Abstract
Benzodiazepines such as diazepam are widely prescribed as anxiolytics and sleep aids. Continued use of benzodiazepines, however, can lead to addiction in vulnerable individuals. Here, we investigate the neural mechanisms of the behavioral effects of benzodiazepines using the intracranial self-stimulation (ICSS) test, a procedure with which the reward-enhancing effects of these drugs can be measured. Benzodiazepines bind nonselectively to several different GABAA receptor subtypes. To elucidate the α subunit(s) responsible for the reward-enhancing effects of benzodiazepines, we examined mice carrying a histidine-to-arginine point mutation in the α1, α2, or α3 subunit, which renders the targeted subunit nonresponsive to diazepam, other benzodiazepines and zolpidem. In wild-type and α1-point-mutated mice, diazepam caused a dose-dependent reduction in ICSS thresholds (reflecting a reward-enhancing effect) that is comparable to the reduction observed following cocaine administration. This effect was abolished in α2- and α3-point-mutant mice, suggesting that these subunits are necessary for the reward-enhancing action of diazepam. α2 Subunits appear to be particularly important, since diazepam increased ICSS thresholds (reflecting an aversive-like effect) in α2-point-mutant animals. Zolpidem, an α1-preferring benzodiazepine-site agonist, had no reward-enhancing effects in any genotype. Our findings implicate α2 and α3 subunit containing GABAA receptors as key mediators of the reward-related effects of benzodiazepines. This finding has important implications for the development of new medications that retain the therapeutic effects of benzodiazepines but lack abuse liability.
Similar content being viewed by others
INTRODUCTION
Benzodiazepines are widely prescribed to treat anxiety disorders and insomnia. While they are effective in providing symptom relief for these disorders, they are also listed as the second most commonly abused prescription drug group following opioid pain relievers (http://dawninfo.samhsa.gov/). Two types of inappropriate use of these drugs have brought about questions regarding their abuse potential over the years: Continued, long-term use beyond the therapeutic period often at higher doses than prescribed by patients and illicit use, often but not exclusively by polydrug abusers (Griffiths and Weerts, 1997; Malcolm, 2003; Salzman, 1998; Woods et al, 1992; O’Brien, 2005). Both types of misuse depend on the reinforcing effects of benzodiazepines (Griffiths and Weerts, 1997), making it necessary to understand the nature (eg, direct reward, enhancement of drug ‘high’ induced by other drug, relief of anxiety) and mechanisms (eg, receptor subtypes and brain regions involved in each component of the drug reinforcement effect) of benzodiazepine drug reinforcement. Here, we investigate the facilitation of brain-stimulation reward by benzodiazepines and receptor subtypes that are involved in this effect. Benzodiazepines exert their pharmacological effects through positive allosteric modulation of GABAA receptors. GABAA receptors are heteropentameric chloride channels with subunits derived from seven receptor subunit families, many of which exist as multiple isoforms (α1–6, β1–3, γ1–3, δ, ɛ, π, ρ1–3, θ; Olsen and Sieghart, 2008). While the different combinations of these subunits result in diverse receptor composition, benzodiazepines bind relatively unselectively (see below) to a great majority of GABAA receptors, specifically those containing the α1, α2, α3, or α5 subunits, together with a β subunit and a γ subunit.
The benzodiazepine binding site on GABAA receptors is located between the α and γ subunits (Sigel and Buhr, 1997). A specific histidine residue in a conserved position on the α subunits (H101 for α1 and α2; H126 for α3 and H105 for α5) has been shown to be necessary for benzodiazepine binding (Wieland et al, 1992). α4 and α6 subunits, having an arginine residue at this position, are insensitive to benzodiazepines. This knowledge led to the generation of mice carrying histidine-to-arginine point mutations in the normally benzodiazepine-sensitive α subunits, rendering the receptors containing the respective subunits insensitive to benzodiazepines (ie, α1(H101R), α2(H101R), α3(H126R), and α5(H105R) mice). Studies using these point-mutant mice revealed that different actions of benzodiazepines, such as anxiolysis, sedation, and amnestic effects, are pharmacologically separable and can be functionally linked to specific α subunits (Crestani et al, 2001, 2002; Low et al, 2000; Rudolph et al, 1999). These findings stimulated interest in the development of subunit-specific compounds. While no drug has been convincingly shown to be truly subunit-specific for any GABAA receptor subunit in vivo, reports involving the use of subunit-preferring compounds (Dias et al, 2005; McKernan et al, 2000) have supported the idea that the undesirable effects of benzodiazepines (eg, sedation) can be managed by the use of compounds specific to the subunit that is involved in a certain symptom (eg, α2- and/or α3-subunit-selective agonists for anxiety).
Despite the above-noted high prevalence of benzodiazepine misuse and abuse, little is known about the mechanisms by which benzodiazepines modulate reward-related processes and by which they become addictive (Tan et al, 2011). Several studies have shown that benzodiazepines have reward-enhancing effects in the intracranial self-stimulation (ICSS) test (Carden and Coons, 1990; Cauderella et al, 1982, 1984; Gomita et al, 2003; Olds, 1976; Straub et al, 2010). The GABAA receptor subunits that mediate these reward-enhancing properties, however, have not been elucidated. Two recent studies (Heikkinen et al, 2009; Tan et al, 2010) suggest that the α1-containing GABAA receptors (α1-GABAA-Rs) in the VTA may be responsible for the addictive properties of benzodiazepines. While the electrophysiological evidence makes a convincing case for the role of α1 subunits in the ability of benzodiazepines to induce addiction-like synaptic plasticity in the VTA, there is limited evidence for the translation of these synaptic modulations into behavioral changes, especially in cases where a motivational component is involved, as in the case of ICSS. Moreover, GABAA receptors containing other subunits are abundant in different parts of the mesolimbic dopamine system, suggesting that there may be more than one GABAA receptor subtype mediating the rewarding properties of benzodiazepines.
