Abstract
Purpose. The pharmacokinetic properties of methotrexate (MTX) in the plasma and synovial fluid (SF) after bolus IV and topical administration were studied in dogs to assess the feasibility of topical delivery of MTX for the treatment of rheumatoid arthritis.
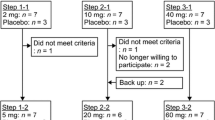
Methods. A MTX gel in Poloxamer 407 containing an absorption enhancer was formulated and topically applied on the elbow and stifle joints of dogs. SF was collected by inserting a needle with syringe into the joint space. Drug concentrations in the plasma, SF and muscle tissues were determined using a HPLC method with fluorimetric detection.
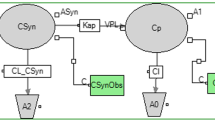
Results. Peak MTX concentrations in SF occurrred at 38 ± 5 min following bolus IV dose, indicating the presence of a substantial diffusion barrier between the plasma and SF. The plasma/SF concentration ratios of 1.16 ± 0.25 were maintained after the attainment of distribution equilibrium between the two compartments. The t1/2 values in the plasma (11.2 ± 1.2 hr) and SF (12.7 ± 3.7 hr) were similar during the elimination phase, while the MRT in SF (3.24 ± 0.21 hr) was longer than that in plasma (2.56 ± 0.20 hr), probably due to the slow distribution of MTX to SF. After topical dose, MTX concentrations in plasma reached the steady state at ~4 hr, lasting for ~20 hr.The bioavailability of MTX from the gel was 11.8 ± 3.3% of the applied dose, but muscle tissues beneath the gel application site had significantly higher levels of MTX than untreated muscle tissues. There was no statistical difference in SF concentrations of MTX between drug treated and untreated joints 24 hr after topical dose.
Conclusions. Topical delivery of MTX in a hydrophilic gel achieved a sustained C/t profile in plasma and higher drug levels in muscle tissues underneath the dosing site, implicating the potential therapeutic value of the topical formulation.
Methods. A MTX gel in Poloxamer 407 containing an absorption enhancer was formulated and topically applied on the elbow and stifle joints of dogs. SF was collected by inserting a needle with syringe into the joint space. Drug concentrations in the plasma, SF and muscle tissues were determined using a HPLC method with fluorimetric detection.
Results. Peak MTX concentrations in SF occurrred at 38 ± 5 min following bolus IV dose, indicating the presence of a substantial diffusion barrier between the plasma and SF. The plasma/SF concentration ratios of 1.16 ± 0.25 were maintained after the attainment of distribution equilibrium between the two compartments. The t1/2 values in the plasma (11.2 ± 1.2 hr) and SF (12.7 ± 3.7 hr) were similar during the elimination phase, while the MRT in SF (3.24 ± 0.21 hr) was longer than that in plasma (2.56 ± 0.20 hr), probably due to the slow distribution of MTX to SF. After topical dose, MTX concentrations in plasma reached the steady state at ~4 hr, lasting for ~20 hr.The bioavailability of MTX from the gel was 11.8 ± 3.3% of the applied dose, but muscle tissues beneath the gel application site had significantly higher levels of MTX than untreated muscle tissues. There was no statistical difference in SF concentrations of MTX between drug treated and untreated joints 24 hr after topical dose.
Conclusions. Topical delivery of MTX in a hydrophilic gel achieved a sustained C/t profile in plasma and higher drug levels in muscle tissues underneath the dosing site, implicating the potential therapeutic value of the topical formulation.
Similar content being viewed by others
REFERENCES
R. Segal, M. Yaron, and B. Tartakovsky. Methotrexate: mechanism of action in rheumatoid arthritis. Semin. Arthritis Rheum. 20:190–200 (1990).
S. Hirata, T. Matsubara, R. Saura, H. Tateishi, and K. Hirohata. Inhibition of in vitro vascular endothelial cell proliferation and in vivo neovascularization by low-dose methotrexate. Arthritis Rheum. 32:1065–1073 (1989).
B. Haraoui, J.P. Pelletier, J.M. Cloutier, M.P. Faure, and J. Martel-Pelletier. Synovial membrane histology and immunopathology in rheumatoid arthritis and osteoarthritis: In vivo effects of antirheumatic drugs. Arthritis Rheum. 34:153–163 (1991).
D. Mathers and A.S. Russell. Methotrexate. In Dixon & Furst (eds.) Second-line Agents in the Treatment of Rheumatic Diseases. Marcel Dekker, New York, 1992, pp. 288–289.
W.J. Wallis and P.A. Smikin. Antirheumatic drug concentrations in human synovial fluid and synovial tissue: observations on extravascular pharmacokinetics. Clin. Pharmacokinet. 8:496–522 (1983).
J.M. Kremer and J.K. Lee. The safety and efficacy of the use of methotrexate in long-term therapy for rheumatoid arthritis. Arthritis Rheum. 29:822–831 (1986).
T.W. Rooney and D.E. Furst. Methotrexate. In McCarty and Koopman (Eds.), Arthritis and Allied Conditions, 12th ed. Vol. 1, Lea and Febiger, Philadelphia. 1993, pp.621–636.
N.J. Olsen, L.F. Callaghan and T. Pincus. Immunologic studies of rheumatoid arthritis patients treated with methotrexate. Arthritis Rheum. 30:481–488 (1987).
I.R. Schmolka. Artificial skin I. preparation and properties of pluronic F-127 gels for treatment of burns. J. Biomed. Mater. Res. 6:571–582 (1972).
G.W. Lu and H.W. Jun. Determination of trace methotrexate and 7-OH-methotrexate in plasma by high-performance liquid chromatography with fluorimetric detection. J. Liq. Chromatogr. 18:155–171 (1995).
R.A. Herman, P. Veng-Pedersen, J. Hoffman, R. Koehnke, and D.E. Furst. Pharmacokinetics of low-dose methotrexate in rheumatoid arthritis patients. J. Pharm. Sci. 78:165–171 (1989).
D.A. O'keefe, R.L. Capizzi, and S.A. Rudnick. Methotrexate cytotoxicity for L5178Y/ASN lymphoblasts: relationship of dose and duration of exposure to tumor cell viability. Cancer Res. 42:1641–1647 (1982).
W.S. Wilke, J.M. Kremer, A.M. Mackenzie, A.M. Segal and D.J. Mazanec. Methotrexate and rheumatoid arthritis. Ann. Internal Med. 110:88–89 (1989).
R.L. Woods and J.J. Smolich. Regional blood flow effects of ANP in conscious dogs: preferential gastrointestinal vasoconstriction. Am. J. Physiol. 261:H1961–1969 (1991).
P. Singh and M.S. Roberts. Skin permeability and local tissue concentrations of nonsteroidal anti-inflammatory drugs after topical application. J. Pharmacol. Exp. Therap. 268:144–151 (1994).
J.L. Rabinowitz, E.S. Feldman, A. Weinberger, and H.R. Schumacher. Comparative tissue absorption of oral 14C-aspirin and topical triethanolamine 14C-salicylate in human and canine knee joints. J. Clin. Pharmacol. 22:42–48 (1982).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Lu, G.W., Jun, H.W., Dzimianski, M.T. et al. Pharmacokinetic Studies of Methotrexate in Plasma and Synovial Fluid Following IV Bolus and Topical Routes of Administration in Dogs. Pharm Res 12, 1474–1477 (1995). https://doi.org/10.1023/A:1016231303689
Issue Date:
DOI: https://doi.org/10.1023/A:1016231303689