CVD is the first leading cause of death in the world. As a major risk factor for CVD, hypertension contributed to 10·3 million deaths and 208 million disability-adjusted life years in 2013(Reference Campbell, Khalsa and Lackland1). In 2013, almost 300 million Chinese adults had hypertension, which accounted for 2·5 million deaths and 15 % of total disability-adjusted life years(Reference Li, Yang and Wang2,Reference Forouzanfar, Alexander and Anderson3) .
Epidemiological and clinical studies showed that excessive salt consumption is positively associated with the incidence of hypertension(Reference Forman, Scheven and de Jong4,Reference Subasinghe, Arabshahi and Busingye5) . Besides, salt consumption increases the relative risk of CHD(Reference He, Li and Macgregor6,Reference Narula, Mancia and McKee7) , stroke(Reference Li, Huang and Jin8) and gastric cancer(Reference D’Elia, Rossi and Ippolito9). In addition, a high dietary Na:K ratio could contribute to an increased risk of cardiovascular events(Reference O’Donnell, Mente and Rangarajan10). In contrast, restricting salt intake can lower the blood pressure (BP) of hypertensive patients and also reduce the risk of hypertension and cardiovascular events(Reference He and MacGregor11). Excessive salt intake was reported to be a modifiable determinant of hypertension. Reducing salt intake is well known to have many beneficial effects and is the most cost-efficient measure to prevent CVD(Reference Schorling, Niebuhr and Kroke12–Reference Watkins, Olson and Verguet14). An amount of 5 g/d is recommended by the WHO as the upper limit for daily salt intake(15). Data available in China show that the average salt intake of residents ranges from 10 to 20 g/d(Reference Chen, Guo and Ma16–Reference Okuda, Stamler and Brown18), much higher than the WHO recommendation. However, evidence of daily salt intake among inhabitants in Chaoshan region is absent.
The Chaoshan region is located in the east of Guangdong Province in China, bordering the sea, which is one of the famous hometowns of overseas Chinese. Over hundreds of years, people from this area have emigrated and most of them still retain the customs and habits of their ancestors. People living in this region mainly speak the Teochew and Hakka dialects. Besides, they have distinct dietary habits compared with people in other regions of China(Reference Yi, Tan and Zhao19,Reference Ding, Pi and Zhang20) . However, due to cultural differences, the dietary habits and lifestyles of people speaking different dialects in this region differ widely.
It is hard to gather data on salt intake and salt-related knowledge, attitudes as well as behaviours of the population in this region. One reason for this lack of information is the difficulty in assessing salt intake. The gold standard for measuring Na and K excretion is 24-h urine collection(Reference Nowson, Lim and Grimes21,Reference Wielgosz, Robinson and Mao22) . However, such a measurement is challenging for researchers and for participants to comply with, often leading to a difficulty in its implementation(Reference Wielgosz, Robinson and Mao22).
The current study aimed to estimate the baseline salt intake and Na:K ratio as well as knowledge, attitudes and behaviours related to salt intake among adults speaking the Teochew and Hakka dialects in the Chaoshan region by 24-h urinary Na and K excretion to provide information for preventing hypertension and CVD.
Methods
Study population and sampling
On the basis of cluster random sampling, we randomly selected one sub-district each from Jinping, Longhu and Chenghai districts of Shantou city, where we could find the most representative and largest number of Teochew speakers. However, most of Teochew–Hakka and Hakka speakers mainly reside in the Jiexi district of Jieyang city, and that is the reason why we randomly selected two sub-districts from Teochew–Hakka speaking sub-districts and one from Hakka speaking sub-districts in the Jiexi district. The sample sizes of these three dialect groups were comparable. Subsequently, we investigated all residents in the selected sub-districts according to inclusion and exclusion criteria, and informed consent was obtained from March 2016 to June 2017. The response rate of these three dialects reached 89, 86 and 88 %, respectively.