The goal of this study was to investigate the broad role of α1-, α2-, and α3-GABAA-Rs in the mediation of the reward-enhancing effects of benzodiazepines in the ICSS test, using systemic administration of representative drugs of this class. As mentioned above, to date no drug has been shown to be absolutely specific to any GABAA receptor subtype in vivo. On the other hand, the histidine-to-arginine point-mutated mice provide an elegant model to investigate the subunit(s) crucial for the development of a certain benzodiazepine effect. Thus, we have utilized wild-type, α1(H101R), α2(H101R), and α3(H126R) mice to investigate the role of each of these subunits in the effects of the nonselective benzodiazepine-site agonist diazepam and the α1-preferring drug zolpidem in an ICSS paradigm. For comparison, the effect of cocaine was also examined in each genotype, to determine if any of the mutations produce generalized reductions in sensitivity to rewarding stimuli.
MATERIALS AND METHODS
Subjects
Eighty-five male mutant (Rudolph et al, 1999; Low et al, 2000) and wild-type mice (between 4 and 7 months of age at the time of surgery) and maintained on a C57BL/6J background were used in this experiment. The mice were bred at McLean Hospital, housed individually with free access to food and water, and maintained on a 12-h light (lights on at 0600 hours) dark cycle during the experiment. Training and testing occurred during the light phase at the same time each day. All procedures were conducted in accordance with the NIH guide for the Care and Use of Laboratory animals, and were approved by the McLean Hospital Institutional Animal Care and Use Committee.
Surgery
All procedures have been described previously in detail (Carlezon and Chartoff, 2007). Mice were anesthetized with intraperitoneal (IP) injections of a ketamine (139 mg/kg) plus xylazine (21 mg/kg) mixture (Sigma-Aldrich, St Louis, MO). Monopolar electrodes (0.250-mm diameter; Plastics One, Roanoke, VA) were implanted in the right medial forebrain bundle (MFB) at the level of the lateral hypothalamus (−1.9 mm AP, ±0.8 mm ML, −4.8 mm DV from bregma). Electrodes were coated with polyimide insulation except at the flattened tip, and the anode was a noninsulated stainless steel wire (0.125-mm diameter) wrapped around a stainless steel screw threaded into the skull. The electrode and screw assembly were secured to the skull with dental cement.
The use of monopolar electrodes was preferred over the more conventional bipolar electrodes due to their smaller size in order to minimize damage to brain tissue. While the use of monopolar electrodes leads to a greater spread of current (Potegal et al, 1980; Valenstein and Beer, 1961; Stark et al, 1962), with the stimulation parameters employed in the current experiments, the spread is expected to be limited; for example, <0.5 mm (Potegal et al, 1980; Wise, 1972). Thus, the cathodal current delivered through the monopolar electrodes with the stimulation intensities used in the current experiments is expected to provide relatively precise stimulation of the tracts passing through the MFB.
ICSS Training
After 2 weeks of recovery, mice were trained on a fixed-ratio schedule (FR1) to respond for brain stimulation. Each operant conditioning chamber (Med Associates, St Albans, VT) was equipped with a 2 cm × 5 cm wheel manipulandum. Each quarter turn of the wheel earned a 0.5-s train of square-wave cathodal pulses (0.1 ms pulse duration) at a set frequency of 158 Hz. During the first phase of training consisting of daily 60 min training sessions, the stimulation current (52–135 μA) of each mouse was adjusted to a value that would sustain a reliable rate of responding (48–72 spins per min) for 3 consecutive days. After the mice were assessed to be performing stably at their individual current, each mouse was adapted to brief tests with each of a descending series of 15 stimulation frequencies, beginning with the training frequency of 158 Hz. Each series (or rate–frequency ‘curve’) comprised 1-min test trials at each frequency. For each frequency, there was a 5-s ‘priming’ phase during which noncontingent stimulation was given, a 50-s test phase during which the number of responses was counted, and a 5-s time-out period during which no stimulation was available. The stimulation frequency was then lowered by 10% (0.05 log units), and another trial was started. After responding had been evaluated at each of the 15 frequencies, the procedure was repeated such that each mouse was given six such series per day (90 min of training). During the training procedure, the current was adjusted for each mouse so that the highest 5–7 frequencies would sustain responding. To quantify ICSS thresholds (the frequency at which the stimulation becomes rewarding), a least-squares line of best fit was plotted across the frequencies that sustained responding at 20, 30, 40, 50, and 60% of the maximum rate. Reward threshold was defined as the frequency at which the line intersected the x axis (Theta 0; see Carlezon and Chartoff, 2007). In addition to meeting initial training criteria, mice that were assessed to have no greater than 20% variation in mean thresholds for 3 consecutive days or were trained for a minimum of 20 days were started with drug testing. Of the 85 mice that began training after ICSS surgery, 48 mice (WT n=12, α1(H101R) n=12, α2(H101R) n=12, and α3(H126R) n=12) were used in drug testing, while the remaining mice were eliminated due to the headcap assembly getting loose during the training period, or due to problems possibly resulting from misplaced electrodes, such as seizure-like responses or motor-artifacts following stimulation, failing to meet training criteria (ie, spinning response not acquired or the baseline not stabilizing) etc.
