Abstract
Purpose
The Morbidity and Mortality (M&M) report of the Scoliosis Research Society (SRS) has been collected since 1965 and since 1968 submission of complications has been required of all members. Since 2009, the SRS has collected information on death, blindness, and neurological deficit, with acute infection being added in 2012 and unintentional return to the operating room (OR) being added in 2017. In this report, we use the most recent data submitted to the SRS M&M database to determine the rate of neurological deficit, blindness, acute infection, unintentional return to the OR, and death, while also comparing this information to previous reports.
Methods
The SRS M&M database was queried for all cases from 2013 to 2020. The rates of death, vision loss, neurological deficit, acute infection, and unintentional return to the OR were then calculated and analyzed. The rates were compared to previously published data if available. Differences in complication rates between years were analyzed with Poisson regression with significance set at α = 0.05.
Results
The total number of cases submitted per year varied with a maximum of 49,615 in 2018 and a minimum of 40,464 in 2020. The overall reported complication rate from 2013 to 2020 was 2.86%. The overall mortality rate ranged from 0.09% in 2018 to 0.14% in 2015. The number of patients with visual impairment ranged from 4 to 13 between 2013 and 2015 (no data on visual impairment were collected after 2015). The overall infection rate varied from 0.95 in 2020 to 1.30% in 2015. When the infection rate was analyzed based on spinal deformity group, the neuromuscular scoliosis group consistently had the highest infection rate ranging from 3.24 to 3.94%. The overall neurological deficit rate ranged from 0.74 to 0.94%, with the congenital kyphosis and dysplastic spondylolisthesis groups having the highest rates. The rates of unintentional return to the OR ranged from 1.60 to 1.79%. Multiple groups showed a statistically significant decreasing trend for infection, return to the operating room, neurologic deficit, and death.
Conclusions
Neuromuscular scoliosis had the highest infection rate among all spinal deformity groups. Congenital kyphosis and dysplastic spondylolisthesis had the highest rate of neurological deficit postoperatively. This is similar to previously published data. Contrary to previous reports, neuromuscular scoliosis did not have the highest annual death rate. Multiple groups showed a statistically significant decreasing trend in complication rates during the reporting period, with only mortality in degenerative spondylolisthesis significantly trending upwards.
Level of evidence
Level III.
Similar content being viewed by others
Introduction
The Scoliosis Research Society (SRS) Morbidity and Mortality (M&M) database is an invaluable tool as it contains complications from a wide variety of procedures performed at a large number of institutions globally by mostly fellowship-trained spine surgeons. Since 2009, the SRS has collected information on death, blindness, and neurological deficit, with acute infection being added in 2012 and unintentional return to the operating room (OR) being added in 2017.
With the database containing a large number of cases from around the world, rates of rare events such as death and new neurological deficit can be determined over time in a real world setting. Ultimately, this allows those performing these procedures to better counsel patients on the risks and benefits of surgery.
A multitude of reports have been generated from the data collected by the SRS [1,2,3,4,5,6,7,8,9,10,11]. These studies include information regarding surgical complications for various pathologies, including adolescent idiopathic scoliosis, Scheuermann’s kyphosis, and thoracolumbar fixed sagittal plane deformity. Others have used the database to report on the complications of specific, frequently performed spinal procedures. In 2016, Burton et al. reported on the complications of the SRS M&M database from 2009 to 2012 [4]. In that time period, the authors found the overall mortality rate to range from 0.07 to 0.12%. Infection cases were first collected in the database in 2012 and the overall rate was 1.14%, with the highest rate occurring in patients with neuromuscular (NM) scoliosis (2.97%). Patients who had dysplastic spondylolisthesis and congenital kyphosis had the highest neurological deficit rates.
In this report, we use the most recent data submitted to the SRS M&M database to determine the rate of neurological deficit, blindness, acute infection, unintentional return to the OR, and death while also comparing this information to previous reports.
Materials and methods
Reporting on complications related to spinal deformity procedures is an annual requirement for membership of the SRS. Members may opt out of reporting complications by paying a $300 fee, with approximately 70% of members submitting their complete data. Submitted cases are classified into specific spinal deformity groups (Table 1). The total number of cases is derived by summing the cases in each group.
Primary complications recorded include death (within 21 days of surgery), neurological deficit, acute infection (within 90 days of surgery), vision change, and unintentional return to the OR (within 90 days of the index surgery). Information collected on vision change was halted after 2015 due to the consistently low number of patients with this complication each year. Data on acute infection were first reported in 2012 and data on unintentional return to the OR were first reported in 2017.
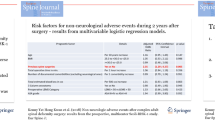
Overall complication rates and complication rates for each spinal deformity group were calculated. Statistical analysis was performed using R 4.1.0. Poisson regression with significance set at α = 0.05 was used to model how each tracked complication rate changed between years for each spinal deformity group. Expected decrease and 95% confidence intervals were reported for models with p values below 0.05.