All participants should be aged ≥18 years, of Han nationality and not immigrants; all had resided in the region for at least 10 years before this investigation. Whereas pregnant or breastfeeding females, very heavy manual workers, people who worked in high-temperature environments, professional athletes and people who used any diuretic drug for the last 2 weeks or had other severe diseases were excluded. A total of 506 participants aged 18–80 years were recruited in our study. During the collection and determination of 24-h urine samples, ninety-one participants were excluded; among them, fifty-seven had more than one urine sample not collected during the 24 h or the total volume of the 24-h urine sample was <500 ml; thirty-two had a creatinine level <4 mmol (female) or <6 mmol (male); and two had renal impairment. Finally, 415 participants were included in the analysis.
The required sample size was determined by assuming that the difference of mean salt intake between dialect groups was about 3 g/d(Reference Tan, He and Wang23) and their standard deviation of salt intake was equally 5·87 g/d(Reference Wen, Zhou and Stamler24). Then a sample size of eighty-one participants in each group would be needed to detect a significant difference occurring with a two-sided α = 0·05 and β = 0·10. Making a 20 % allowance of non-participation and incomplete samples, at least ninety-seven of each dialect group was needed.
Data collection and anthropometric measurements
All information was obtained using a questionnaire that included general characteristics (age, education, occupation, smoking, health status, etc.) as well as knowledge, attitudes and behaviours related to salt intake. We focused on the behaviour of salt usage, which included dietary characteristics and habits.
Anthropometric measurements including height, weight, waist and hip measurements and BP were taken following standardised methods. BMI (kg/m2) was calculated based on height and weight. We measured BP using a mercury sphygmomanometer three times with an interval of at least 2 min in the same arm, and averages were calculated. Participants were defined as hypertensive if the measured systolic BP (SBP) was ≥140 mmHg and/or diastolic BP (DBP) was ≥90 mmHg, or if they self-reported the use of anti-hypertensive medications within 2 weeks(Reference Mancia, Fagard and Narkiewicz25).
Collection of 24-h urine sample
We collected 24-h urine samples after questionnaire administration and anthropometric measurements. We distributed a container (4 l) to each subject and taught them how to collect 24-h urine samples. In brief, 24-h urine sampling included the first urination in the morning and all other urinations until the first urination the next morning. Participants were asked to record the beginning and end time of urine collection and any missed urine collection during the 24-h period. The participants came to the community centre the next morning with the containers, and we measured and recorded the volumes of 24-h urine. A 3-ml urine sample from each participant was sent to the laboratory of First Affiliated Hospital of Shantou University Medical College for measuring Na, K and creatinine under freezing after homogenisation of the entire 24-h urine sample, and 20 ml urine was stored at –20°C in a refrigerator immediately. Urinary Na and K was determined using ion-selective electrodes, and urinary creatinine was determined by the Jaffe kinetic method; all analyses were performed with the Backman Coulter LX20 automatic analyser. A 1 mol urinary Na was equal to 58·42 g salt intake (salt (g) = mol Na × 23 × 2·54; 1 mol Na = 23 g Na; 1 g Na = 2·54 g NaCl)(Reference Nowson, Lim and Grimes21).
Statistical analysis
A database was established using Epidata 3·0, and data were analysed using SPSS 21·0 (SPSS Inc.). Shapiro–Wilk test was used to test the normality of distribution of continuous variables. Continuous variables were described as mean and sd (normally distributed data), or median and interquartile range (non-normally distributed data). Categorical variables were described with numbers and percentages or ratio. Student’s t test and ANOVA (normally distributed data), or Mann–Whitney U test and Kruskal–Wallis H test (non-normally distributed data) were used for comparing 24-h urinary Na level or Na:K ratio in different groups. If ANOVA was statistically significant, the SNK test was used for a comparison between the two groups. χ 2 test was used to compare salt-related knowledge, attitudes and behaviours in different groups, and Spearman correlation was used to analyse the correlation between 24-h urinary Na level and BP. A multiple linear regression analysis was used to identify the risk factors of 24-h urinary Na level and Na:K ratio by dialect groups. Independent variables included in the models were age, sex (male, female), BMI, hypertension, family history of hypertension, education level (illiterate or primary school, middle school, above middle school), marital status (married, unmarried), smoking (non-smoker, former/current smoker), income (≤3000, >3000 Chinese Yuan/month) and waist–hip ratio (WHR). Two-sided tests were performed, and P < 0·05 was considered statistically significant.
