Abstract
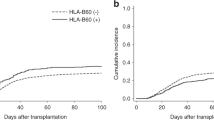
In 8/8 HLA-matched unrelated donor (UD) hematopoietic cell transplants (HCT), HLA-DPB1 mismatches between alleles from different T-cell epitope (TCE) groups (non-permissive mismatches) are associated with significantly higher risks of mortality compared with those between alleles from the same TCE group (permissive mismatches); however, the relevance of mismatch directionality, that is (host vs graft (uni-directional HvG), graft vs host (uni-directional GvH) or both (bi-directional) in the non-permissive setting is unknown. We show here significantly higher in vitro relative responses (RR) to bi-directional mismatches compared with uni-directional HvG or GvH mismatches in a total of 420 one-way mixed lymphocyte reactions between 10/10 matched pairs (RR 27.5 vs 7.5 vs 15.5, respectively, P<0.001). However, in 3281 8/8 matched UD HCT for leukemia or myelodysplastic syndrome, the hazards of transplant-related mortality (TRM) were similar for uni-directional HvG or GvH mismatches and bi-directional mismatches (hazard ratio (HR) 1.32, P=0.001 vs HR 1.28, P=0.005 and HR 1.34, P=0.046), compared with permissive mismatches. Similar results were observed for overall survival. No statistical differences between the uni- and the bi-directional non-permissive groups were detected in pairwise comparisons for any of the outcomes tested. We conclude that consideration of directionality does not improve risk stratification by non-permissive HLA-DPB1 TCE mismatches in UD searches.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Lee SJ, Klein J, Haagenson M, Baxter-Lowe LA, Confer DL, Eapen M et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood 2007; 110: 4576–4583.
Petersdorf EW . Optimal HLA matching in hematopoietic cell transplantation. Curr Opin Immunol 2008; 20: 588–593.
Eapen M, Rocha V, Sanz G, Scaradavou A, Zhang MJ, Arcese W et al. Effect of graft source on unrelated donor haemopoietic stem-cell transplantation in adults with acute leukaemia: a retrospective analysis. Lancet Oncol 2010; 11: 653–660.
Hurley CK, Woolfrey A, Wang T, Haagenson M, Umejiego J, Aljurf M et al. The impact of HLA unidirectional mismatches on the outcome of myeloablative hematopoietic stem cell transplantation with unrelated donors. Blood 2013; 121: 4800–4806.
Stevens CE, Carrier C, Carpenter C, Sung D, Scaradavou A . HLA mismatch direction in cord blood transplantation: impact on outcome and implications for cord blood unit selection. Blood 2011; 118: 3969–3978.
Kanda J, Ichinohe T, Fuji S, Maeda Y, Ohashi K, Fukuda T et al. Impact of HLA mismatch direction on the outcome of unrelated bone marrow transplantation: a retrospective analysis from the Japan Society for Hematopoietic Cell Transplantation. Biol Blood Marrow Transplant 2015; 21: 305–311.
Zino E, Frumento G, Marktel S, Sormani MP, Ficara F, Di Terlizzi S et al. A T-cell epitope encoded by a subset of HLA-DPB1 alleles determines nonpermissive mismatches for hematologic stem cell transplantation. Blood 2004; 103: 1417–1424.
Crocchiolo R, Zino E, Vago L, Oneto R, Bruno B, Pollichieni S et al. Nonpermissive HLA-DPB1 disparity is a significant independent risk factor for mortality after unrelated hematopoietic stem cell transplantation. Blood 2009; 114: 1437–1444.
Fleischhauer K, Shaw BE, Gooley T, Malkki M, Bardy P, Bignon JD et al. Effect of T-cell-epitope matching at HLA-DPB1 in recipients of unrelated-donor haemopoietic-cell transplantation: a retrospective study. Lancet Oncol 2012; 13: 366–374.
Pidala J, Lee SJ, Ahn KW, Spellman S, Wang HL, Aljurf M et al. Nonpermissive HLA-DPB1 mismatch increases mortality after myeloablative unrelated allogeneic hematopoietic cell transplantation. Blood 2014; 124: 2596–2606.
Zino E, Vago L, Di Terlizzi S, Mazzi B, Zito L, Sironi E et al. Frequency and targeted detection of HLA-DPB1 T cell epitope disparities relevant in unrelated hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2007; 13: 1031–1040.
Crivello P, Zito L, Sizzano F, Zino E, Maiers M, Mulder A et al. The impact of amino acid variability on alloreactivity defines a functional distance predictive of permissive HLA-DPB1 mismatches in hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 2015; 21: 233–241.