ICSS Testing
On each testing day, three rate–frequency curves were determined for each mouse immediately before drug treatment. The first curve served as a warm-up period; the second and third curves were averaged to obtain the baseline (threshold and maximum response rate) parameters. Each mouse then received an IP injection of drug or vehicle, and three more 15-min rate–frequency curves were obtained that were averaged for analysis of drug effects. Mice first received diazepam (1, 2, or 4 mg/kg), then zolpidem (0.3, 1, or 3 mg/kg) and finally cocaine (10 mg/kg); doses were given in ascending and then descending order for each drug, so that mice received every drug dose twice; vehicle doses were given between all drug days as well as at the first and last day of each drug test (see Figure 1 for a summary of the experimental schedule). This drug regimen was designed to reduce the likelihood of any effects of sensitization or tolerance seen from repeated drug doses. There were no significant differences between the first and second treatment at any dose, indicating that there was no measurable development of tolerance or sensitization; therefore, the data for each dose were combined into single means.
Experimental schedule.
Drugs
Diazepam (Biomol, Plymouth Mtg., PA) and zolpidem (Tocris Bioscience, Minneapolis, MN) were dissolved in 10% (2-Hydroxypropyl)-β-cyclodextrin (Sigma-Aldrich). Cocaine HCl (Sigma-Aldrich) was dissolved in 0.9% saline. Drugs and vehicle solutions were administered IP injection at a volume of 10 ml/kg.
Histology
At the end of the experiments, mice were deeply anesthetized with sodium pentobarbital (200 mg/kg, IP) and perfused with 4% paraformaldehyde containing 15% picric acid. The fixed brains were removed, frozen, and sliced in 40 μm sections for cresyl violet staining.
Data Analysis
Threshold and maximal response rate data were each analyzed using a two-way analysis of variance (ANOVA) with repeated measures, followed by post hoc Dunnett test with the vehicle groups in each genotype as the comparison group for pairwise comparisons.
RESULTS
Histology
The approximate locations for the tip of the stimulation electrodes, as well as a representative slice showing a cresyl violet stained section from an experimental mouse can be seen in Figure 2. All mice included in drug testing had electrodes correctly targeting the MFB.
Histology. (a) Atlas plates showing the electrode tip targets (Paxinos and Franklin, 2001) and (b) a representative brain slice showing the electrode tract and target region. All animals that were included in the experiments had correctly placed electrodes.
The Effects of Diazepam on ICSS Reward Threshold and Maximum Response
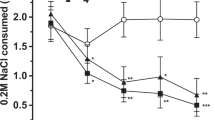
A two-way ANOVA on reward thresholds using diazepam treatment dose and genotype as the independent variables revealed a significant main effect of diazepam treatment (F(3, 190)=4.35, p<0.01) and of genotype (F(3, 190)=15.21, p<0.01), in addition to a significant treatment × genotype interaction (F(9, 190)=2.98, p<0.01). In wild-type animals, diazepam reduced reward threshold at all three doses administered (Dunnett post hoc test; p<0.05 for 1 mg/kg, p<0.01 for 2 and 4 mg/kg), indicating a reward-enhancing effect (Figure 3a). The reward-enhancing effect of diazepam was dampened in α1(H101R) animals and was significant at only the lowest, 1 mg/kg dose (Dunnett post hoc test; p<0.05) despite the fact that a nonsignificant trend towards reduction was also observed at other doses (see Figure 3a). This effect was completely abolished in α2(H101R) and α3(H126R) mice. In fact, 4 mg/kg diazepam significantly increased reward thresholds in α2(H101R) mice (Dunnett post hoc test; p<0.05).
Diazepam effects on ICSS behavior. (a) Rate–frequency functions plotted for each genotype show a left-shift at all doses of diazepam for wild-type mice and at 1 mg/kg for α1(H101R) mice, while no comparable left-shifts are observed in α2(H101R) and α3(H101R) mice. A right-shift is observed in α2(H101R) mice following a 4 mg/kg dose of diazepam. (b) Reward thresholds expressed as percentage baseline threshold were significantly reduced following diazepam treatment in wild-type (WT) and α1(H101R) mice, while this effect was abolished in α2(H101R) and α3(H126R) mice. The 4 mg/kg dose of diazepam caused an increase in reward threshold for α2(H101R) mice. (c) Maximum response (expressed as percentage baseline maximum response) was increased by 2 and 4 mg/kg diazepam in WT mice. While there were no other significant changes in maximum response rates, all genotypes showed the same initial-increase-then-decline pattern with increasing doses of diazepam. *p<0.05, **p<0.01.
Two-way ANOVA on maximum response rates revealed a main effect of drug treatment (F(3,190)=4.27, p<0.01; Figure 3b). Further analyses revealed that the maximum response rates were increased in wild-type mice receiving 2 or 4 mg/kg diazepam (Dunnett post hoc test; p<0.05 for both doses).