Results
Basic characteristics
Among the 415 enrolled participants, 171 (41·2 %) spoke the Teochew dialect, 131 (31·6 %) the Teochew–Hakka dialect and 113 (27·2 %) the Hakka dialect. The mean age was 59·70 (sd 14·50) years. The general characteristics of participants are shown in Table 1. Hakka dialect speakers had higher WHR, BP and hypertension prevalence compared with Teochew dialect speakers (all P < 0·05).
Table 1 General characteristics of participants speaking different dialects

WHR, waist–hip ratio, BP, blood pressure.
* P < 0·05, Teochew v. Teochew–Hakka speakers.
† P < 0·05, Teochew v. Hakka speakers.
‡ P < 0·05, Teochew–Hakka v. Hakka speakers.
24-h urinary sodium level and related indexes across participants speaking different dialects
The mean 24-h urinary Na and K and Na:K ratio was 149·88, 40·33 mmol and 3·48, respectively, and the mean daily salt intake was 8·76 g/d. The 24-h urinary Na level was higher for Hakka than Teochew speakers (173·28 v. 123·00 mmol; P < 0·05). In contrast, the mean 24-h urinary K level was lower for Hakka than Teochew speakers (36·00 v. 40·63 mmol; P < 0·05). The mean Na:K ratio was higher for Hakka than Teochew–Hakka and Teochew speakers (all P < 0·001) and was significantly higher for Teochew–Hakka than Teochew speakers (P = 0·004). The salt intake of adults who spoke the Teochew, Teochew–Hakka and Hakka dialects was 7·19 (interquartile range 5·29–10·17), 9·03 (interquartile range 6·62–11·54) and 10·12 (interquartile range 7·61–12·82) g/d, respectively, with significant differences between Teochew and Teochew–Hakka speakers and between Teochew and Hakka speakers (both P < 0·05). Besides, the daily salt intake in >85·0 % of participants was >5 g and for 36·4 % was >10 g. Only 14·0 % of the population had a Na:K ratio ≤2, and for 22·9 %, the ratio was >5 (Table 2).
Table 2 Comparison of 24-h urinary sodium and relative indexes for participants speaking different dialects
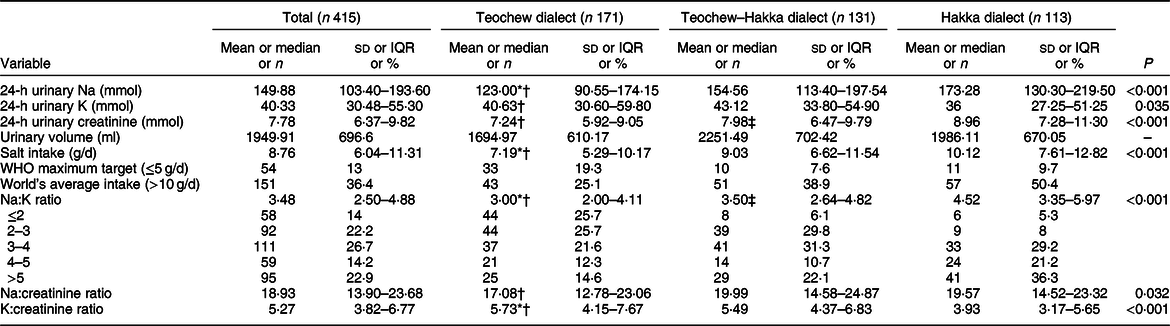
IQR, interquartile range. *P < 0·05, Teochew v. Teochew–Hakka speakers.
† P < 0·05, Teochew compared with Hakka dialect adults.
‡ P < 0·05, Teochew–Hakka compared with Hakka dialect adults.
