Abstracts
Background/Objectives
We aim to describe the clinical and imaging characteristics of young children with dark without pressure- a well-defined area of dark retina in the mid periphery associated with attenuated hyperreflective outer segment bands on spectral domain OCT.
Subjects/Methods
Retrospective medical chart review. We reviewed the charts and retinal images of children with dark without pressure (DWP) seen in the paediatric eye clinic that had undergone retinal imaging.
Results
We identified 6 children (3 males, 3 females) ranging in age from 3 to 13 years with DWP lesions. These were an incidental finding in children referred for other disorders. The lesions spared the macula and were typically in the mid-peripheral retina. In those children who could cooperate with detailed imaging, the DWP lesions were hypoautofluorecent on fundus autofluorescence imaging and OCT imaging showed reduced reflectance of the outer segments and EZ line as has been described in older children and adults. In two of the six subjects a DWP lesion appeared in an area of previously normal fundus; in no subjects did the lesion resolve over the period of follow up.
Conclusions
The clinical and imaging characteristics of DWP lesions are similar in young children to those described in adults. The site of dysfunction appears to be at the level of the outer retina, but the precise cause is unknown. Recognition of this benign disorder will prevent patient anxiety and unnecessary further investigation.
Similar content being viewed by others
Introduction
Dark without pressure fundus lesions are circumscribed retinal areas in the mid periphery which are darker than the surrounding retina and often have a reddish or brown hue. A similar appearance was first described in Jamaican adults and children with sickle cell disease by Condon and Sergeant [1, 2] but the term dark without pressure (DWP) was first coined by Nagpal et al. [3] who published a detailed phenotypic description in a group of African-American patients, the majority of whom had sickle cell disease. In their patients, the lesions were often transient and could disappear without leaving any residual retinal abnormality. The cause of these lesions is uncertain, and no histopathology is available. However, the development of modern retinal imaging, in particular optical coherence tomography (OCT), has allowed a better understanding of the site of the pathology. Fawzi et al. [4] described the results of multi modal imaging in a series of patients with DWP. Their case series was notable for the fact that their patients did not have sickle cell disease and although the majority of cases were African-American the typical lesions were also seen in Caucasian, Hispanic and Asian patients, where they were an incidental finding. The authors highlighted the fact that OCT imaging characteristically demonstrated a reduction in outer segment reflectivity compared with the surrounding retina. It is unclear however whether DWP lesions are congenital or acquired. The majority of reported cases with a well-documented fundus appearance have been in adults and older children. We report here a series of young children who have this characteristic phenotype.
Patients and methods
Six children with a fundus appearance compatible with DWP, seen in the paediatric ophthalmology service at UCSF, in whom it was possible to acquire retinal images, form the basis of this report. The study was approved by the IRB Committee of the University of California San Francisco. Clinical details were collected retrospectively from the electronic patient records and the retinal images reviewed. Colour fundus imaging was performed using scanning laser ophthalmoscopy (Optos 200Tx; Optos Inc, Marlborough, MA), contact fundus photography systems (RETCAM; Clarity Medical System, Inc, Pleasanton, CA or Phoenix Icon; Phoenix Clinical Inc, Pleasanton, CA) and non-mydriatic retinal fundus photography (TRC-NW400; Topcon, Japan). Optical coherence tomography (OCT) imaging was performed either with hand-held spectral domain OCT (Bioptigen Inc., Research Triangle Park, NC) or table top spectral domain OCT (Spectralis; Heidelberg Engineering, Germany) as tolerated by the individual children. Fundus autofluorescence imaging was performed with a scanning laser ophthalmoscope (Optos 200Tx; Optos Inc, Marlborough, MA) or spectral domain OCT (Spectralis; Heidelberg Engineering, Germany).
Results
Six patients, three males and three females, ranged in age from 3 to 13 years of age (Table 1). Four patients had Hispanic background, one patient African-American and one patient was Caucasian. In all cases the DWP lesions were identified as an incidental finding in the clinic or during examination under anaesthesia (EUA) in children referred for another reason. In three patients the DWP lesions were seen in the supero-temporal quadrant and three patients the DWP was nasal to the optic disc. These lesions were present in both eyes in four patients. Two of the lesions were documented as new, after an unremarkable fundus exam and normal fundus photographs in the affected eye a year or more previously. The size of the lesions ranged from 1 DD to 8 DD.