The Effects of Zolpidem on ICSS Reward Threshold and Maximum Response
A two-way ANOVA on reward thresholds revealed a significant main effect of zolpidem treatment (F(3, 190)=8.77, p<0.01) and of genotype (F(3, 190)=10.65, p<0.01; Figure 4a). The zolpidem treatment × genotype interaction effect was not statistically significant. Further analyses of the genotype main effect showed that the α1(H101R) animals were significantly different than the wild-type control mice regardless of the drug treatment (Dunnett post hoc test; p<0.05). The 3 mg/kg dose of zolpidem caused a significant increase in reward threshold in wild-type (p<0.01), α2(H101R) (p<0.05), and α3(H126R) (p<0.01) mice. No effect on reward threshold was observed in α1(H101R) animals.
Zolpidem effects on ICSS behavior. (a) Rate–frequency functions plotted for each genotype reveal rightward shifts in all genotypes except α1(H101R) following zolpidem administration. (b) No reduction in reward thresholds were observed following zolpidem treatment when the reward threshold were expressed as percentage baseline threshold; 3 mg/kg dose of zolpidem caused an increase in reward threshold in WT, α2(H101R), and α3(H126R) animals, possibly due to sedation. (c) Maximum response (expressed as percentage baseline maximum response) was reduced following 3 mg/kg dose of zolpidem WT and α3(H126R) animals. *p<0.05, **p<0.01.
The analysis of maximum response revealed a significant genotype main effect (F(3, 190)=3.31, p<0.05), a significant zolpidem treatment main effect (F(3, 190)=8.98, p<0.01) and a significant interaction effect (F(9, 190)=2.86, p<0.01; Figure 4b). In further analyses, we found that zolpidem (3 mg/kg) reduced maximum responding in wild-type and α3(H126R) mice (Dunnett post hoc test; p<0.01 for both). The lowest dose of zolpidem also caused a slight increase in maximum response only in α2(H101R) mice (p<0.05). No effects on maximum response were observed in α1(H101R) animals.
The Effects of Cocaine on ICSS Reward Threshold and Maximum Response
As expected, the analysis of the cocaine reward threshold data revealed only a significant main effect of cocaine treatment (F(1, 98)=54.91, p<0.01), with no effect of genotype or of the interaction of the two variables (Figure 5a). Cocaine administration reduced reward threshold in all genotypes (p<0.01 for wild-type, α1(H101R) and α3(H126R) mice; p<0.05 for α2(H101R) mice).
Cocaine effects on ICSS behavior. (a) Rate–frequency functions plotted for each genotype reveal a left-shift following cocaine administration in all genotypes. (b) Cocaine treatment caused a decrease in reward threshold (expressed as percentage baseline threshold) in all genotypes. (c) A trend for an increase in maximum response (expressed as percentage baseline maximum response) was observed for all genotypes but was significant only in α3(H126R) animals. *p<0.05, **p<0.01.
A significant cocaine treatment main effect was also observed in maximum response (F(1, 98)=18.23, p<0.01; Figure 5b)). Cocaine treatment caused a slight increase in maximum responding in all genotypes, but this effect was statistically significant only in α3(H126R) (p<0.01) animals.
DISCUSSION
In this study, we report that the benzodiazepine diazepam dose dependently reduces ICSS reward thresholds in wild-type C57Bl/6J mice, confirming and extending earlier findings regarding the effects of this benzodiazepine on brain stimulation reward thresholds (Straub et al, 2010). More importantly, we report that the reduction in reward thresholds relies on the functional binding of diazepam to and the positive modulation of GABAA receptors containing α2 and/or α3 subunits, as this effect is abolished in α2(H101R) and α3(H126R) mice. The treatment of the α2(H101R) mice with 4 mg/kg diazepam even led to an increase in reward thresholds, suggesting that at this dose, diazepam might be aversive for these animals, further establishing the importance of α2-GABAA-Rs for the rewarding effects of benzodiazepines. Diazepam did not cause an obvious level of sedation at the doses employed, as evidenced by the maximum response rates following diazepam treatment, which are either higher or at the same level as the maximum response following vehicle treatment.
Diazepam treatment still led to a decrease of the reward threshold in α1(H101R) mice, suggesting that the positive modulation of α1-GABAA-Rs is not required for the reward-enhancing effects of this drug as measured by ICSS. However, the reduction in reward thresholds in α1(H101R) mice was dampened compared with wild-type mice. These findings raise the possibility that the α1-GABAA-R's may be partially involved in the threshold-reducing effects of diazepam. Based on this finding and earlier studies, suggesting the importance of α1-GABAA-R's in the addictive properties of benzodiazepines (Heikkinen et al, 2009; Tan et al, 2010), we performed an ICSS test with three different doses of zolpidem, an α1-preferring benzodiazepine. Zolpidem did not reduce reward thresholds in wild-type or point-mutant mice, further confirming that drug actions at the α1 subunit are not sufficient for the reduction of ICSS reward thresholds. The highest dose of zolpidem (3 mg/kg) caused sedation in wild-type, α2(H101R) and α3(H126R) mice, as evidenced by the reduction in maximum response rates. At this dose, zolpidem also led to an increase in reward thresholds; this effect may be an artifact of decreased responding due to sedation rather than an aversive effect, although the metric we use to quantify alterations in thresholds (Theta 0) is designed specifically to minimize this type of confound (see Carlezon and Chartoff, 2007). This increase in reward thresholds accompanied by a decrease in maximum responding stands in contrast with the increase in reward thresholds observed in α2(H101R) mice following treatment with 4 mg/kg diazepam, which appears completely unrelated to sedation (ie, 4 mg/kg diazepam did not reduce maximum response in α2(H101R) mice). Elevations in ICSS thresholds may reflect anhedonia (reduced sensitivity to reward) or aversion (Carlezon and Chartoff, 2007); additional studies such as place conditioning are needed to distinguish these two possibilities. Finally, as expected, zolpidem treatment did not cause sedation in α1(H101R) mice, as the α1 subunit is responsible for the sedative effects of benzodiazepines and zolpidem (Crestani et al, 2000; Rudolph et al, 1999).