Factors associated with 24-h urinary sodium level and sodium:potassium ratio
After adjusting for age, sex, BMI, education and income, 24-h urinary Na level was associated with SBP (β = 1·01, 95 % CI 0·30, 1·72, P = 0·006) and DBP (β = 1·52, 95 % CI 0·42, 2·61, P = 0·007) in Teochew, and SBP (β = 0·96, 95 % CI 0·07, 1·86, P = 0·035) in Teochew–Hakka. The Na:K ratio was associated with SBP (β = 0·03, 95 % CI 0·01, 0·06, P = 0·002) and DBP (β = 0·04, 95 % CI 0·01, 0·07, P = 0·036) in Teochew, and SBP (β = 0·02, 95 % CI 0·01, 0·04, P = 0·036) in Teochew–Hakka. However, hypertension was associated with the Na:K ratio (β = 0·86, 95 % CI 0·10, 1·61, P = 0·026) only in Hakka (Table 3).
Table 3 Associations of 24-h urinary sodium and sodium:potassium ratio with BP and prevalence of hypertension by multiple linear regressions
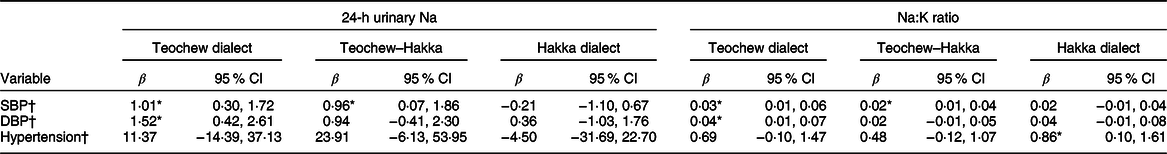
SBP, systolic blood pressure; DBP, diastolic blood pressure.
* P < 0·05.
† Adjusted for age, sex, BMI, education, income.
A multiple linear regression analysis showed 24-h urinary Na level to be associated with age (β = –1·00, 95 % CI –1·77, –0·22, P = 0·012), BMI (β = 4·60, 95 % CI 1·40, 7·80, P = 0·005) and WHR (β = 185·48, 95 % CI 15·42, 355·54, P = 0·033) in Teochew, with income (β = 34·18, 95 % CI 1·85, 66·51, P = 0·038) in Teochew–Hakka and education (β = –25·10, 95 % CI –46·67, –3·54, P = 0·023) in Hakka. On the other hand, a higher Na:K ratio was associated with both hypertension (β = 0·71, 95 % CI 0·02, 1·40, P = 0·043) and smoking (β = 0·90, 95 % CI 0·07, 1·73, P = 0·033) in Hakka while with lower education (β = –0·48, 95 % CI –0·91, –0·05, P = 0·028) in Teochew (Table 4). BMI was weakly but positively correlated with both 24-h urinary Na level (r s = 0·244, P < 0·001) and Na:K ratio (r s = 0·124, P = 0·011). The 24-h urinary Na level was weakly but positively correlated with both SBP and DBP (r s = 0·215, 0·258) as was Na:K ratio (r s = 0·238, 0·276) (all P < 0·001) (see online supplementary material, Supplemental Fig. S1).
Table 4 Factors associated with 24-h urinary sodium and sodium:potassium ratio by multiple linear regressions
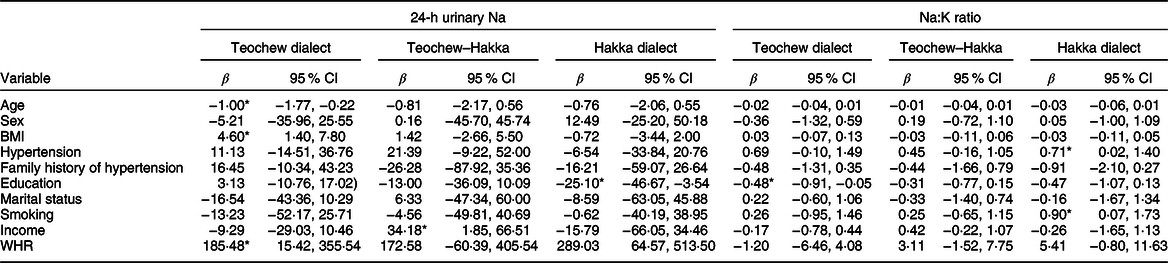
WHR, waist–hip ratio.
