Abstract
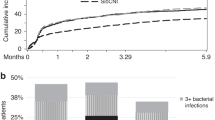
Antibiotic prophylaxis has been used during the initial phases of myeloablative hematopoietic cell transplantation (HCT) for more than two decades. However, the optimal regimen in terms of both cost and clinical effectiveness is unclear. We retrospectively compared the clinical and microbiological impact of a change in antibiotic prophylaxis practice from ceftazidime (n=216 patients with HCT in 2000–2002) to levofloxacin (n=219 patients, August 2002–2005) in patients receiving myeloablative conditioning. Levofloxacin prophylaxis was associated with fever and a change in antibiotics during neutropenia, but this strategy was not associated with any adverse outcomes. Patients receiving levofloxacin had lower rates of significant bacteremia than did those receiving ceftazidime (day 100, 19.2 vs 29.6%, P=0.02). The use of levofloxacin was associated with lower antibiotic acquisition costs. There was no deleterious impact caused by levofloxacin prophylaxis on survival, emergence of antibiotic resistance, detection of Clostridium difficile Ag in stool specimens, incidence of viridans group streptococcal bacteremia or Pseudomonas infections. There was a trend toward lower rates of bacteriuria, wound and bacterial respiratory infections in the levofloxacin than in the ceftazidime group, but these differences were not statistically significant. These data support the use of levofloxacin as prophylaxis in myeloablative allogeneic HCT when prophylaxis is used.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Gratwohl A, Brand R, Frassoni F, Rocha V, Niederwieser D, Reusser P et al. Cause of death after allogeneic haematopoietic stem cell transplantation (HSCT) in early leukaemias: an EBMT analysis of lethal infectious complications and changes over calendar time. Bone Marrow Transplant 2005; 36: 757–769.
Hughes WT, Armstrong D, Bodey GP, Bow EJ, Brown AE, Calandra T et al. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin Infect Dis 2002; 34: 730–751.
Bodey GP, Buckley M, Sathe YS, Freireich EJ . Quantitative relationships between circulating leukocytes and infection in patients with acute leukemia. Ann Intern Med 1966; 64: 328–340.
Pizzo PA, Robichaud KJ, Gill FA, Witebsky FG . Empiric antibiotic and antifungal therapy for cancer patients with prolonged fever and granulocytopenia. Am J Med 1982; 72: 101–111.
Petersen F, Thornquist M, Buckner C, Counts G, Nelson N, Meyers J et al. The effects of infection prevention regimens on early infectious complications in marrow transplant patients: a four arm randomized study. Infection 1988; 16: 199–208.
Gafter-Gvili A, Paul M, Fraser A, Leibovici L . Effect of quinolone prophylaxis in afebrile neutropenic patients on microbial resistance: systematic review and meta-analysis (Review). J Antimicrob Chemother 2007; 59: 5–22.
Gafter-Gvili A, Fraser A, Paul M, Leibovici L . Meta-analysis: antibiotic prophylaxis reduces mortality in neutropenic patients [erratum appears in Ann Intern Med. 2006 May 2;144(9):704]. Ann Intern Med 2005; 142: 979–995.
von Baum H, Sigge A, Bommer M, Kern WV, Marre R, Dohner H et al. Moxifloxacin prophylaxis in neutropenic patients. J Antimicrob Chemother 2006; 58: 891–894.
Bucaneve G, Micozzi A, Menichetti F, Martino P, Dionisi MS, Martinelli G et al. Levofloxacin to prevent bacterial infection in patients with cancer and neutropenia. N Engl J Med 2005; 353: 977–987.
Cullen M, Steven N, Billingham L, Gaunt C, Hastings M, Simmonds P et al. Antibacterial prophylaxis after chemotherapy for solid tumors and lymphomas. N Engl J Med 2005; 353: 988–998.
Gafter-Gvili A, Fraser A, Paul M, van de WM, Kremer L, Leibovici L . Antibiotic prophylaxis for bacterial infections in afebrile neutropenic patients following chemotherapy (Review). Cochrane Database of Systematic Review, vol 4, 2005, Article no. CD004386.
Leibovici L, Paul M, Cullen M, Bucaneve G, Gafter-Gvili A, Fraser A et al. Antibiotic prophylaxis in neutropenic patients: new evidence, practical decisions (Review). Cancer 2006; 107: 1743–1751.
Baden LR . Prophylactic antimicrobial agents and the importance of fitness. N Engl J Med 2005; 353: 1052–1054.
Pepin J, Saheb N, Coulombe MA, Alary ME, Corriveau MP, Authier S et al. Emergence of fluoroquinolones as the predominant risk factor for Clostridium difficile-associated diarrhea: a cohort study during an epidemic in Quebec. Clin Infect Dis 2005; 41: 1254–1260.
Loo VG, Poirier L, Miller MA, Oughton M, Libman MD, Michaud S et al. A predominantly clonal multi-institutional outbreak of Clostridium difficile-associated diarrhea with high morbidity and mortality [erratum appears in N Engl J Med 2006; 354: 2200]. N Engl J Med 2005; 353: 2442–2449.
Razonable RR, Litzow MR, Khaliq Y, Piper KE, Rouse MS, Patel R . Bacteremia due to viridans group streptococci with diminished susceptibility to levofloxacin among neutropenic patients receiving levofloxacin prophylaxis. Clin Infect Dis 2002; 34: 1469–1474.
Acknowledgements
We acknowledge W Garrett Nichols and Michael Boeckh for their contributions to the study design, and Chris Davis and Gary Schoch for database support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Guthrie, K., Yong, M., Frieze, D. et al. The impact of a change in antibacterial prophylaxis from ceftazidime to levofloxacin in allogeneic hematopoietic cell transplantation. Bone Marrow Transplant 45, 675–681 (2010). https://doi.org/10.1038/bmt.2009.216
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bmt.2009.216
Keywords
This article is cited by
-
Soll die asymptomatische Bakteriurie bei Immunsupprimierten antibiotisch therapiert werden?
Die Urologie (2023)
-
Bacteremia during neutropenic episodes in children undergoing hematopoietic stem cell transplantation with ciprofloxacin and penicillin prophylaxis
International Journal of Hematology (2017)
-
Bacteremia During Early Post-allogeneic Hematopoietic Stem Cell Transplantation Period: A Single Center Experience
Indian Journal of Hematology and Blood Transfusion (2017)
-
Breakthrough viridans streptococcal bacteremia in allogeneic hematopoietic stem cell transplant recipients receiving levofloxacin prophylaxis in a Japanese hospital
BMC Infectious Diseases (2016)
-
Clostridium difficile: Deleterious Impact on Hematopoietic Stem Cell Transplantation
Current Hematologic Malignancy Reports (2014)