The fact that the ICSS paradigm provides a measure of ‘reward-facilitation’ rather than a direct measure of reward should be taken into account while interpreting the findings. The finding that the administration of diazepam reduces reward thresholds means that the effects of diazepam add to the rewarding effects of the brain stimulation, making lower amounts of stimulation more effective. However, technically, the effectiveness of a certain stimulation frequency in maintaining the response may increase or decrease due to factors unrelated to changes in the activity of the brain reward system, such as nonspecific motor effects. The choice of the theta 0 (T0) reward threshold measure (as opposed to half-maximum, for instance) assures that the data interpretation is minimally affected by possible changes in motor capabilities (see Figure 2c in Carlezon and Chartoff, 2007). Thus, the reported changes in ICSS reward thresholds are likely to be a result of the manipulation of the brain reward system by the administered drugs rather than their effects on motor facility. A second possible interpretation of the results is that the mutant animals have nonspecific dysfunctions in the brain reward system that do not relate to the effects of diazepam. However, the above-noted abolishment of reward-enhancing effects in α2(H101R) and α3(H101R) animals is unlikely to be due to a generalized dysfunction in the reward system of the point-mutant animals, as evidenced by two pieces of data: First, the vehicle-treated animals of all genotypes showed comparable baseline responding under all drugs, suggesting that the mutations are silent under drug-free conditions. Second, our ICSS test with cocaine as a positive control shows that a drug with a mechanism of action not involving the GABAA receptors can still lead to the same level of reward enhancement in all animals.
Our findings stand in an apparent contrast to the results of earlier studies that suggested that the positive manipulation of α1-containing GABAA-Rs may be vital for the addictive-like profile of benzodiazepines at the electrophysiological level (Heikkinen et al, 2009; Tan et al, 2010). Moreover, Tan et al (2010) reported that α1(H101R) mice, unlike wild-type mice, do not prefer a sucrose solution that contains the benzodiazepine midazolam over a sucrose-only solution, indicating that the rewarding effects of this benzodiazepine rely on α1-GABAA-Rs also at the behavioral level. Their findings are in line with earlier studies showing that zolpidem, an α1-preferring drug, is self-administered by baboons (Griffiths et al, 1992), at rates equal to or higher than several benzodiazepines (Griffiths et al, 1981, 1991). Other reports, however, have noted that the positive modulation of α1-GABAA-Rs may be sufficient, but not necessary, for the reinforcing effects of benzodiazepines (Rowlett et al, 2005).
The discrepancy between our findings and earlier reports may be due to a number of factors. First, the time course followed in our behavioral studies and that in the electrophysiological studies is different and it is possible that the neuronal mechanisms mediating benzodiazepine reward at these two different time points are distinct. It is possible that the activity of the α1-GABAA-Rs is required for the long-lasting neuronal changes that underlie addiction as investigated in the electrophysiology studies, while the immediate reinforcing effect following injection is dependent on other subunits, namely α2 and α3. Second, as the electrophysiology studies do not depend on motor responses and as the measurements were taken only 24 h following treatment, the authors of these studies were able to employ significantly higher doses of zolpidem than in the current study. The possibility remains that different subunits might mediate the reward-related effects of benzodiazepines at different receptor occupancies, where the α1 subunits may become more important at high receptor occupancies.
In addition to the above-noted technical differences between earlier studies and the current study, there are a number of conceptual differences, suggesting that the studies may be investigating different phenomena with possibly different underlying brain circuitry. The ICSS paradigm used in our study investigates the facilitation of brain stimulation reinforcement by drugs, as opposed to the rewarding effects of the drug per se. Drugs of abuse supplement and enhance the performance to receive this stimulation reinforcement. It is possible that the rewarding effects of a drug given under baseline conditions and under self-stimulation reinforcement conditions tap into different brain circuitry, considering that MFB self-stimulation in and of itself causes neuronal changes in the dopaminergic neurons of the VTA (Pillolla et al, 2007). It is generally agreed upon that ICSS in the MFB stimulates the descending fibers, which transynaptically activate the DA neurons in the VTA (Bielajew and Shizgal, 1986). However, the exact substrate activated by ICSS is not clear. There have been reports that the activation of cholinergic neurons in nearby tegmental areas or the descending glutamatergic fibers (Yeomans et al, 1993; 2000; You et al, 2001) may be important. The GABAergic system may be involved in the modulation of this complex system; however, a study of the exact anatomical substrates and cell populations where different GABAA receptor subtypes modulate this system is beyond the scope of this report.
