Abstract
The exposure to pesticides and toxic compounds in xenobiotic transport and metabolism genes has been shown to affect risk of developing multiple myeloma (MM). Therefore, we hypothesized that genetic variations in xenobiotic transport and metabolism regulator genes PXR (NR1I2) and CAR (NR1I3) could determine a difference in MM susceptibility. Ten tagging single-nucleotide polymorphisms (SNPs) for PXR and seven for the CAR genes were selected and genotyped in 627 MM cases and 883 controls collected in the context of the International Multiple Myeloma rESEarch (IMMEnSE) consortium. None of the 17 SNPs investigated showed significant association with MM risk either alone or when combined in haplotypes. Significant SNP–SNP interactions were not found, neither with 58 previously genotyped polymorphisms in ABC transporters. We can therefore exclude that common genetic variants in the xenobiotic transport and metabolism regulator genes PXR and CAR affect MM risk.
Similar content being viewed by others
Introduction
Multiple myeloma (MM) is a hematological neoplasm with a worldwide incidence of 1.5/100 000 new cases/year. The disease is slightly more frequent in males than females, and the mean age at diagnosis is around 60 years.1 It has been shown that MM could evolve from an asymptomatic premalignant stage termed monoclonal gammopathy of undetermined significance (MGUS). The rate of progression of this condition to MM is around 1.5% per year, and about 15–17% of MGUS subjects develop MM.2 Among other proposed risk factors, pesticides and toxic compounds have been shown to affect the risk of developing MM and MGUS.3, 4 In particular, higher incidence rates of both MM and MGUS have been shown among farmers and agricultural workers.3, 5, 6, 7
In addition, converging evidences of MM in monozygotic twins and familial aggregation of MM strongly suggest that MM etiology has a robust genetic component.8 Several case–control studies investigating the role of single-nucleotide polymorphisms (SNPs) in MM risk have been conducted, and associations of SNPs in genes involved in xenobiotic metabolism with MM risk have been reported.9, 10 Recently, we found a strong association of SNPs in the key xenobiotic transporter ABCB1 gene with the risk of MM in the largest candidate-gene study on MM risk conducted to date.11 Both evidences that the exposure to toxic compounds, and in particular pesticides, can increase the risk of MM (and its premalignant condition MGUS) and that several SNPs within genes involved in xenobiotic transport and metabolism are associated with MM risk suggest that the xenobiotic metabolism process could have an important role in MM susceptibility and that genetic variation in key genes within this pathway can further affect the individual risk to develop MM. Although the role of genetic variation in xenobiotic metabolism enzymes and transporters has been already extensively studied, no study focused on the role of regulators of xenobiotic transport and metabolism.
The pregnane X receptor (PXR or NR1I2) and the constitutive androstane receptor (CAR or NR1I3) are the most known and well-characterized regulators of xenobiotic transport and metabolism. These proteins belong to the nuclear receptor subfamily and are activated by numerous xenobiotics, drugs, bile acids and hormones. It has been shown that several environmental, occupational and natural products, among which pesticides (some of which specifically linked with MM risk3, 5, 6, 7), can activate (or inactivate) both PXR and CAR.12 The activation of PXR and CAR leads to the induction of several detoxification enzymes (that is, phase I cytochrome P450 enzymes, phase II enzymes, such as uridine diphospho-glucorunosyltransferase, glutathione-S-transferases and sulfutransferases, and the phase III transporters, such as ABCB1 and ABCG2).12 In addition, PXR and CAR have shown to be highly polymorphic genes with several SNPs identified within their coding or regulatory sequences. Indeed, genetic variants within PXR and CAR genes have been related to differential gene expression of some of the detoxifying enzymes activated by these receptors.12, 13, 14 For this reason, it has been hypothesized that part of the individual variability in xenobiotic metabolism efficiency could be due to the genetic variations within these regulator genes.15
Therefore, to address the hypothesis that genetic variants in PXR and CAR genes could affect the risk of MM, we selected 17 SNPs in the PXR and CAR genes and genotyped them in 627 MM cases and 883 controls.
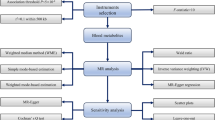
Materials and methods
Study population
The study population consisted of 627 MM cases and 883 controls (Table 1). This study way carried out in the context of the International Multiple Myeloma rESEarch (IMMEnSE) consortium, a recently created working group that aims to study genetics and pharmacogenetics of MM.10, 16, 17 Briefly, cases were defined by a confirmed diagnosis of MM, according to the International Myeloma Working Group criteria.18 Incident cases of MM diagnosed between 1990–2010 were recruited, whereas subjects with uncertain diagnosis or MGUS were excluded. Different region-specific subpopulations of controls were selected among the general population, as well as among hospitalized subjects with different diagnoses, excluding cancer.