Case reports
Case 1
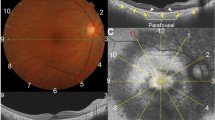
A 2-year old Hispanic girl was referred with a history of sixth nerve palsy and bilateral papilledema in the setting of thrombosis of the right sigmoid sinus. The patient was managed with oral acetazolamide and topiramate, multiple lumbar punctures and subsequently a left optic nerve sheath fenestration for refractory optic nerve swelling was performed. At one-year follow-up, funduscopic examination showed normal disc margins in both eyes. The disc appeared full but not oedematous. The right eye had two flat patches of reddish dark retina with well-defined scalloped edges (2.5 × 1.5 DD; 2 × 1 DD) nasal to the disc (Fig. 1). The left eye had one similar area (1.5 ×0.75 DD) inferonasal to the disc. Otherwise the exam was within normal limits. These lesions had not been noted in previous fundus exams but were apparent on careful review of the RETCAM imaging. Fluorescein angiography revealed a normal choroidal and retinal vascular pattern in each eye with no leakage. Hand held spectral domain OCT revealed a normal vitreoretinal interface and normal retinal and choroidal architecture at the macula. Scans centred on the border of the DWP lesion in the right eye demonstrated normal reflectivity of the ellipsoid zone (inner segment and outer segment junction) outside the lesion, with a discrete transition to hyporeflectivity of the outer retinal bands within the dark patch (Fig. 2a).
a Case 1: hand-held spectral domain OCT revealed discrete transition to hypo reflectivity of the outer retinal bands within the dark fundus patch. The transition points are labelled with orange arrowheads. b Case 2 Infrared reflectance imaging shows reduced reflectance of the DWP lesion. Spectral domain OCT scans across the dark patch demonstrate the transition to hypo reflectivity of the outer retinal bands at the junction between normal retina and DWP (orange arrowhead).
Case 2
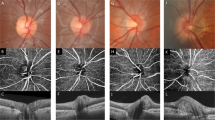
A 13–year old Hispanic male with the diagnosis of high risk-B acute lymphoblastic leukaemia was referred to ophthalmology to rule out papilledema after the finding an opening pressure of 27–30 cm H20 during a lumbar puncture for maintenance chemotherapy. The dilated fundus exam showed normal discs and maculae. The left eye was remarkable for a large (8 × 6 DD) flat dark irregular well-defined patch of retina nasal to the optic disc. Fundus autofluorescence imaging showed reduced autofluorescence within the lesion (Fig. 3). An OCT performed with the Heidelberg Spectralis machine through the dark area showed attenuation of the outer hyper reflective band in the outer retina along the EZ line, that did not change with OCT beam direction change (Fig. 2b). Although imaging of the right eye was initially normal, he later developed extensive DWP in the right eye nasal to the disc (Fig. 4a). A Humphrey 30-2 visual field showed normal retinal sensitivity in each eye including an area of visual field corresponding to the area of DWP.
a Case 2: colour fundus photos right eye, demonstrating normal fundus at baseline imaging (at age 13 years) and DWP lesion nasal to the disc 2 years later. b Case 3 RETCAM Colour fundus images taken a year apart. At age 4 years there was an irregular well-defined dark-reddish flat lesion in the retina nasal to the optic nerve head (right-side); this was not present on images taken 1 year previously (left-side).
Case 3
A 4-year old Hispanic female with a complex medical history including: global developmental delay, congenital or perinatal cytomegalovirus infection, congenital bilateral cataracts, alopecia, ichthyosis and nail dystrophy was referred to ophthalmology for management of bilateral cataracts. Bilateral lensectomies were performed at age 3 months. At age 4 years fundus performed during an EUA revealed two flat patches of darker retina, nasal to the disc (2 × 3DD; and 8 × 6DD) in the left eye. These lesions had not been present at EUA 1 year earlier and were not evident on RETCAM images taken at that time. The optic nerves were small and tilted; the maculae, vessels and peripheral exam were otherwise normal (Fig. 4b). Fluorescein angiography demonstrated normal retinal and choroidal vasculatures within these dark areas. OCT was not performed.