Second, the midazolam drinking paradigm employed by Tan et al (2010) requires very little directed action on the part of the animal (ie, drinking from one liquid bottle vs another), while the ICSS paradigm requires an active operant response (ie, spinning of a wheel). Goal-directed behaviors, such as the spinning of a wheel to retrieve a reward, involve excitatory projections from the prefrontal cortex, the subiculum and the basolateral amygdala to the NAcc (Sesack and Grace, 2010), while simple ‘liking’ of a rewarding stimulus, such as a solution that contains midazolam, can be controlled by a small ‘hedonic hotspot’ within the medial region of the NAcc shell (Pecina and Berridge, 2005). Indeed, there is strong evidence showing that the neuronal circuitry underlying different components of reward, such as ‘liking’ (ie, experience of simple pleasure through the administration of an appetitive stimulus), ‘wanting’ (ie, incentive salience that leads to motivated behavior) and learning (ie, the acquisition of the associations between reward-predictive cues and the natural reward) is distinct (Berridge et al, 2009). The areas that are implicated in goal-directed behaviors, such as the prefrontal cortex, the subiculum and the basolateral amygdala, as well as the NAcc itself, have a high density of α2-GABAA-Rs, while the VTA contains predominantly α1-GABAA-Rs in the interneurons (Dixon et al, 2010; Fritschy and Mohler, 1995; Pirker et al, 2000; Tan et al, 2010). Thus, it is possible that the prefrontal, subicular, and amygdalar excitatory inputs into the NAcc, as well as NAcc output to downstream structures, may be controlled by α2-GABAA-Rs, while the dopaminergic inputs from VTA onto NAcc may be controlled by α1-GABAA-Rs, resulting in a dissociation between the motivational (ie, wanting) and appetitive (ie, liking) components of reward. A recent study provides some initial evidence for the view that the α2-containing GABAA-Rs of the NAcc play a pivotal role in the incentive effects of drugs of abuse by modulating the activity of medium spiny neurons (Dixon et al, 2010), supporting a role for these receptors in certain incentive motivational processes as well.
The specific dopaminergic disinhibition mechanism through the activation of the α1-GABAA-Rs located in the somata of VTA GABAergic neurons has been well explained by Tan et al (2010). It is, however, more challenging to explain the involvement of α2 and α3 subunits in reward, as there is evidence from RT–PCR, suggesting that these subunits are expressed on the dopaminergic neurons within VTA (Okada et al, 2004), although the results from immunohistochemical studies provide conflicting results on whether the α2 subunit is expressed in the VTA (Fritschy and Mohler, 1995, S Pirker et al, 2000), potentially indicating that if the α2 subunit is expressed in the VTA, it may be at very low levels. This would suggest that the activation of the α2- and α3-GABAA-Rs in the VTA would inhibit dopaminergic projections from VTA to the NAcc, the opposite of a rewarding effect. Thus, it is likely that the activation of α2- and α3-containing GABAA-Rs in other parts of the reward circuitry is important for the reward-enhancing effects of diazepam in ICSS, similar to the findings by Dixon et al (2010) showing that the NAcc α2-containing GABAA-Rs are required for certain drug effects of cocaine.
Our findings indicate that the reward-enhancing effect of benzodiazepines is mediated by α2- and possibly α3-GABAA-Rs. We have found no evidence that the α1-GABAA-Rs are required for this effect. The data we present provide important evidence that the α2- and α3-GABAA-Rs may mediate some of the reward-related properties of benzodiazepines, at least when (1) the individual is already in a high-reward state and (2) when there is a motivational component involved. Self-administration and oral consumption studies, on the other hand, have pointed out an important role for α1-containing GABAA-Rs in maintaining self-administration (Griffiths et al, 1992; Tan et al, 2010). The findings have some correspondence with the human literature, where drug-experienced subjects report ‘liking’ different benzodiazepines, as well as zolpidem (Roache and Griffiths, 1987; Evans et al, 1990). The reports are far from consistent, however, and some findings indicate that zolpidem might even have aversive effects in drug-inexperienced subjects (Licata et al, 2008, 2011; Rush and Griffiths, 1996; Rush et al, 1998). It is unclear how reward threshold measures in ICSS, self-administration studies in animals and even self-report measures by humans exactly reflect onto the abuse and misuse potential of any compound. The widespread misuse and abuse of benzodiazepines, however, remains a reality, and it is clear that each of the above-noted measures represent certain components of reward and motivation processes that play a role in misuse and abuse. Further studies are necessary in order to understand the exact behavioral outcomes that engage different GABAA receptor subtypes, as well as in order to elucidate the exact anatomical circuitry underlying these behavioral effects.
References
Berridge KC, Robinson TE, Aldridge JW (2009). Dissecting components of reward: ‘liking’, ‘wanting’, and learning. Curr Opin Pharmacol 9: 65–73.
Bielajew C, Shizgal P (1986). Evidence implicating descending fibers in self stimulation of the medial forebrain bundle. J Neurosci 6: 919–929.
Carden SE, Coons EE (1990). Diazepam's impact on self-stimulation but not stimulation-escape suggests hedonic modulation. Behav Neurosci 104: 56–61.
Carlezon Jr WA, Chartoff EH (2007). Intracranial self-stimulation (ICSS) in rodents to study the neurobiology of motivation. Nat Prot 2: 2987–2995.
Cauderella M, Campbell KA, Milgram NW (1982). Differential effects of diazepam (valium) on brain stimulation reward sites. Pharmacol Biochem Behav 16: 17–21.
Cauderella M, Destrade C, Cazala P, Gauthier M (1984). Dissociation of limbic structures by pharmacological effects of diazepam on electrical self-stimulation in the mouse. Brain Res 302: 196–200.
