummel, C. et al. A fully automated pipeline for normative atrophy in patients with neurodegenerative disease. under review at Frontiers in Neurology (2017).
Smith, S. M. et al. Advances in functional and structural MR image analysis and implementation as FSL. NeuroImage 23(Suppl. 1), S208–S219 (2004).
Dale, A. M., Fischl, B. & Sereno, M. I. Cortical surface-based analysis. I. Segmentation and surface reconstruction. NeuroImage 9, 179 (1999).
Fischl, B., Sereno, M. I. & Dale, A. M. Cortical surface-based analysis. II: Inflation, flattening, and a surface-based coordinate system. NeuroImage 9, 195 (1999).
Wellmer, J. et al. Digital photography and 3D MRI-based multimodal imaging for individualized planning of resective neocortical epilepsy surgery. Epilepsia 43, 1543–1550 (2002).
Grimes, D. A. & Schulz, K. F. Uses and abuses of screening tests. Lancet 359, 881–884 (2002).
Maxim, L. D., Niebo, R. & Utell, M. J. Screening tests: a review with examples. Inhal Toxicol. 26, 811–828 (2014).
Duncan, J. S., Winston, G. P., Koepp, M. J. & Ourselin, S. Brain imaging in the assessment for epilepsy surgery. Lancet Neurol. 15, 420–433 (2016).
Wernick, M. N., Yang, Y., Brankov, J. G., Yourganov, G. & Strother, S. C. Machine Learning in Medical Imaging. IEEE Signal Processing Magazine 27, 25–38 (2010).
Pardoe, H. R., Pell, G. S., Abbott, D. F. & Jackson, G. D. Hippocampal volume assessment in temporal lobe epilepsy: How good is automated segmentation? Epilepsia 50, 2586–2592 (2009).
Kim, H. et al. Automatic hippocampal segmentation in temporal lobe epilepsy: impact of developmental abnormalities. NeuroImage 59, 3178–3186 (2012).
Hammers, A. et al. Automatic detection and quantification of hippocampal atrophy on MRI in temporal lobe epilepsy: A proof-of-principle study. NeuroImage 36, 38–47 (2007).
Chupin, M. et al. Automatic segmentation of the hippocampus and the amygdala driven by hybrid constraints: Method and validation. NeuroImage 46, 749–761 (2009).
Destrieux, C., Fischl, B., Dale, A. & Halgren, E. Automatic parcellation of human cortical gyri and sulci using standard anatomical nomenclature. NeuroImage 53, 1–15 (2010).
Fischl, B. et al. Automatically parcellating the human cerebral cortex. Cereb. Cortex 14, 11–22 (2004).
Desikan, R. S. et al. An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. NeuroImage 31, 968–980 (2006).
Good, C. D. et al. A voxel-based morphometric study of ageing in 465 normal adult human brains. NeuroImage 14, 21–36 (2001).
Smith, C. D., Chebrolu, H., Wekstein, D. R., Schmitt, F. A. & Markesbery, W. R. Age and gender effects on human brain anatomy: a voxel-based morphometric study in healthy elderly. Neurobiol. Aging 28, 1075–1087 (2007).
Draganski, B. et al. Regional specificity of MRI contrast parameter changes in normal ageing revealed by voxel-based quantification (VBQ). NeuroImage 55, 1423–1434 (2011).
Becker, J. T. et al. Cross-validation of brain structural biomarkers and cognitive aging in a community-based study. Int. Psychogeriatr. 24, 1065–1075 (2012).
Wierenga, L. et al. Typical development of basal ganglia, hippocampus, amygdala and cerebellum from age 7 to 24. NeuroImage 96, 67–72 (2004).
Wierenga, L. M., Langen, M., Oranje, B. & Durston, S. Unique developmental trajectories of cortical thickness and surface area. NeuroImage 87, 120–126 (2014).
Malone, I. B. et al. Accurate automatic estimation of total intracranial volume: a nuisance variable with less nuisance. Neuroimage 104, 366–372 (2015).
Genovese, C. R., Lazar, N. A. & Nichols, T. Thresholding of statistical maps in functional neuroimaging using the false discovery rate. NeuroImage 15, 870–878 (2002).
Glas, A. S., Lijmer, J. G., Prins, M. H., Bonsel, G. J. & Bossyut, P. M. M. The diagnostic odds ratio: a single indicator of test performance. J. Clin. Epidemiol. 56, 1129–1135 (2003).
Acknowledgements
The authors thank Kathrin Bieri, Regula Everts, Raimund Kottke, Stefan Schweizer and Rajeev K. Verma for contributing imaging data of healthy controls for secondary use. Christian Güder and Martin Zbinden supported us in distributed computing. We thank our MR and EEG technicians for support during data acquisition. This study was supported by the Swiss National Science Foundation (SNF) via the projects 124089 and 140332. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript. S.V. received support from the SNF via grants 320030-169198 and CRSII5_170873. K.S. received support from the SNF via grant 155950.
Author information
Authors and Affiliations
Contributions
C.R., R.W., E.A. and M.H. devised the automated MRI analysis pipeline. Y.B. performed quality control of the MRI processing. N.S., C.W. and R.W. performed expert rating of the MRIs. A.S. and K.S. performed expert rating of the EEGs. C.R. performed the statistical analysis. S.V. and M.S. contributed with helpful inputs throughout the genesis of this work. C.R., N.S., K.S. and R.W. discussed the results and wrote the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Change History: A correction to this article has been published and is linked from the HTML version of this paper. The error has been fixed in the paper.
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A correction to this article is available online at https://doi.org/10.1038/s41598-017-16213-8.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rummel, C., Slavova, N., Seiler, A. et al. Personalized structural image analysis in patients with temporal lobe epilepsy. Sci Rep 7, 10883 (2017). https://doi.org/10.1038/s41598-017-10707-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10707-1
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.