Sizzano F, Zito L, Crivello P, Crocchiolo R, Vago L, Zino E et al. Significantly higher frequencies of alloreactive CD4+ T cells responding to nonpermissive than to permissive HLA-DPB1 T-cell epitope disparities. Blood 2010; 116: 1991–1992.
Bochtler W, Gragert L, Patel ZI, Robinson J, Steiner D, Hofmann JA et al. A comparative reference study for the validation of HLA-matching algorithms in the search for allogeneic hematopoietic stem cell donors and cord blood units. HLA 2016; 87: 439–448.
Spellman SR, Eapen M, Logan BR, Mueller C, Rubinstein P, Setterholm MI et al. A perspective on the selection of unrelated donors and cord blood units for transplantation. Blood 2012; 120: 259–265.
Shaw BE, Robinson J, Fleischhauer K, Madrigal JA, Marsh SG . Translating the HLA-DPB1 T-cell epitope-matching algorithm into clinical practice. Bone Marrow Transplant 2013; 48: 1510–1512.
van den Tweel JG, van Oud Alblas AB, Keuning JJ, Goulmy E, Termijtelen A, Bach ML et al. Typing for MLC (LD). I. Lymphocytes from cousin-marriage offspring as typing cells. Transplant Proc 1973; 5: 1535–1538.
Spellman S, Setterholm M, Maiers M, Noreen H, Oudshoorn M, Fernandez-Vina M et al. Advances in the selection of HLA-compatible donors: refinements in HLA typing and matching over the first 20 years of the National Marrow Donor Program Registry. Biol Blood Marrow Transplant 2008; 14: 37–44.
Hollenbach JA, Madbouly A, Gragert L, Vierra-Green C, Flesch S, Spellman S et al. A combined DPA1~DPB1 amino acid epitope is the primary unit of selection on the HLA-DP heterodimer. Immunogenetics 2012; 64: 559–569.
Rutten CE, van Luxemburg-Heijs SA, van der Meijden ED, Griffioen M, Oudshoorn M, Willemze R et al. HLA-DPB1 mismatching results in the generation of a full repertoire of HLA-DPB1-specific CD4+ T cell responses showing immunogenicity of all HLA-DPB1 alleles. Biol Blood Marrow Transplant 2010; 16: 1282–1292.
Rutten CE, van Luxemburg-Heijs SA, van der Meijden ED, Griffioen M, Oudshoorn M, Willemze R et al. Both permissive and nonpermissive HLA-DPB1 mismatches can induce polyclonal HLA-DPB1 specific immune responses in vivo and in vitro. Blood 2010; 115: 151–153.
Shaw BE, Gooley TA, Malkki M, Madrigal JA, Begovich AB, Horowitz MM et al. The importance of HLA-DPB1 in unrelated donor hematopoietic cell transplantation. Blood 2007; 110: 4560–4566.
Shaw BE, Mayor NP, Russell NH, Apperley JF, Clark RE, Cornish J et al. Diverging effects of HLA-DPB1 matching status on outcome following unrelated donor transplantation depending on disease stage and the degree of matching for other HLA alleles. Leukemia 2010; 24: 58–65.
Fleischhauer K, Fernandez-Vina MA, Wang T, Haagenson M, Battiwalla M, Baxter-Lowe LA et al. Risk associations between HLA-DPB1 T-cell epitope matching and outcome of unrelated hematopoietic cell transplantation are independent of HLA-DPA1. Bone Marrow Transplant 2014; 49: 1176–1183.
Rutten CE, van Luxemburg-Heijs SA, Griffioen M, Marijt EW, Jedema I, Heemskerk MH et al. HLA-DP as specific target for cellular immunotherapy in HLA class II-expressing B-cell leukemia. Leukemia 2008; 22: 1387–1394.
Herr W, Eichinger Y, Beshay J, Bloetz A, Vatter S, Mirbeth C et al. HLA-DPB1 mismatch alleles represent powerful leukemia rejection antigens in CD4 T-cell immunotherapy after allogeneic stem-cell transplantation. Leukemia 2017; 31: 434–445.
Kanda J, Atsuta Y, Wake A, Ichinohe T, Takanashi M, Morishima Y et al. Impact of the direction of HLA mismatch on transplantation outcomes in single unrelated cord blood transplantation. Biol Blood Marrow Transplant 2013; 19: 247–254.
Crivello P, Heinold A, Rebmann V, Ottinger HD, Horn PA, Beelen DW et al. Functional distance between recipient and donor HLA-DPB1 determines nonpermissive mismatches in unrelated HCT. Blood 2016; 128: 120–129.