For each subject, informed consent to collect fresh blood and perform DNA extraction for research purpose was requested and collected individually by each center. The study has been approved by the competent ethical committees.
SNP selection and genotyping
We used a tagging SNP approach for the selection of the genetic variants within the PXR and the CAR genes. The entire set of common genetic variants (including 5 kb upstream of the first exon and 5 kb downstream of the last exon of each gene), with minor allele frequency (MAF) ⩾5% in Caucasians from the International HapMap Project (release no. 26; http://www.hapmap.org), was included for both genes. Tagging SNPs were selected using the Tagger algorithm available through Haploview (http://www.broad.mit.edu/mpg/haploview/; http://www.broad.mit.edu/mpg/tagger/), using pairwise SNP selection with a minimum r2 threshold of 0.8. This selection resulted in 10 tagging SNPs for PXR and 7 for CAR. Genotyping was carried out at the German Cancer Research Center (DKFZ) in Heidelberg, where the IMMEnSE bio-bank is set up, on genomic DNA extracted from peripheral blood, using both TaqMan (Applied Biosystems, Foster City, CA, USA) and KASPar (KBioscence, Hoddesdon, UK) technologies. The order of DNAs from cases and controls was randomized on plates to ensure that an equal number of cases and controls were analyzed simultaneously. For quality-control purpose, duplicates of 10% of the samples were interspersed throughout the plates. PCR plates for both TaqMan and KASPar assays were read on an ABI PRISM 7900HT instrument (Applied Biosystems). The SDS Software, version 2.4 (Applied Biosystems) was used to determine the genotypes. Subjects whose samples had a call rate <75% were dropped from any analysis. Once subjects with low call rate were removed, all SNPs had a call rate >95%.
Statistical analysis
The Hardy–Weinberg equilibrium was tested in controls for each polymorphism. The χ2- and Kruskal–Wallis tests were used to compare gender and age distributions between MM patients and controls. Unconditional logistic regression was used to assess the main effects of the genetic polymorphisms on MM risk using a co-dominant and a dominant inheritance model. For each SNP, the more common allele in the controls was assigned as the reference category. All analyses were adjusted for age (continuous), gender and region of origin, and were conducted with STATA software (StataCorp, College Station, TX, USA).
Because of the large number of SNPs analyzed, a conservative threshold for statistical significance was applied, based on a revised version of the Bonferroni method.19
Haplotype blocks were identified from the genotyping data of the controls using SNPtool (http://www.dkfz.de/de/molgen_epidemiology/tools/SNPtool.html)20 and the Haploview v4.2 software. A MAF >0.05, Hardy–Weinberg equilibrium P>0.001 and a call rate >75% were used as cut-off values. Individual haplotypes were then statistically inferred using the PHASE v.2.1.1 algorithm, based on a Bayesian approach (http://www.stat.Washington.edu/stephens/).21, 22 Unconditional logistic regression was used to estimate risk. The most frequent haplotype was set as reference, whereas haplotypes with a frequency <3% were declared as rare and combined in a single category.
SNP–SNP interactions were tested using the nonparametric Multifactor Dimensionality Reduction approach. Detailed information is described elsewhere,23 and the Multifactor Dimensionality Reduction software is available from http://www.epistasis.org.
Results and Discussion
MM cases and controls had similar gender and age distributions (χ2=0.717, Kruskal–Wallis=0.39). All the SNPs were in Hardy–Weinberg equilibrium among controls (P>0.02), with the exception of the PXR rs2461818 (P=0.0003), which was therefore excluded from further analysis.
To correct for multiple testing, we calculated Meff values for each candidate gene separately (PXR=8, CAR=3) and for the whole study (by adding the individual Meff values). The study-wise Meff was 11. We therefore used a study-wise statistical significance P-value of 0.05/11=0.0045. None of the SNPs resulted associated with MM risk, with either a co-dominant or dominant inheritance model (Table 2). We reconstructed haplotypes within PXR and CAR genes based on the linkage disequilibrium blocks observed in the controls. Two haplotype blocks were identified in the PXR and one in the CAR gene. None of the individual haplotypes showed association with MM risk (Table 3). The statistically significant association for the others group (that is, rare haplotypes lumped together) within the CAR haplotype block is most likely because of the heterogeneity of the group. Further analyses within this group are prevented by the small numbers of each individual haplotype.
