Abstract
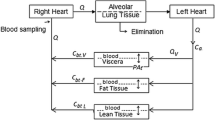
Physiologically based pharmacokinetic (PBPK) models can be used to predict drug disposition in humans from animal data and the influence of disease or other changes in physiology on the pharmacokinetics of a drug. The potential usefulness of a PBPK model must however be balanced against the considerable effort needed for its development. Proposed methods to simplify PBPK modeling include predicting the necessary tissue:blood partition coefficients (kp) from physicochemical data on the drug instead of determining them in vivo, formal lumping of model compartments, and replacing the various kp values of the organs and tissues by only two values, for “fat” and “lean” tissues, respectively. The aim of this study was to investigate the effects of simplifying complex PBPK models on their ability to predict drug disposition in humans. Arterial plasma concentration curves of fentanyl and pethidine were simulated by means of a number of successively reduced models. Median absolute prediction errors were used to evaluate the performance of each model, in relation to arterial plasma concentration data from clinical studies, and the Wilcoxon matched pairs test was used for comparison of predictions. An originally diffusion-limited model for fentanyl was simplified to perfusion-limitation, and this model was either lumped, reducing 11 organ/tissue compartments to six, or changed to a model based on only two kp values, those of fat (used for fat and lungs) and muscle (used for all other tissues). None of these simplifications appreciably changed the predictions of arterial drug concentrations in the 10 patients. Perfusion-limited models for pethidine were set up using either experimentally determined [Gabrielsson et al. 1986] or theoretically calculated [Davis and Mapleson 1993] kp values, and predictions using the former were found to be significantly better. Lumping of the models did not appreciably change the predictions; however, going from a full set of kp values to only two (“fat” and “lean”) had an adverse effect. Using a kp for lungs determined either in rats or indirectly in humans [Persson et al. 1988], i.e., a total of three kp values, improved these predictions. In con- clusion, this study strongly suggested that complex PBPK models for lipophilic basic drugs may be considerably reduced with marginal loss of power to predict standard plasma pharmacokinetics in humans. Determination of only two or three kp values instead of a “full” set can mean an important reduction of experimental work to define a basic model. Organs of particular pharmacological or toxicological interest should of course be investigated separately as needed. This study also suggests and applies a simple method for statistical evaluation of the predictions of PBPK models.
Similar content being viewed by others
References
S. B. Charnick, R. Kawai, J. R. Nedelman, M. Lemaire, W. Niederberger, and H. Sato. Physiologically based pharmacokinetic modeling as a tool for drug development. J. Pharmacokin. Biopharm. 23:217-229 (1995).
P. Poulin and F.-P. Theil. Prediction of pharmacokinetics prior to in vivo studies. 1. Mechanism-based prediction of volume of distribution. J. Pharm. Sci. 91:129-156 (2002).
A. Boobis, U. Gundert-Remy, P. Kremers, P. Macheras, and O. Pelkonen. In silico prediction of ADME and pharmacokinetics. Report of an expert meeting organized by COST B15. Eur. J. Pharm. Sci. 17:183-193 (2002).
F.-P. Theil, T. W. Guentert, S. Haddad, and P. Poulin. Utility of physiologically based pharmacokinetic models to drug development and rational drug discovery candidate selection. Toxicol. Lett. 138:29-49 (2003).
H. L. Price. A dynamic concept of the distribution of thiopental in the human body. Anesthesiology 21:40-45 (1960).
D. R. Wada, S. Björkman, W. F. Ebling, H. Harashima, S. R. Harapat, and D. R. Stanski. Computer simulation of the effects of alterations in blood flows and body composition on thiopental pharmacokinetics in humans. Anesthesiology 87:884-899 (1997).
S. Björkman, D.R. Wada, and D.R. Stanski. Application of physiological models to predict the influence of changes in body composition and blood flows on the pharmacokinetics of fentanyl and alfentanil in patients. Anesthesiology 88:657-667 (1998).
S. Björkman, D. R. Wada, B. M. Berling, and G. Benoni. Prediction of the disposition of midazolam in surgical patients by a physiologically based pharmacokinetic model. J. Pharm. Sci. 90:1226-1241 (2001).
N. R. Davis and W. W. Mapleson. A physiological model for the distribution of injected agents, with special reference to pethidine. Br. J. Anaesth. 70:248-258 (1993).