Petersdorf EW, Malkki M, O'hUigin C, Carrington M, Gooley T, Haagenson MD et al. High HLA-DP expression and graft versus host disease. N Engl J Med 2015; 373: 599–609.
Fleischhauer K . Immunogenetics of HLA-DP—A New View of Permissible Mismatches. N Engl J Med 2015; 373: 669–672.
Joris MM, van Rood JJ, Roelen DL, Oudshoorn M, Claas FH . A proposed algorithm predictive for cytotoxic T cell alloreactivity. J Immunol 2012; 188: 1868–1873.
Joris MM, Lankester AC, von dem Borne PA, Kuball J, Bierings M, Cornelissen JJ et al. Translating in vitro prediction of cytotoxic T cell alloreactivity to hematopoietic stem cell transplantation outcome. Transplant Immunol 2014; 30: 59–64.
Acknowledgements
This work was supported by grants from the Deutsche José Carreras Leukämie Stiftung (DJCLS R 15/02) and from the Joseph Senker Stiftung to K.F. The CIBMTR is supported by Public Health Service Grant/Cooperative Agreement 5U24-CA076518 from the National Cancer Institute (NCI), the National Heart, Lung and Blood Institute (NHLBI) and the National Institute of Allergy and Infectious Diseases (NIAID); a Grant/Cooperative Agreement 5U10HL069294 from NHLBI and NCI; a contract HHSH250201200016C with Health Resources and Services Administration (HRSA/DHHS); two Grants N00014-15-1-0848 and N00014-16-1-2020 from the Office of Naval Research; and grants from Alexion; *Amgen, Inc.; Anonymous donation to the Medical College of Wisconsin; Astellas Pharma US; AstraZeneca; Be the Match Foundation; *Bluebird Bio, Inc.; *Bristol Myers Squibb Oncology; *Celgene Corporation; Cellular Dynamics International, Inc.; *Chimerix, Inc.; Fred Hutchinson Cancer Research Center; Gamida Cell Ltd.; Genentech, Inc.; Genzyme Corporation; *Gilead Sciences, Inc.; Health Research, Inc. Roswell Park Cancer Institute; HistoGenetics, Inc.; Incyte Corporation; Janssen Scientific Affairs, LLC; *Jazz Pharmaceuticals, Inc.; Jeff Gordon Children’s Foundation; The Leukemia & Lymphoma Society; Medac, GmbH; MedImmune; The Medical College of Wisconsin; *Merck & Co, Inc.; Mesoblast; MesoScale Diagnostics, Inc.; *Miltenyi Biotec, Inc.; National Marrow Donor Program; Neovii Biotech NA, Inc.; Novartis Pharmaceuticals Corporation; Onyx Pharmaceuticals; Optum Healthcare Solutions, Inc.; Otsuka America Pharmaceutical, Inc.; Otsuka Pharmaceutical Co, Ltd.–Japan; PCORI; Perkin Elmer, Inc.; Pfizer, Inc; *Sanofi US; *Seattle Genetics; *Spectrum Pharmaceuticals, Inc.; St. Baldrick’s Foundation; *Sunesis Pharmaceuticals, Inc.; Swedish Orphan Biovitrum, Inc.; Takeda Oncology; Telomere Diagnostics, Inc.; University of Minnesota; and *Wellpoint, Inc. The views expressed in this article do not reflect the official policy or position of the National Institute of Health, the Department of the Navy, the Department of Defense, Health Resources and Services Administration (HRSA) or any other agency of the U.S. Government (*Corporate Members).
Author contributions
KF designed and supervised the study and wrote the manuscript. LZ performed the analysis of experimental data. PC supervised the analysis of experimental data and the HLA-DPB1 assignments of clinical data. MO performed and provided the experimental data. KWA and HW performed statistical analyses. KF, SRS, SJL and KWA interpreted the statistical analysis results. KF, KWA, HW, LZ, PC, CM, MV, BES, JP, MO, SJL and SRS participated in the writing and editing of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Fleischhauer, K., Ahn, K., Wang, H. et al. Directionality of non-permissive HLA-DPB1 T-cell epitope group mismatches does not improve clinical risk stratification in 8/8 matched unrelated donor hematopoietic cell transplantation. Bone Marrow Transplant 52, 1280–1287 (2017). https://doi.org/10.1038/bmt.2017.96
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2017.96
This article is cited by
-
Host versus graft HLA-DP1 mismatching promotes graft versus host disease
Bone Marrow Transplantation (2023)