* P < 0·05.
Knowledge, attitudes and behaviours related to salt intake
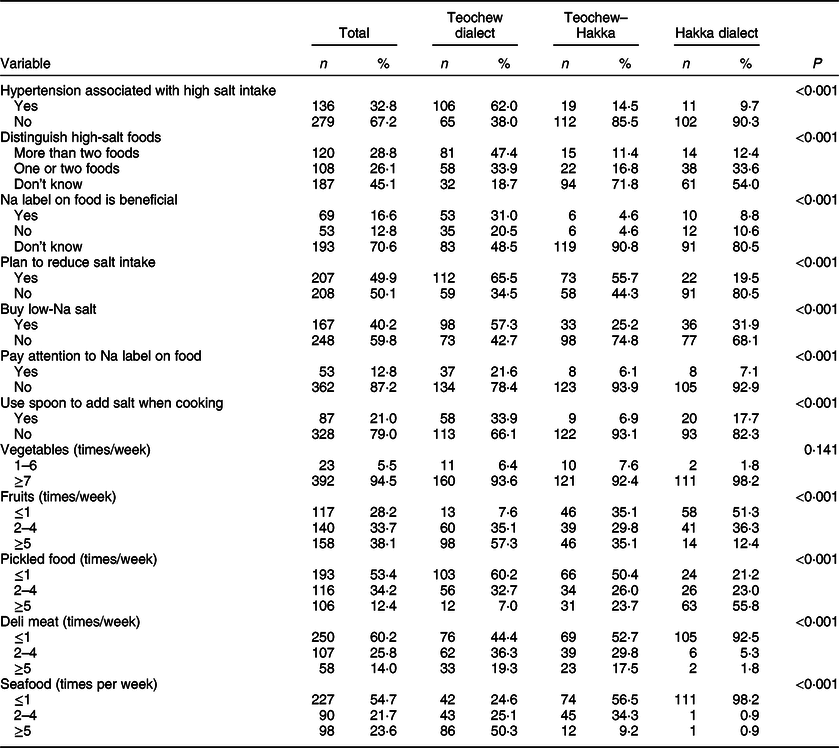
Only 16·6 % of the participants believed they consumed too much salt (data not shown). Among all participants, more than a half could not identify the relation between hypertension and high salt intake. Also, <13 % of participants paid attention to Na label on food packages, and nearly 21 % residents used a spoon to add salt when cooking. Approximately 50 % of participants aimed to reduce their salt intake. Significant differences were found in knowledge, attitudes and behaviours related to salt intake among different dialect speakers (all P < 0·001). Moreover, the consumption of fruits, pickled food, deli meat and seafood differed (all P < 0·001) (Table 5).
Table 5 Knowledge, attitudes and behaviours related to salt intake in participants speaking different dialects
Discussion
We estimated salt intake and evaluated the knowledge and self-awareness about salt intake among people speaking the Teochew, Teochew–Hakka and Hakka dialects in the Chaoshan region of southern China. Salt intake differed between Teochew and Teochew–Hakka speakers and between Teochew and Hakka speakers. The Na:K ratio differed significantly among the dialects. Knowledge and self-awareness about salt intake were poor in this population.
Studies of salt intake are limited in southern China. Moreover, most previous studies might have underestimated salt intake in this population because some sources of Na intake were not included, such as snacks and deli meats. Some studies showed that >75 % of participants reported low Na intake, and the consistency was low between self-reported Na intake and actual Na intake(Reference Chang, Park and Chung26–Reference Zhang, Guo and Seo28), which suggests that individuals’ self-reported outcomes might not reflect their actual daily salt intake. Our study evaluated daily salt intake of the population in the Chaoshan region of southern China using the method of 24-h urine collection(Reference McLean29).