Results
The total number of cases reported between 2013 and 2020 ranged from 40,464 in 2020 to 49,615 in 2018 (Tables 2, 3, 4, 5, 6). In all, 375,917 cases were submitted during that timeframe. The overall mortality rate ranged from 0.09% in 2018 to 0.14% in 2015. The highest group mortality rate was the other kyphosis group at 0.5%. These numbers generally align with what has been previously published [4]. From 2009 to 2012, the overall death rate ranged from 0.07 to 0.12%.
The overall infection rate varied from year to year as well. The year with the lowest infection rate was 2020 at 0.95% and the year with the highest infection rate was 2015 at 1.30%. The NM group had the highest infection rate, ranging from 3.24 to 3.94%. These data are in accordance with the study published by Burton et al., who reported an overall infection rate of 1.14% in 2012, with the NM scoliosis group having the highest infection rate at 2.97% [4].
The overall neurological deficit rate ranged from 0.71 to 0.94%, with congenital kyphosis and dysplastic spondylolisthesis patients having the highest rates. These rates appear to be slightly greater than the previously published data from 2009 to 2012 (0.44–0.79%) but the groups that had the highest rates of neurological deficits remained unchanged.
As stated above, vision loss rates were not recorded after 2015. However, from 2013 to 2015, visual loss rates were less than 0.1% in all groups, similar to previously published accounts. There were 13 cases of blindness reported in 2015 for a rate of 0.03%.
Data on unintentional return to the OR were first collected in 2017 during which the reported rate was 1.79%. This remained similar in the two subsequent years with reported unintentional return to the OR rates at 1.60% in 2018, 1.66% in 2019 and 1.61% in 2020.
Multiple groups were found to have a statistically significant decrease in complication rate from 2013 to 2020 (Supplement). In terms of infection, the groups that were found to have a statistically significant decreasing trend were the IS < 10 (p = 0.01), IS 10–18 (p = 0.05), isthmic spondylolisthesis (p = 0.01), degenerative spondylolisthesis (p < 0.01), and congenital kyphosis (p < 0.01) groups. Furthermore, there was an overall statistically significant decreasing trend in infection across all cases (p < 0.01). In addition, the neuromuscular scoliosis group (p = 0.03), other scoliosis group (p < 0.01), and all cases (p < 0.01) showed a statistically significant decreasing trend in neurologic deficit. Unintentional return to the OR was found to significantly decrease in the IS < 10 group (p = 0.02) and the other kyphosis group (p = 0.02). Deaths were found to significantly decrease in the other kyphosis group (p < 0.01). The only statistically significant increasing trends were vision loss across all cases (p = 0.03) and deaths in the degenerative spondylolisthesis group (p < 0.01).
Discussion
Burton et al. were the first to report on the SRS M&M database after it was changed to include more specific reporting of four major complication categories (death, visual deficit, neurological deficit, infection) starting in 2009 [4]. As shown by our data, these complication rates have remained relatively constant over the past decade.
Patients with NM scoliosis had the highest rate of infection throughout the years. This is consistent with the previous report by Burton et al. [4]. The data presented include for both superficial and deep surgical site infections. Mackenzie et al. reported on the surgical site infection rate in patients undergoing instrumentation for scoliosis and found that patients with NM scoliosis had the highest infection rate compared to other scoliosis etiologies as well [12]. Their study showed a higher rate of 13.1% but their patients were followed out to 1 year postoperatively, whereas the SRS database only captures acute infections that occur within 90 days of surgery. Previous studies have noted that the overall risk for surgical site infection in AIS patients ranges from 0.5 to 1.6%, which is consistent with our findings [13].
As with the previous study by Burton et al., congenital kyphosis and dysplastic spondylolisthesis patients had the highest neurological deficit rates [4]. These rates fluctuated from year to year with no clear trend. Several series on the surgical treatment of congenital kyphosis have reported postoperative neurological deficit as a complication. In their group of 23 patients treated with either pedicle subtraction osteotomy or vertebral column resection, Zeng et al. had two (8.7%) patients with a neurological deficit [14]. Both of these patients recovered. Kim et al. reported similar results, in which 2 out of 26 (7.6%) patients had a neurological deficit after treatment for congenital kyphosis [15]. Molinari et al. analyzed 32 patients treated surgically for Meyerding Grade 3 or 4 isthmic dysplastic spondylolisthesis and found only one (3.1%) patient with a neurological deficit who eventually recovered [16].