Finally, we evaluated SNP–SNP interactions using the nonparametric Multifactor Dimensionality Reduction approach. We investigated the interaction between PXR and CAR genotypes. In addition, we verified the presence of inter-gene interactions between the PXR and CAR genotypes and 58 previously genotyped polymorphisms in ABC transporters ABCB1, ABCG2, ABCC2, ABCC1 and ABCC3.11 We performed a stratified analysis of PXR and CAR genotypes among groups defined according to ABCB1 genotypes that we previously showed to be strongly associated with MM risk.11 Nevertheless, no evidence of associations with MM risk emerged in any case (Supplementary Table I).
At the best of our knowledge, this is the first investigation of the PXR and CAR genetic variation in relation to MM risk. Despite the strong rationale and the existing evidences suggesting a role of genetic variants in xenobiotic transport and metabolism genes in influencing MM risk, our results show no effect of SNPs in PXR and CAR genes in modifying individual susceptibility to the disease. In this study, we analyzed also the haplotype structure within the two genes and the possible SNP–SNP interactions, including the analysis of previously obtained genotypes for SNPs within ABC transporters. Moreover, our study had a sufficient statistical power to evidence the effect of common low-penetrance genetic variants, such as those expected to affect cancer susceptibility. Indeed, we achieved a statistical power of 80% to discover a minimum odds ratio (OR) of 1.34 with the smallest MAF observed among the selected tagging SNPs (0.14, rs1054190) and α=0.05. The minimum OR detectable with the same power decreased to 1.24 with the highest MAF observed (0.43, rs12488820). Thus, we had sufficient power to detect risks of the magnitude commonly observed with genetic polymorphisms.
In the light of our thorough investigation showing overall negative results, we are keen to exclude a role of common genetic variations in the xenobiotic transporter and metabolism regulator genes PXR and CAR in MM etiology. Although the tag SNP approach accounts for >95% of the genetic variations with a MAF ⩾0.05 in both genes, including functional variants, we cannot exclude the presence of functional SNPs with a lower frequency that could still affect MM risk. Further studies in this sense are needed to identify and establish genetic risk factors for MM.
References
Ferlay, J., Shin, H. R., Bray, F., Forman, D., Mathers, C. & Parkin, D. M. GLOBOCAN 2008 v2.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 [Internet], International Agency for Research on Cancer: Lyon, France, (2010) Available from: http://globocan.iarc.fr).
Kyle, R. A., Therneau, T. M., Rajkumar, S. V., Larson, D. R., Plevak, M. F. & Melton, L. J. Long-term follow-up of 241 patients with monoclonal gammopathy of undetermined significance: the original Mayo Clinic series 25 years later. Mayo Clin. Proc. 79, 859–866 (2004).
Landgren, O., Kyle, R. A., Hoppin, J. A., Beane Freeman, L. E., Cerhan, J. R., Katzmann, J. A. et al. Pesticide exposure and risk of monoclonal gammopathy of undetermined significance in the Agricultural Health Study. Blood 113, 6386–6391 (2009).
Lope, V., Perez-Gomez, B., Aragones, N., Lopez-Abente, G., Gustavsson, P., Plato, N. et al. Occupation, exposure to chemicals, sensitizing agents, and risk of multiple myeloma in Sweden. Cancer Epidemiol. Biomarkers Prev. 17, 3123–3127 (2008).
Koutros, S., Alavanja, M. C., Lubin, J. H., Sandler, D. P., Hoppin, J. A., Lynch, C. F. et al. An update of cancer incidence in the Agricultural Health Study. J. Occup. Environ. Med. 52, 1098–1105 (2010).
Perrotta, C., Staines, A. & Cocco, P. Multiple myeloma and farming. A systematic review of 30 years of research. Where next? J. Occup. Med. Toxicol. 3, 27 (2008).
Pahwa, P., Karunanayake, C. P., Dosman, J. A., Spinelli, J. J., McDuffie, H. H. & McLaughlin, J. R. Multiple myeloma and exposure to pesticides: a Canadian case-control study. J. Agromed. 17, 40–50 (2011).
Landgren, O. & Weiss, B. M. Patterns of monoclonal gammopathy of undetermined significance and multiple myeloma in various ethnic/racial groups: support for genetic factors in pathogenesis. Leukemia 23, 1691–1697 (2009).