Our study found that the mean salt intake of the Chaoshan population is much higher than 5 g/d, the upper limit recommended by the WHO(15). The proportion of no more than 5 g/d was only 13 %. The average salt intake was higher than that of residents 18–75 years old in northern Greece (4·4 g/d)(Reference Vasara, Marakis and Breda30) but lower than that of residents in Korea(Reference Lee, Kim and Oh31) (13·2 g/d), Japan(Reference Uechi, Sugimoto and Kobayashi32) (11·0 g/d), Chinese people in the INTERMAP study(Reference Okuda, Stamler and Brown18) (13·3 g/d) and other studies. For example, in the Yantai city of China, the average intake was 12·8 g/d in ninety-eight males and 10·8 g/d in ninety-three females 18–69 years of age(Reference Xu, Wang and Chen33). Peng et al. (Reference Peng, Li and Wang17) reported a salt intake of 16·0 g/d in 120 people 35–70 years of age in the Shanxi province of China. Climate and diet habits might influence salt intake in southern and northern China.
Our results showed that BMI is positively correlated with 24-h Na intake, which is consistent with the results of Yan et al. in Chinese adults(Reference Yan, Bi and Tang34). Furthermore, Chakma et al. (Reference Chakma, Kavishwar and Sharma35) reported excessive salt intake and high BMI to be associated with an increased risk of hypertension, which indicates that limiting both Na intake and weight gain may be effective ways to prevent high BP. We observed significant, although weak, positive correlations between 24-h urinary Na and BP as well as Na:K ratio and BP, which agrees with other research(Reference Hedayati, Minhajuddin and Ijaz36,Reference Mente, O’Donnell and Rangarajan37) .
We found dialect to be associated with the level of salt intake, much higher in Hakka and Teochew–Hakka than Teochew speakers. People speaking the Teochew dialect, the predominant inhabitants of the Chaoshan area, are mainly the descendants of northcentral Chinese Han people. Their ancestors migrated to the Chaoshan area from Fujian, because of wars and famine during the Qin Dynasty (216–207 BC) and Han Dynasty (206 BC–220 AD)(Reference Wang, Wang and Cheng38,Reference Liu, Huang and Huang39) , and ultimately settled in the cultivated coastal plains, which provided plenty of food such as cereals, vegetables and seafood. People speaking the Hakka dialect originated in the Yellow River basin of the Central Plain. From the Jin Dynasty (266–316 AD) to the Tong Dynasty (960–1297 AD), they moved to southern areas also because of wars. When they arrived in the Chaoshan area, people speaking the Teochew dialect had already settled in the rich plain area, so Hakka speakers had to settle in the mountain area where food was scarcer than in the plain area(Reference Wang, Wang and Cheng38,Reference Liu, Huang and Huang39) . This situation resulted in different lifestyles, customs and habits between these two groups. For instance, Teochew speakers prefer eating light food, while Hakka speakers in the Chaoshan area are likely to preserve food using salt because of previous lack of food. In the long term, they even thought that salt could give food flavour and bring out the best in food. Moreover, people speaking Teochew drink Kongfu tea prepared by brewing dried tea leaves with hot water(Reference Yi, Tan and Zhao19), whereas Hakka speakers usually drink ‘grinding tea’ prepared by brewing dried tea leaves with salt, rice, sesame seeds, orange peel, other raw materials and hot water. All of these habits led to a high level of salt intake in Hakka speakers. Interestingly, the salt intake of Teochew–Hakka was intermediate between that of Teochew and Hakka. It was probably a result of the unique culture of Teochew–Hakka speakers that blends the lifestyle and dietary patterns of Teochew and Hakka.
In this survey, fewer people had a Na:K ratio <1·0, the target recommended by the WHO(40), and only 14 % of participants had a ratio <2·0. Dietary K partly offsets the effect of high dietary Na intake. Meanwhile, we found a correlation between Na:K ratio and hypertension for Hakka speakers, because they prefer eating salty food with a strong taste and that they do not eat much fruit and vegetables, a factor that could easily lead to excessive Na and insufficient K intake. A high Na and low K diet is one of the major risk factors of hypertension and CVD(Reference Judd, Aaron and Letter41). It is probably related to increased IL-6 levels caused by a high-salt diet and high Na:K ratio(Reference Zhao, Zhang and Zhang42). Along with dialect and hypertension, education is the main determining factor of Na:K ratio in our study. A previous study in New York has found a lower Na:K ratio in people with higher than lower educational attainment(Reference Yi, Curtis and Angell43). This finding suggests that residents should pay attention to the balance of Na and K in their diet, and health education plays an important role in controlling BP of residents in communities.