H. A. El-Masri and C. J. Portier. Physiologically based pharmacokinetic model of primidone and its metabolites phenobarbital and phenylethylmalonamide in humans, rats, and mice. Drug Metab. Dispos. 26:585-594 (1998).
P. Poulin, K. Schoenlein, and F. P. Theil. Prediction of adipose tissue:plasma partition coefficients for structurally unrelated drugs. J. Pharm. Sci. 90:436-447 (2001).
I. A. Nestorov, L. J. Aarons, P. A. Arundel, and M. Rowland. Lumping of whole-body physiologically based pharmacokinetic models. J. Pharmacokin. Biopharm. 26:21-46 (1998).
S. Björkman. Prediction of the volume of distribution of a drug: which tissue:plasma partition coefficients are needed? J. Pharm. Pharmacol. 54:1237-1245 (2002).
R. J. Hudson, I. R. Thomson, J. E. Cannon, R. M. Friesen, and R. C. Meatherall. Pharmacokinetics of fentanyl in patients undergoing abdominal aortic surgery. Anesthesiology 64:334-338 (1986).
F. Redke and S. Björkman. Pharmacokinetics of pethidine in patients with postoperative fever [abstract]. Eur. J. Pharm. Sci. 8:xix(1999).
S. Björkman, D. R. Stanski, H. Harashima, R. Dowrie, S. R. Harapat, D. R. Wada, and W. F. Ebling. Tissue distribution of fentanyl and alfentanil in the rat cannot be described by a blood flow limited model. J. Pharmacokin. Biopharm. 21:255-279 (1993).
S. Björkman, D. R. Wada, D. R. Stanski, and W. F. Ebling. Comparative physiological pharmacokinetics of fentanyl and alfentanil in rats and humans based on parametric single-tissue models. J. Pharmacokin. Biopharm. 22:381-410 (1994).
S. Björkman, D. R. Stanski, D. Verotta, and H. Harashima. Comparative tissue concentration profiles of fentanyl and alfentanil in humans predicted from tissue/blood partition data obtained in rats. Anesthesiology 72:865-873 (1990).
J. L. Gabrielsson, P. Johansson, U. Bondesson, M. Karlsson, and L. K. Paalzow. Analysis of pethidine disposition in the pregnant rat by means of a physiological flow model. J. Pharmacokin. Biopharm. 14:381-395 (1986).
M. P. Persson, P. Hartvig, L. Wiklund, and L. Paalzow. Pulmonary disposition of pethidine in postoperative patients. Br. J. Clin. Pharmacol. 25:235-241 (1988).
T. H. Hallynck, H. H. Soep, J. A. Thomis, J. Boelaert, R. Daneels, and L. Dettli. Should clearance be normalized to body surface or to lean body mass? Br. J. Clin. Pharmacol. 11:523-526 (1981).
L. R. Williams and R. W. Leggett. Reference values for resting blood flow to organs of man. Clin. Phys. Physiol. Meas. 10:187-217 (1989).
S. Björkman and F. Redke. Clearance of fentanyl, alfentanil, methohexitone, thiopentone, and ketamine in relation to estimated hepatic blood flow in several animal species: application to prediction of clearance in man. J. Pharm. Pharmacol. 52:1065-1074 (2000).
D. R. Wada, D. R. Stanski, and W. F. Ebling. A PC-based graphical simulator for physiological pharmacokinetic models. Comp. Meth. Progr. Biomed. 46:245-255 (1995).
W. F. Ebling, D. R. Wada, and D. R. Stanski. From piecewise to full physiologic pharmacokinetic modeling: Applied to thiopental disposition in the rat. J. Pharmacokin. Biopharm. 22:259-292 (1994).
A. Tsuji, K. Nishide, H. Minami, E. Nakashima, T. Terasaki, and T. Yamana. Physiologically based pharmacokinetic model for cefazolin in rabbits and its preliminary extrapolation to man. Drug Metab. Disp. 13:729-739 (1985).
O. Nagata, M. Murata, H. Kato, T. Terasaki, H. Sato, and A. Tsuji. Physiological pharmacokinetics of a new muscle-relaxant, inaperisone, combined with its pharmacological effect on blood flow rate. Drug Metab. Disp. 18:902-910 (1990).
L. B. Sheiner and S. L. Beal. Some suggestions for measuring predictive performance. J. Pharmacokin. Biopharm. 9:503-512 (1981).