Lincz, L. F., Kerridge, I., Scorgie, F. E., Bailey, M., Enno, A. & Spencer, A. Xenobiotic gene polymorphisms and susceptibility to multiple myeloma. Haematologica 89, 628–629 (2004).
Martino, A., Sainz, J., Buda, G., Jamroziak, K., Reis, R. M., Garcia-Sanz, R. et al. Genetics and molecular epidemiology of multiple myeloma: the rationale for the IMMEnSE consortium (review). Int. J. Oncol. 40, 625–638 (2011).
Martino, A., Campa, D., Buda, G., Sainz, J., Garcia-Sanz, R., Jamroziak, K. et al. Polymorphisms in xenobiotic transporters ABCB1, ABCG2, ABCC2, ABCC1, ABCC3 and multiple myeloma risk: a case-control study in the context of the International Multiple Myeloma rESEarch (IMMEnSE) consortium. Leukemia 26, 1419–1422 (2011).
Hernandez, J. P., Mota, L. C. & Baldwin, W. S. Activation of CAR and PXR by dietary, environmental and occupational chemicals alters drug metabolism, intermediary metabolism, and cell proliferation. Curr. Pharmacogenomics Person. Med. 7, 81–105 (2009).
Zhang, B., Xie, W. & Krasowski, M. D. PXR: a xenobiotic receptor of diverse function implicated in pharmacogenetics. Pharmacogenomics 9, 1695–1709 (2008).
Lamba, J. K. Pharmacogenetics of the constitutive androstane receptor. Pharmacogenomics 9, 71–83 (2008).
Timsit, Y. E. & Negisi, M. CAR and PXR: the xenobiotic-sensing receptors. Steroids 72, 231–246 (2007).
Campa, D., Martino, A., Sainz, J., Buda, G., Jamroziak, K., Weinhold, N. et al. Comprehensive investigation of genetic variation in the 8q24 region and multiple myeloma risk in the IMMEnSE consortium. Br. J. Haematol. 157, 331–338 (2012).
Martino, A., Campa, D., Jamroziak, K., Reis, R. M., Sainz, J., Buda, G. et al. Impact of polymorphic variation at 7p15.3, 3p22.1 and 2p23.3 loci on risk of multiple myeloma. Br. J. Haematol. 158, 805–809 (2012).
International Myeloma Working Group. Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br. J. Haematol. 121, 749–757 (2003).
Gao, X., Starmer, J. & Martin, E. R. A multiple testing correction method for genetic association studies using correlated single nucleotide polymorphisms. Genet. Epidemiol. 32, 361–369 (2008).
Chen, B., Wilkening, S., Drechsel, M. & Hemminki, K. SNP_tools: A compact tool package for analysis and conversion of genotype data for MS-Excel. BMC Res. Notes 2, 214 (2009).
Stephens, M. & Scheet, P. Accounting for decay of linkage disequilibrium in haplotype inference and missing-data imputation. Am. J. Hum. Genet. 76, 449–462 (2005).
Stephens, M., Smith, N. J. & Donnelly, P. A new statistical method for haplotype reconstruction from population data. Am. J. Hum. Genet. 68, 978–989 (2001).
Moore, J. H. Computational analysis of gene-gene interactions using multifactor dimensionality reduction. Expert Rev. Mol. Diagn. 4, 795–803 (2004).
Acknowledgements
We thank for the support by the recruiting hospitals and physicians of the study regions, as well as their collaborating nurses and technicians.
Author contributions
AM, DC and FC designed the study, performed the genotyping and the statistical analysis and wrote the original draft of the manuscript. AS performed the genotyping. JS, RMR, VM, GB, FL, HM, RG-S, RR, CD, FG, AMR, SL, MJ, MP and KJ recruited cases and controls and provided DNA samples and the clinical information. All the authors approved the final version submitted.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Journal of Human Genetics website
Supplementary information
Rights and permissions
About this article
Cite this article
Martino, A., Sainz, J., Manuel Reis, R. et al. Polymorphisms in regulators of xenobiotic transport and metabolism genes PXR and CAR do not affect multiple myeloma risk: a case–control study in the context of the IMMEnSE consortium. J Hum Genet 58, 155–159 (2013). https://doi.org/10.1038/jhg.2012.149
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/jhg.2012.149
Keywords
This article is cited by
-
Genetic predisposition for multiple myeloma
Leukemia (2020)