Abstract
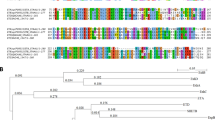
Exfoliative toxin A, produced by Staphylococcus aureus, causes blisters in bullous impetigo and its more generalized form, staphylococcal scalded-skin syndrome1,2,3. The toxin shows exquisite specificity in causing loss of cell adhesion only in the superficial epidermis. Although exfoliative toxin A has the structure of a serine protease, a target protein has not been identified4,5. Desmoglein (Dsg) 1, a desmosomal cadherin that mediates cell–cell adhesion, may be the target of exfoliative toxin A, because it is the target of autoantibodies in pemphigus foliaceus, in which blisters form with identical tissue specificity and histology. We show here that exfoliative toxin A cleaved mouse and human Dsg1, but not closely related cadherins such as Dsg3. We demonstrate this specific cleavage in cell culture, in neonatal mouse skin and with recombinant Dsg1, and conclude that Dsg1 is the specific receptor for exfoliative toxin A cleavage. This unique proteolytic attack on the desmosome causes a blister just below the stratum corneum, which forms the epidermal barrier, presumably allowing the bacteria in bullous impetigo to proliferate and spread beneath this barrier.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Farrell, A.M. Staphylococcal scalded-skin syndrome. Lancet 354, 880–881 (1999).
Melish, M.E. & Glasgow, L.A. Staphylococcal scalded skin syndrome: The expanded clinical syndrome. J. Pediatrics 78, 958–967 (1971).
Elias, P.M., Fritsch, P. & Epstein, Jr. E.H. Staphylococcal scalded skin syndrome. Clinical features, pathogenesis, and recent microbiological and biochemical developments. Arch. Dermatol. 113, 207– 219 (1977).
Dancer, S.J., Garratt, R., Saldanha, J., Jhoti, H. & Evans, R. The epidermolytic toxins are serine proteases. FEBS Letters 268, 129– 132 (1990).
Vath, G.M. et al. The structure of the superantigen exfoliative toxin A suggests a novel regulation as a serine protease. Biochemistry 36, 1559–1566 (1997).
Lyell, A. The staphylococcal scalded skin syndrome in historical perspective: emergence of dermopathic strains of Staphylococcal aureus and discovery of the epidermolytic toxin. J. Am. Acad. Dermatol. 9, 285–294 (1983).
Rago, J.V., Vath, G.M., Bohach, G.A., Ohlendorf, D.H. & Schlievert, P.M. Mutational analysis of the superantigen staphylococcal exfoliative toxin A (ETA). J. Immunol. 164, 2207–2213 (2000).
Mahoney, M.G. et al. Explanation for the clinical and microscopic localization of lesions in pemphigus foliaceus and vulgaris. J. Clin. Invest. 103, 461–468 ( 1999).
Melish, M.E. & Glasgow, L.A. The staphylococcal scalded-skin syndrome. Development of an experimental model. N. Engl. J. Med. 282, 1114–1119 (1970).
Nilles, L.A. et al. Structural analysis and expression of human desmoglein: a cadherin-like component of the desmosome. J. Cell Science 99, 809–821 (1991).
Koch, P.J. et al. Desmoglein 3 anchors telogen hair in the follicle. J. Cell Sci. 111, 2529–2537 (1998).
Hopp, T.P. et al. A short polypeptide marker sequence useful for recombinant protein identification and purification. Biotechnology 6, 1205–1210 (1988).
Ishikawa, H. et al. cDNA cloning and chromosomal assignment of the mouse gene for desmoglein 3 (Dsg3), the pemphigus vulgaris antigen. Mammalian Genome 5, 803–804 ( 1994).
Ishikawa, H., Li, K., Sawamura, D. & Uitto, J. Cloning of the mouse desmoglein 3 gene (Dsg3): interspecies conservation within the cadherin superfamily. Exp. Dermatol. 9, 229– 239 (2000).
Wu, H. et al. Protection of neonates against pemphigus foliaceus by desmoglein 3. N. Engl. J. Med. 343, 31– 35 (2000).
Shirayoshi, Y., Nose, A., Iwasaki, K. & Takeichi, M. N-linked oligosaccharides are not involved in the function of a cell-cell binding glycoprotein E-cadherin. Cell Struct. Funct. 11, 245–252 (1986).
Ishii, K. et al. Characterization of autoantibodies in pemphigus using antigen-specific enzyme-linked immunosorbent assays with baculovirus-expressed recombinant desmogleins. J. Immunol. 159, 2010– 2017 (1997).
Amagai, M. et al. Use of autoantigen-knockout mice in developing an active autoimmune disease model for pemphigus. J. Clin. Invest. 105, 625–631 (2000).
Acknowledgements
This work was supported by grants from the National Institute of Arthritis, Musculoskeletal, and Skin Diseases, and Grants for Research on Specific Diseases from the Ministry of Health and Welfare of Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Amagai, M., Matsuyoshi, N., Wang, Z. et al. Toxin in bullous impetigo and staphylococcal scalded-skin syndrome targets desmoglein 1. Nat Med 6, 1275–1277 (2000). https://doi.org/10.1038/81385
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/81385
This article is cited by
-
Management of Infectious Emergencies for the Inpatient Dermatologist
Current Dermatology Reports (2021)
-
Kutane Infektionen durch Staphylokokken und Streptokokken
hautnah dermatologie (2021)
-
Whole-genome epidemiology, characterisation, and phylogenetic reconstruction of Staphylococcus aureus strains in a paediatric hospital
Genome Medicine (2018)