Crestani F, Keist R, Fritschy JM, Benke D, Vogt K, Prut L et al (2002). Trace fear conditioning involves hippocampal alpha5 GABA(A) receptors. Proc Natl Acad Sci USA 99: 8980–8985.
Crestani F, Martin JR, Mohler H, Rudolph U (2000). Mechanism of action of the hypnotic zolpidem in vivo. Brit J Pharmacol 131: 1251–1254.
Crestani F, Mohler H, Rudolph U (2001). Anxiolytic-like action of diazepam: mediated by GABAA receptors containing the alpha2 subunit. Trends Pharmacol Sci 22: 403–406.
Dias R, Sheppard WF, Fradley RL, Garrett EM, Stanley JL, Tye SJ et al (2005). Evidence for a significant role of alpha 3-containing GABAA receptors in mediating the anxiolytic effects of benzodiazepines. J Neurosci 25: 10682–10688.
Dixon CI, Morris HV, Breen G, Desrivieres S, Juqurnauth S, Steiner RC et al (2010). Cocaine effects on mouse incentive-learning and human addiction are linked to alpha 2 subunit-containing GABA(A) receptors. PNAS 107: 2289–2294.
Evans SM, Funderbunk FR, Griffiths RR (1990). Zolpidem and triazolam in humans: behavioral and subjective effects and abuse liability. J Pharmacol Exp Ther 255: 1246–1255.
Fritschy JM, Mohler H (1995). GABAA-receptor heterogeneity in the adult rat brain: differential regional and cellular distribution of seven major subunits. J Comp Neurol 359: 154–194.
Gomita Y, Ichimaru Y, Moriyama M, Araki H, Futagami K (2003). Effects of anxiolytic drugs on rewarding and aversive behaviors induced by intracranial stimulation. Acta Med Okayama 57: 95–108.
Griffiths RR, Lamb RJ, Sannerud CA, Ator NA, Brady JV (1991). Self-injection of barbiturates, benzodiazepines and other sedative-anxiolytics in baboons. Psychopharmacology 103: 154–161.
Griffiths RR, Lukas SE, Bradford LD, Brady JV, Snell JV (1981). Self-injection of barbiturates and benzodiazepines in baboons. Psychopharmacology 75: 101–109.
Griffiths RR, Sannerud CA, Ator NA, Brady JV (1992). Zolpidem behavioral pharmacology in baboons–self-injection, discrimination, tolerance and withdrawal. J Pharmacol Exp Ther 260: 1199–1208.
Griffiths RR, Weerts EM (1997). Benzodiazepine self-administration in humans and laboratory animals -- implications for problems of long-term use and abuse. Psychopharmacology 134: 1–37.
Heikkinen AE, Moykkynen TP, Korpi ER (2009). Long-lasting modulation of glutamatergic transmission in VTA dopamine neurons after a single dose of benzodiazepine agonists. Neuropsychopharmacology 34: 290–298.
Licata SC, Mashhoon Y, Maclean RR, Lukas SE (2011). Modest abuse-related subjective effects of zolpidem in drug-naive volunteers. Behav Pharmacol 22: 160–166.
Licata SC, Penetar DM, Dunlap S, Lukas SE (2008). A therapeutic dose of zolpidem has limited abuse-like effects in drug-naive females: a pilot study. Eur J Pharmacol 598: 64–67.
Low K, Crestani F, Keist R, Benke D, Brunig I, Benson JA et al (2000). Molecular and neuronal substrate for the selective attenuation of anxiety. Science 290: 131–134.
Malcolm RJ (2003). GABA systems, benzodiazepines, and substance dependence. J Clin Psychiatry 64: 36–40.
McKernan RM, Rosahl TW, Reynolds DS, Sur C, Wafford KA, Atack JR et al (2000). Sedative but not anxiolytic properties of benzodiazepines are mediated by the GABA(A) receptor alpha1 subtype. Nat Neurosci 3: 587–592.
O’Brien CP (2005). Benzodiazepine use, abuse, and dependence. J Clin Psychiat 66: S28–S33.
Okada H, Matsushita N, Kobayashi K, Kobayashi K (2004). Identification of GABAA receptor subunit variants in midbrain dopaminergic neurons. J Neurochem 89: 7–14.
Olds J (1976). Brain stimulation and the motivation of behavior. Prog Brain Res 45: 401–426.
Olsen RW, Sieghart W (2008). International Union of Pharmacology. LXX. Subtypes of gamma-aminobutyric acid(A) receptors: classification on the basis of subunit composition, pharmacology, and function. Update. Pharmacol Rev 60: 243–260.
Paxinos G, Franklin KBJ (2001). The mouse brain in stereotaxic coordinates, 2nd edn Academic press: San Diego, CA.
Pecina S, Berridge KC (2005). Hedonic hot spot in nucleus accumbens shell: where do mu-opioids cause increased hedonic impact of sweetness? J Neurosci 25: 11777–11786.
Pillolla G, Melis M, Perra S, Muntoni AL, Gessa GL, Pistis M (2007). Medial forebrain bundle stimulation evokes endocannabinoid-mediated modulation of ventral tegmental area dopamine neuron firing in vivo. Psychopharmacology 191: 843–853.
Pirker S, Schwarzer C, Wieselthaler A, Sieghart W, Sperk G (2000). GABA(A) receptors: immunocytochemical distribution of 13 subunits in the adult rat brain. Neuroscience 101: 815–850.