Similar to the study by Burton et al., the overall mortality rate remained low [4]. Whereas Burton et al. found that the NM scoliosis group had the highest mortality rate, in the time period from 2013 to 2020, NM patients had the second highest mortality rate behind patients in the other kyphosis group. There were several years in which NM patients had a higher mortality rate than the other kyphosis group (2016–2017, 2019–2020). In their prospectively collected, multicenter database in cerebral palsy patients treated surgically, Yaszay et al. found that 11 of 257 (4.3%) patients died between 3 months and 5.6 years postoperatively [17]. In addition, 4 (1.5%) patients died less than a year after surgery and 2 (0.7%) deaths were directly related to the surgical procedure.
In 2017, data for unintentional return to the OR began to be collected. The overall rate was found to be 1.66%. Several studies have looked at unplanned returns to the operating room after spinal surgery. Samdani et al. found a 2.0% unplanned return rate in AIS patients who underwent pedicle screw fixation [18]. In their study, Mehta et al. found an unplanned return to the operating room rate of 4.8% in AIS [19]. Their average time to return to the OR was approximately 734 days.
Infection appeared to decrease significantly year over year in certain groups. This could be attributed to the increased use of vancomycin powder at wound closure. Two groups (neuromuscular scoliosis and other scoliosis) showed a significantly decreasing trend in neurologic deficit. Interestingly, Burton et al. showed an increasing trend in neurologic deficits from 2009 to 2012. The other kyphosis group trended significantly downward for deaths and unintentional return to the OR. The only group to demonstrate a significantly increasing trend was the degenerative spondylolisthesis group with death rate.
Although there was an increase in vision loss cases, these data have not been captured in the M&M database since 2015. This was due to blindness being such a rare event (1 out of 3000 cases). Despite the rarity, it is a devastating consequence and surgeons should be acutely aware of head positioning and avoiding pressure on the eyes when positioning a patient prior to surgery.
It is unclear as to why the mortality rate for degenerative spondylolisthesis increased during the reporting period. Since 2017, the number of cases reported for degenerative spondylolisthesis have increased except for 2020 most likely due to the COVID-19 pandemic. It is possible the increase in cases has resulted in patients with more medical comorbidities undergoing surgery thus resulting in a higher death rate.
This study has several drawbacks, including its retrospective nature, and it is purely descriptive in nature with no p value corrections despite concurrent analyses. In addition, this study relies on members to accurately and completely report their data. Reporting is voluntary and there is no quality assurance process, possibly resulting in a lower rate of complications if the data is incomplete. We also recognize that medical complications are not recorded in our database so the complication rate reported here is most likely much lower than the total complication rate for these procedures. We advise that surgeon performance should not be compared to these data as well as there was no risk adjustment performed. The advantages of this study include the large number of cases. The number of surgeons reporting cases have a wide range of experience and the large number of institutions represented from around the world may help control for differences in patient populations.
Conclusion
The reported complication rates in our study are comparable to years past. There was a decreasing overall trend for infection and neurological deficit. Patients with NM scoliosis had the highest rate of infection. Congenital kyphosis and dysplastic spondylolisthesis patients had the highest neurological deficit rates. While the other kyphosis group had the highest mortality rate, there was a decreasing trend in mortality rate over time. The only increasing trend was mortality rate in the degenerative spondylolisthesis group. Unintentional return to the OR ranged from 1.60 to 1.79%. Given the large number of patients included in the registry, the data presented here should give spine surgeons guidance when counseling patients on complications after surgery.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
The software application and code used for the statistical analysis are available from the corresponding author on reasonable request.
References
MacEwen GD, Bunnell WP, Sriram K (1975) Acute neurological complications in the treatment of scoliosis. A report of the Scoliosis Research Society. J Bone Jt Surg Am 57(3):404–8
Smith JS et al (2010) Complication rates of three common spine procedures and rates of thromboembolism following spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 35(24):2140–9
Coe JD et al (2006) Complications in spinal fusion for adolescent idiopathic scoliosis in the new millennium. A report of the Scoliosis Research Society Morbidity and Mortality Committee. Spine (Phila Pa 1976) 31(3):345–9
Burton DC et al (2016) Results of the scoliosis research society morbidity and mortality database 2009–2012: a report from the morbidity and mortality committee. Spine Deform 4(5):338–343
Hamilton DK, Smith JS, Sansur CA et al (2011) Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: a report of the scoliosis research society morbidity and mortality committee. Spine 36(15):1218–1228
Reames DL, Smith JS, Fu KG et al (2011) Complications in the surgical treatment of 19,360 cases of pediatric scoliosis: a review of the Scoliosis Research Society Morbidity and Mortality database. Spine 36(18):1484–1491