Case 4
A 4-year old African-American boy with autosomal dominant congenital cataract underwent bilateral lensectomies at 9 months of age. He was followed closely for aphakia management. The best corrected visual acuity was hands motion in the right eye and 20/60 (HOTV-Blocked) in the left eye. He had a large right exotropia. Dilated fundus exam was notable for a pale optic disc and pigmentary changes adjacent to the optic nerve head that spared the fovea in both eyes. In the right eye, there was a large dark retinal patch temporal to the fovea, that extended between the arcades. The left eye had a dark flat patch of retina (~3 × 5 DD) along the inferotemporal arcade at the second bifurcation of the inferior vessel arcade. OCT imaging was not possible.
Case 5
A 7-year old Caucasian girl with Marfan syndrome and a history of bilateral lensectomy for lens subluxation was seen in the clinic for follow-up examination. Best corrected visual acuity was 20/25 OD and 20/40 OS (Snellen-Line). Anterior segment exam revealed bilateral aphakia but was otherwise normal. The dilated fundus exam was remarkable for vascular tortuosity in both eyes and a dark retinal patch of irregular well-defined margins area in the upper temporal quadrant of the left eye. It was not possible to obtain OCT images across the DWP lesion.
Case 6
A 9-year old Hispanic male with developmental delay, obesity, high myopia and nystagmus underwent electrophysiological testing and dilated fundus exam under anaesthesia, as part of his work-up. The full-field ERG was abnormal with a reduced amplitude of the scotopic dim (rod specific) b-wave response, a normal amplitude a-wave and severely reduced scotopic b-wave amplitude to the dark-adapted bright flash producing a negative ERG configuration. Cone responses were within normal limits. The electrophysiological responses were consistent with a diagnosis of congenital stationary night blindness. Dilated fundus exam demonstrated a posterior staphyloma and changes consistent with high myopia in each eye but no pigment migration. There were areas of well-defined dark patches in the temporal retina anterior to the equator in each eye and along the superotemporal vascular arcade. The optic nerve heads were tilted with mild pallor. Handheld OCT images across the DWP lesions showed transition to hyporeflectivity of the outer retinal bands across the dark areas.
Discussion
The term DWP was first termed by Nagpal et al. [3] who described flat dark brown patches of retina in 7 African-American subjects, six of whom had sickle cell disease. Their ages ranged from 12 to 56 years. They observed that the lesions appeared to be asymptomatic, transient and could change shape over time. They were observed in the posterior retina or mid periphery in contrast to white without pressure that have a more peripheral location. The authors hypothesized that these changes were caused by subtle changes in the RPE or internal limiting membrane. Similar changes were also described in the longitudinal study of Jamaican adults and children with sickle cell disease [1, 2, 5, 6]. Fawzi et al. [4] later described a series of cases where they were able to perform multimodal retinal imaging. Their subjects ranged in age from 12 to 37 years of age and included subjects who had Hispanic, Asian and Caucasian background as well as African-American. They were also able to demonstrate a normal Goldmann visual field in one subject with a large lesion indicating that there was no significant functional deficit over the lesions. One of our subjects was able to perform static perimetry with the Humphrey perimeter and this showed normal retinal sensitivity over the DWP lesion.
Multimodal imaging in their series showed characteristic findings with the lesions being hypo-autofluorescent on fundus autofluorescence imaging and hyporeflective on near infrared reflectance imaging. We identified similar changes in the patients in our series who had detailed imaging. The most striking findings reported by Fawzi et al. [4] were on OCT imaging which show reduced reflectivity of the photoreceptors and E-Z line over the lesion. There was an abrupt change in reflectivity at the border of the dark patches, which has been confirmed in two further case reports;[7, 8] we were able to demonstrate these findings in those children in our series who could comply with OCT imaging. The underlying anatomical and functional basis for these dark patches is unclear. Nagpal et al. [3] suggested that the DWP lesions were caused by abnormal reflectivity of the internal limiting membrane or retinal pigment epithelium (RPE) and Talbot et al. [6] hypothesized that they may represent sequelae of retinal haemorrhages in children with sickle cell disease. Neither of these explanations are likely given the multimodal imaging findings which show that the site of the abnormality on imaging is in the outer retina. This led Fawzi et al. to suggest that DWP represents islands of abnormal photoreceptor structure; however, this hypothesis does not explain why the lesions can be transient and why they are more common in more darkly pigmented fundi. Adaptive optics imaging of the photoreceptor mosaic within these lesions would be helpful in elucidating the responsible retinal changes but such imaging not yet been reported and will be challenging because of the usual mid peripheral location of the DWP.