Potegal M, Blau A, Miller S (1980). Preliminary observations with a technique for measuring current spread in the rat brain. Physiol Behav 25: 769–773.
Roache JD, Griffiths RR (1987). Lorazepam and meprobamate dose effects in humans: behavioral effects and abuse liability. J Pharmacol Exp Ther 243: 978–988.
Rowlett JK, Platt DM, Lelas S, Atack JR, Dawson GR (2005). Different GABA(A) receptor subtypes mediate the anxiolytic, abuse-related, and motor effects of benzodiazepine-like drugs in promates. Proc Natl Acad Sci USA 102: 915–920.
Rudolph U, Crestani F, Benke D, Brunig I, Benson JA, Fritschy JM et al (1999). Benzodiazepine actions mediated by specific γ-aminobutyric acidA receptor subtypes. Nature 401: 796–800.
Rush CR, Armstrong DL, Ali JA, Pazzaglia PJ (1998). Benzodiazepine-receptor ligands in humans: acute performance-impairing, subject-rated and observer-rated effects. J Clin Psychopharmacol 18: 154–165.
Rush CR, Griffiths RR (1996). Zolpidem, triazolam, and temazepam: behavioral and subject-rated effects in normal volunteers. J Clin Psychopharmacol 16: 146–157.
Salzman C (1998). Addiction to benzodiazepines. Psychiatr Q 69: 251–261.
Sesack SR, Grace AA (2010). Cortico-Basal Ganglia reward network: microcircuitry. Neuropsychopharmacology 35: 27–47.
Sigel E, Buhr A (1997). The benzodiazepine binding site of GABAA receptors. Trends Pharmacol Sci 18: 425–429.
Stark P, Fazio G, Boyd ES (1962). Monopolar and bipolar stimulation of the brain. Am J Physiol 203: 371–373.
Straub CJ, Carlezon Jr WA, Rudolph U (2010). Diazepam and cocaine potentiate brain stimulation reward in C57BL/6J mice. Behav Brain Res 206: 17–20.
Tan KR, Brown M, Labouebe G, Yvon C, Creton C, Fritschy JM et al (2010). Neural bases for addictive properties of benzodiazepines. Nature 463: 769–774.
Tan KR, Rudolph U, Luscher C (2011). Hooked on benzodiazepines: GABAA receptor subtypes and addiction. Trends Neurosci 34: 188–197.
Valenstein ES, Beer B (1961). Unipolar and bipolar electrodes in self-stimulation experiments. Am J Physiol 201: 1181–1186.
Wieland HA, Luddens H, Seeburg PH (1992). A single histidine in GABAA receptors is essential for benzodiazepine agonist binding. J Biol Chem 267: 1426–1429.
Wise RA (1972). Spread of current from monopolar stimulation of the lateral hypothalamus. Amer J Physiol 223: 545–548.
Woods JH, Katz JL, Winger G (1992). Benzodiazepines: use, abuse, and consequences. Pharmacol Rev 44: 151–347.
Yeomans JS, Mathur A, Tampakeras M (1993). Rewarding brain stimulation: role of tegmental cholinergic neurons that activate dopamine neurons. Behav Neurosci 107: 1077–1087.
Yeomans JS, Takeuchi J, Baptista M, Flynn DD, Lepik K, Nobrega J et al (2000). Brain-stimulation reward thresholds raised by an antisense oligonucleotide for the M5 muscarinic receptor infused near dopamine cells. J Neurosci 20: 8861–8867.
You ZB, Chen YQ, Wise RA (2001). Dopamine and glutamate release in the nucleus accumbens and ventral tegmental area of rat following lateral hypothalamic self-stimulation. Neuroscience 107: 629–639.
Acknowledgements
The project described was supported by Award Number R03DA026578 of the National Institute on Drug Abuse to UR. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Drug Abuse or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
UR is a consultant for Sunovion and Concert Pharmaceuticals. WAC has a US patent covering the use of kappa antagonists in the treatment of depression (Assignee: McLean Hospital). In the last 3 years, WAC has received compensation for professional services from The American College of Neuropsychopharmacology and Myneurolab.com.
Rights and permissions
About this article
Cite this article
Reynolds, L., Engin, E., Tantillo, G. et al. Differential Roles of GABAA Receptor Subtypes in Benzodiazepine-Induced Enhancement of Brain-Stimulation Reward. Neuropsychopharmacol 37, 2531–2540 (2012). https://doi.org/10.1038/npp.2012.115
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2012.115
Keywords
This article is cited by
-
Self-administration of benzodiazepine and cocaine combinations by male and female rhesus monkeys in a choice procedure: role of α1 subunit–containing GABAA receptors
Psychopharmacology (2019)
-
TPA-023 attenuates subchronic phencyclidine-induced declarative and reversal learning deficits via GABAA receptor agonist mechanism: possible therapeutic target for cognitive deficit in schizophrenia
Neuropsychopharmacology (2018)
-
Abuse-related effects of subtype-selective GABAA receptor positive allosteric modulators in an assay of intracranial self-stimulation in rats
Psychopharmacology (2017)
-
A Pharmacogenetic ‘Restriction-of-Function’ Approach Reveals Evidence for Anxiolytic-Like Actions Mediated by α5-Containing GABAA Receptors in Mice
Neuropsychopharmacology (2016)
-
The Role of Benzodiazepines in the Treatment of Epilepsy
Current Treatment Options in Neurology (2016)