Coe JD, Smith JS, Berven S et al (2010) Complications of spinal fusion for Scheuermann kyphosis: a report of the scoliosis research society morbidity and mortality committee. Spine 35(1):99–103
Smith JS, Saulle D, Chen C et al (2012) Rates and causes of mortality associated with spine surgery based on 108,419 procedures: a review of the Scoliosis Research Society Morbidity and Mortality Database. Spine 37(23):1975–82
Smith JS, Shaffrey CI, Sansur CA et al (2011) Rates of infection after spine surgery based on 108,419 procedures: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine 36(7):556–563
Sansur CA, Smith JS, Glassman SD et al (2011) Scoliosis research society morbidity and mortality of adult scoliosis surgery. Spine 36(9):E593–E597
Smith JS, Sansur CA, Donaldson WF et al (2011) Short-term morbidity and mortality associated with correction of thoracolumbar fixed sagittal plane deformity: a report from the Scoliosis Research Society Morbidity and Mortality Committee. Spine 36(12):958–964
Mackenzie WG, Matsumoto H, Williams BA et al (2013) Surgical site infection following spinal instrumentation for scoliosis: a multicenter analysis of rates, risk factors, and pathogens. J Bone Jt Surg Am 95(9):800–6, S1-2
Vitale MG, Riedel MD, Glotzbecker MP et al (2013) Building consensus: development of a best practice guideline (BPG) for surgical site infection (SSI) prevention in high-risk pediatric spine surgery. J Pediatric Orthop 33(5):471–478
Zeng Y, Chen Z, Qi Q et al (2013) The posterior surgical correction of congenital kyphosis and kyphoscoliosis: 23 cases with minimum 2 years follow up. Eur Spin J 22(2):372–378
Kim YJ, Otsuka NY, Flynn JM et al (2001) Surgical treatment of congenital kyphosis. Spine 26(20):2251–2257
Molinari RW, Bridwell KH, Lenke LG et al (1999) Complications in the surgical treatment of pediatric high-grade, isthmic dysplastic spondylolisthesis. A comparison of three surgical approaches. Spine 24(16):1701–11
Yaszay B, Bartely CE, Sponseller PD et al (2020) Major complications following surgical correction of spine deformity in 257 patients with cerebral palsy. Spine Deform 27:1–8
Samdani AF, Belin EJ, Bennett JT (2013) Unplanned return to the operating room in patients with adolescent idiopathic scoliosis: are we doing better with pedicle screws? Spine 38(21):1842–1847
Mehta NN, Talwar D, Harms Study Group et al (2021) Unplanned return to the operating room (UPROR) after surgery for adolescent idiopathic scoliosis. Spine Deformity 9:1035–1040. https://doi.org/10.1007/s43390-021-00284-9 (Online ahead of print)
Funding
This work was funded by the Scoliosis Research Society.
Author information
Authors and Affiliations
Contributions
LB: Made substantial contribution, drafted manuscript, approved published version, and accountable for all aspects of work. JF: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. CSD-S: Made substantial contributions to analysis and interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. DCB: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. LD: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. JJS: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. MDK: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. EF: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. DG: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. DK: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. WL: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. VS: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. SJS: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. CY: Made substantial contributions to interpretation of data, critically revised manuscript, approved published version, and accountable for all aspects of work. YL: Made substantial contribution, drafted manuscript, approved published version, and accountable for all aspects of work.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Burton reports personal fees and other from DePuy Spine, non-financial support from Scoliosis Research Society, non-financial support from International Spine Study Group, personal fees from Bioventus, personal fees from Globus, personal fees from Progenerative Medical, personal fees from Blue Ocean Spine, outside the submitted work. Dr. Dolan reports grants from POSNA, other from Green Sun Medical, outside the submitted work. Dr. de Kleuver reports grants from Netherlands National Institute of Health Research (ZonMw), grants from SRS research grant, other from Medtronic, outside the submitted work; and is the SRS vice president, the work submitted is from the SRS database. Dr. Lavelle reports personal fees and other from 4-Web, grants from Abryx, grants from AO Foundation, grants from Cerapedics, grants and personal fees from DePuy Spine, grants from Empirical Spine, other from Expanding Innovations, grants and other from Innovasis, grants from Medtronic, other from Prosydian, grants from Spinal Kinetics, Inc., grants from Vertebral Technologies, Inc., personal fees from Vertiflex, outside the submitted work. Dr. Sarwahi reports personal fees from Medical Device Business Services, INC., personal fees from Depuy Synthes, INC., personal fees from Precision Spine, INC., personal fees from Nuvasive, INC., outside the submitted work. Dr. Li reports grants from Scoliosis Research Society, personal fees from Medtronic, non-financial support from Zimmer, outside the submitted work. The rest of the authors have nothing to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bivona, L.J., France, J., Daly-Seiler, C.S. et al. Spinal deformity surgery is accompanied by serious complications: report from the Morbidity and Mortality Database of the Scoliosis Research Society from 2013 to 2020. Spine Deform 10, 1307–1313 (2022). https://doi.org/10.1007/s43390-022-00548-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43390-022-00548-y