A population study has found that dietary habits are healthier in people with a high dietary self-efficacy(Reference Sheeran, Maki and Montanaro44). Only a small proportion of our respondents recognised that they ate too much salt, and one-quarter knew the recommended maximum level of salt intake. The Chaoshan region is located in the coastal area, so people would easily ignore their salt intake from potential foods, such as seafood and spices, which might explain why most residents thought their salt intake was moderate or less than the recommended level. Studies have found that residents’ awareness of salt control could help reduce their salt intake(Reference Zhang, Xu and Ma45). Overall, 16·6 % of our participants declared that food labels are helpful in choosing low-salt food, whereas only 12·8 % read these labels when buying, which was lesser compared with the results of Claro et al. (Reference Claro, Linders and Ricardo46). Of note, Nasreddine et al. (Reference Nasreddine, Akl and Al-Shaar47) have found that nearly half the consumers do not change their idea of choosing high-salt foods even if the salt content is marked on the food bag. A ‘traffic light’ system is widely used in UK; the system marks packages with different colours (red, yellow, green) to distinguish the amount of salt or Na in food. It significantly improved the understanding of nutritional information and enhanced the awareness of choosing healthy foods among consumers compared with the traditional labelling method(Reference Sonnenberg, Gelsomin and Levy48).
There are two strengths in the current study. First, we provided the first epidemiologic data for salt intake in community residents in the Chaoshan region of southern China. Second, 24-h urine collection combined with a qualitative questionnaire was used to evaluate the level of salt intake in a relatively large sample of community residents, instead of either a dietary survey or spot urine sampling alone.
Because of inconvenience in the respondents carrying the urine container, 24-h urine collection is challenging. A limitation of the study was that we collected urine on only a single 24-h period from each participant, whose results may be less accurate than a continuous 24-h sampling because of day-to-day variations. However, most participants were older and remained at home, whereas young people were unable to meet 24-h urine collection because they may have been at work. In addition, the age of people speaking different dialects was not balanced, so the univariate analysis was affected by age. However, during the multivariable analysis, we adjusted for age, so we mainly refer to the results of multiple linear regressions. A larger sample whose age and sex are balanced should be investigated in the future.
Conclusions
The average daily salt consumption of the Chaoshan population, especially those speaking Teochew–Hakka and Hakka dialects, exceeded the upper limit recommended by the WHO. Residents’ knowledge and self-awareness as well as behaviours related to salt intake were poor. Local governments and medical institutions should take measures to improve the awareness and dietary lifestyles of residents with a view to decrease salt intake and increase potassium intake.
Acknowledgements
Acknowledgements: The authors thank Yanyun Ji and Hanming Chen for their support and cooperation in data collection. The authors thank Mrs Laura Smales (BioMedEditing, Toronto, Canada) for English language editing. Financial support: This work was supported by the Natural Science Foundation of Guangdong Province (grant no. 2014A030313472) and National Key R & D Program of China (grant no. 2016YFC1304000). Natural Science Foundation of Guangdong Province and National Key R & D Program of China had no role in the design, analysis or writing of this article. Conflict of interest: None. Authorship: Q.-Y.Z. designed the research; Q.-Y.Z., W.-Y.D., J.-X.J., X.-L.C., Y.W. and C.-Y.D. participated in data collection; W.-Y.D., F.C. and C.-Y.D. analysed the data; Q.-Y.Z., F.C. and W.-Y.D. wrote the article. Ethics of human subject participation: The current study was conducted according to the guidelines laid down in the Declaration of Helsinki, and all procedures involving study participants were approved by the Ethics Committee of Shantou University Medical College. Written informed consent was obtained from all subjects.
Supplementary material
For supplementary material accompanying this paper visit https://doi.org/10.1017/S136898001900507X