Nagpal et al. [3] described the lesions as transient and in two of the six cases in our series the DWP lesions appeared for the first time during a period of regular retinal examinations. We have demonstrated with fundus photography that the new lesions appeared in a previously normal area of retina. In none of our cases did any lesion disappear during follow up exams, but the follow up period is relatively short. It is unclear, from the few cases that have been reported, whether DWP is a congenital abnormality or acquired in later childhood. The transient nature of the lesions and the fact they can appear for the first time in later childhood argue against a congenital abnormality. Talbot et al. [6] in their study of Jamaican children with sickle cell disease found an increasing frequency between the ages of 5 and 10 years suggesting that the appearance may represent a developmental change in the eye rather than a congenital lesion. We have tried to identify DWP lesions in young infants seen in our regular paediatric practice and have not seen any in patients below the age of 2 years and we have not been able to identify any cases in preterm infants who have undergone screening for ROP. Interestingly neither have we seen this fundus appearance in the elderly nor have there been reports of DWP in subjects older than 56 years [3].
DWP lesions of the fundus are benign patches of reddish-brown discoloration of the retina most commonly seen in the mid periphery. They are more common in pigmented fundi and may be transient. They have a characteristic imaging profile with reduced autofluorescence on fundus autofluorescence imaging and localized hyporeflectance of the EZ on OCT. The lesions are likely to be acquired during ocular development rather than congenital. The appearance may cause concern for serious pathology particularly when the DWP patches appear for the first time in a fundus that was previously normal. Recognition of the benign nature of the patches will prevent unnecessary investigation.
Summary
What was known before
-
DWP fundus lesions are circumscribed retinal areas in the mid periphery which are darker than the surrounding retina and often have a reddish or brown hue.
-
They are usually incidental findings.
-
OCT imaging characteristically demonstrated a reduction in outer segment reflectivity compared with the surrounding retina.
What this study adds
-
The clinical and imaging characteristics of DWP lesions are similar in young children to those described in adults.
-
Congenital vs acquired? We present two cases where the lesions were found after a few years of follow up.
References
Condon PI, Sergeant GR. Ocular findings in homozygous sickle cell anemia. Am J Ophthalmol. 1972;73:533–43.
Condon PI, Sergeant GR. Ocular findings in Hemoglobin SC disease in Jamaica. Am J Ophthalmol. 1972;74:921–31.
Nagpal KC, Goldberg MF, Asgourian G, Goldbaum M, Huamonte F. Dark-without -pressure fundus lesions. Br J Ophthalmol. 1975;59:476–9.
Fawzi AA, Nielsen JS, Mateo-Montoya A, Sinjujrungroj T, Li HK, Gonzales J, et al. Multimodal imaging of white without dark lesions. Retina. 2014;34:2376–87.
Talbot JF, Bird AC, Serjeant GR, Hayes RJ. Sickle cell retinopathy in young children in Jamaica. Br J Ophthalmol. 1982;66:149–54.
Talbot JF, Bird AC, Maude GH, Acheson RW, Moriarty BJ, Serjeant GR. Sickle cell retinopathy in Jamaican children: further observations on a cohort study. Br J Ophthalmol. 1988;72:727–32.
Moysidis SN, Koulisis N, Ameri H, Matsunaga D, Yi J, Isozaki VL, et al. Multimodal imaging of geographic areas of retinal darkening. Retin Cases Brief Rep. 2015;9:347–51.
Chen X, Liang M. Changes in dark without pressure. Ophthalmol Retin. 2018;2:1077.
Acknowledgements
Authors would like to acknowledge unrestricted funding support from Research to Prevent Blindness and the NEI core grant (NEI P30-EY002162).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Flores Pimentel, M.A., Duncan, J.L., de Alba Campomanes, A.G. et al. Dark without pressure retinal changes in a paediatric age group. Eye 35, 1221–1227 (2021). https://doi.org/10.1038/s41433-020-1088-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-1088-5