G. Wu. Calculating predictive performance: a user's note. Pharmacol. Res. 31:393-399 (1995).
P. M. Vermeulen, J. G. C. Lerou, R. Dirksen, L. H. D. J. Booij, and G. F. Borm. Repeated enflurane anesthetics and model predictions: a study of the variability in the predictive performance measures. Br. J. Anaesth. 79:488-496 (1997).
N. Shibata, W. Gao, H. Okamoto, T. Kishida, K. Iwasaki, Y. Yoshikawa, and K. Takada. Drug interactions between HIV protease inhibitors based on physiologically-based pharmacokinetic model. J. Pharm. Sci. 91:680-689 (2002).
F. Y. Bois, T. J. Woodruff, and R. C. Spear. Comparison of three physiologically based pharmacokinetic models of benzene disposition. Toxicol. Appl. Pharmacol. 110:79-88 (1991).
P. Poulin and F.-P. Theil. Prediction of pharmacokinetics prior to in vivo studies. II. Generic physiologically based pharmacokinetic models of drug disposition. J. Pharm. Sci. 91:1358-1370 (2002).
R. K. Verbeeck, R. A. Branch, and G. R. Wilkinson. Meperidine disposition in man: influence of urinary pH and route of administration. Clin. Pharmacol. Ther. 30:619-628 (1981).
K. Chan, J. Tse, F. Jennings, and M. L. E. Orme. Influence of urinary pH on pethidine kinetics in healthy volunteer subjects. Meth. Find. Exptl. Clin. Pharmacol. 7:245-251 (1985).
L. E. Mather and P. J. Meffin. Clinical pharmacokinetics pethidine. Clin. Pharmacokin. 3:352-368 (1978).
B. E. Dahlström, L. K. Paalzow, C. Lindberg, and C. Bogentoft. Pharmacokinetics and analgesic effect of pethidine (meperidine) and its metabolites in the rat. Drug Metab. Disp. 7:108-112 (1979).
W. G. Kramer, D. R. Gross, and C. Medlock. Contribution of the lung to total body clearance of meperidine in the dog. J. Pharm. Sci. 74:569-571 (1985).
B. Ranheim, J. Høiset, T. Framstad, T. E. Horsberg, J. U. Skaare, and N. E. Søli. Pharmacokinetics of pethidine in pigs following intravenous, intramuscular, and subcutaneous administration. J. Vet. Pharmacol. Ther. 21:491-493 (1998).
R. N. Upton, L. E. Mather, and W. B. Runciman. The in vitro uptake and metabolism of lignocaine, procainamide, and pethidine by tissues of the hindquarters of sheep. Xenobiotica 21:1-12 (1991).
J. C. Scott, K. V. Ponganis, and D. R. Stanski. EEG quantitation of narcotic effect: the comparative pharmacodynamics of fentanyl and alfentanil. Anesthesiology 62:234-241 (1985).
J. C. Scott and D. R. Stanski. Decreased fentanyl and alfentanil dose requirements with age. A simultaneous pharmacokinetic and pharmacodynamic evaluation. J. Pharmacol. Exp. Ther. 240:159-166 (1987).
H. J. M. Lemmens, J. B. Dyck, S. L. Shafer, and D. R. Stanski. Pharmacokinetic–pharmacodynamic modeling in drug development: application to the investigational opioid trefentanil. Clin. Pharmacol. Ther. 56:261-271 (1994).
C. C. Hug. Lipid solubility, pharmacokinetics, and the EEG: are you better off today than you were four years ago? Anesthesiology 62:221-226 (1985).
R. N. Upton, G. L. Ludbrook, E. C. Gray, and C. Grant. The cerebral pharmacokinetics of meperidine and alfentanil in conscious sheep. Anesthesiology 86:1317-1325 (1997).
G. L. Qiao and K. F. Fung. Pharmacokinetic–pharmacodynamic modelling of meperidine in goats (II): modelling. J. Vet. Pharmacol. Ther. 17:127-134 (1994).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Björkman, S. Reduction and Lumping of Physiologically Based Pharmacokinetic Models: Prediction of the Disposition of Fentanyl and Pethidine in Humans by Successively Simplified Models. J Pharmacokinet Pharmacodyn 30, 285–307 (2003). https://doi.org/10.1023/A:1026194618660
Issue Date:
DOI: https://doi.org/10.1023/A:1026194618660