Abstract
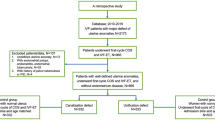
The aim of this study is to evaluate the reproductive outcomes of patients with previous cesarean section (CS) undergoing single-embryo transfer (SET). A total of 5479 patients previously underwent CS or vaginal delivery (VD) were included. The patients with previous CS included single/double cleavage (SCT/DCT), single/double blastocyst stage embryo transfer (SBT/DBT). The comparison of reproductive outcomes between CS and VD, SET, and double-embryo transfer of CS was conducted. The main outcome measures included clinical pregnancy rate (CPR), multiple pregnancy rate (MPR), live birth rate (LBR), and cumulative live birth rate (CLBR). There were no differences in CPR and LBR between patients previously underwent CS and VD, and the preterm birth rate of multiple births in patients underwent CS were significantly higher than underwent VD. As for patients underwent CS, the CPR, MPR, and LBR were lower in patients treated with SCT than DCT in IVF/ICSI cycles. The CPR and LBR of patients treated with SCT were not statistically different compared with DCT and SBT when patients’ age were younger than 35 years in FET cycles, and the MPR of patients treated with SCT was lower. The CPR and LBR of patients treated with SCT were lower than DCT/SBT when patients’ age were 35 years or older in FET cycles. The CPR, LBR, and CLBR of patients treated with SBT were not lower than DCT in IVF/ICSI-ET, FET, and complete cycles, but the MPR was lower. Reducing the number of embryos transferred should be considered seriously for CS. SCT under the 35 years of FET cycles is feasible. SBT is an effective strategy to reduce MPR of IVF/ICSI, FET, and complete cycles regardless of overall or age stratification.




Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ART:
-
assisted reproductive technology
- eSET:
-
elective single embryo transfer
- SCT:
-
single cleavage-stage embryo transfer
- SBT:
-
single blastocyst embryo transfer
- DCT:
-
double cleavage-stage embryo transfer
- DBT:
-
double blastocyst embryo transfer
- CS:
-
cesarean section
- VD:
-
vaginal delivery
- CPR:
-
clinical pregnancy rate
- MPR:
-
multiple pregnancy rate
- LBR:
-
live birth rate
- CLBR:
-
cumulative live birth rate
References
Ye J, Zhang J, Mikolajczyk R, Torloni MR, Gulmezoglu AM, Betran AP. Association between rates of caesarean section and maternal and neonatal mortality in the 21st century: a worldwide population-based ecological study with longitudinal data. BJOG. 2016;123(5):745–53. https://doi.org/10.1111/1471-0528.13592.
Mi J, Liu F. Rate of caesarean section is alarming in China. Lancet (London, England). 2014;383(9927):1463–4. https://doi.org/10.1016/s0140-6736(14)60716-9.
Hellerstein S, Feldman S, Duan T. China’s 50% caesarean delivery rate: is it too high? Bjog. 2015;122(2):160–4. https://doi.org/10.1111/1471-0528.12971.
Gurol-Urganci I, Bou-Antoun S, Lim CP, Cromwell DA, Mahmood TA, Templeton A, et al. Impact of caesarean section on subsequent fertility: a systematic review and meta-analysis. Human Reprod (Oxford, England). 2013;28(7):1943–52. https://doi.org/10.1093/humrep/det130.
Gurol-Urganci I, Cromwell DA, Mahmood TA, van der Meulen JH, Templeton A. A population-based cohort study of the effect of caesarean section on subsequent fertility. Human Reprod (Oxford, England). 2014;29(6):1320–6. https://doi.org/10.1093/humrep/deu057.
Farquhar C, Marjoribanks J. Assisted reproductive technology: an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2018;8:Cd010537. https://doi.org/10.1002/14651858.CD010537.pub5.
Vlachadis N, Vrachnis N, Economou E. Fertility treatments and multiple births in the United States. N Engl J Med. 2014;370(11):1069–70. https://doi.org/10.1056/NEJMc1400242.
Qin J, Wang H, Sheng X, Liang D, Tan H, Xia J. Pregnancy-related complications and adverse pregnancy outcomes in multiple pregnancies resulting from assisted reproductive technology: a meta-analysis of cohort studies. Fertil Steril. 2015;103(6):1492–508.e1–7. https://doi.org/10.1016/j.fertnstert.2015.03.018.
Santana DS, Cecatti JG, Surita FG, Silveira C, Costa ML, Souza JP, et al. Twin pregnancy and severe maternal outcomes: the World Health Organization multicountry survey on maternal and newborn health. Obstet Gynecol. 2016;127(4):631–41. https://doi.org/10.1097/aog.0000000000001338.
Solheim KN, Esakoff TF, Little SE, Cheng YW, Sparks TN, Caughey AB. The effect of cesarean delivery rates on the future incidence of placenta previa, placenta accreta, and maternal mortality. J Matern Fetal Neonatal Med. 2011;24(11):1341–6. https://doi.org/10.3109/14767058.2011.553695.
Kissin DM, Kulkarni AD, Kushnir VA, Jamieson DJ. Number of embryos transferred after in vitro fertilization and good perinatal outcome. Obstet Gynecol. 2014;123(2 Pt 1):239–47. https://doi.org/10.1097/aog.0000000000000106.
Criteria for number of embryos to transfer: a committee opinion. Fertil Steril. 2013;99(1):44–6. https://doi.org/10.1016/j.fertnstert.2012.09.038.
McLernon DJ, Maheshwari A, Lee AJ, Bhattacharya S. Cumulative live birth rates after one or more complete cycles of IVF: a population-based study of linked cycle data from 178,898 women. Human Reprod (Oxford, England). 2016;31(3):572–81. https://doi.org/10.1093/humrep/dev336.
Hu L, Bu Z, Guo Y, Su Y, Zhai J, Sun Y. Comparison of different ovarian hyperstimulation protocols efficacy in poor ovarian responders according to the Bologna criteria. Int J Clin Exp Med. 2014;7(4):1128–34.
Dai W, Ma L, Cao Y, Wu D, Yu T, Zhai J. In vitro fertilization outcome in women with endometrial tuberculosis and tubal tuberculosis. Gynecol Endocrinol. 2019;36:1–5. https://doi.org/10.1080/09513590.2019.1702639.
Chen T, Shi H, Fang LL, Su YC. The effect of endometrial injury on reproductive outcomes of frozen-thawed embryo transfer cycles in women with one implantation failure. J Int Med Res. 2020;48(3):300060520913130. https://doi.org/10.1177/0300060520913130.
Bu Z, Wang K, Dai W, Sun Y. Endometrial thickness significantly affects clinical pregnancy and live birth rates in frozen-thawed embryo transfer cycles. Gynecol Endocrinol. 2016;32(7):524–8. https://doi.org/10.3109/09513590.2015.1136616.
Ledger WL, Anumba D, Marlow N, Thomas CM, Wilson EC. The costs to the NHS of multiple births after IVF treatment in the UK. BJOG. 2006;113(1):21–5. https://doi.org/10.1111/j.1471-0528.2005.00790.x.
Lee MS, Evans BT, Stern AD, Hornstein MD. Economic implications of the Society for Assisted Reproductive Technology embryo transfer guidelines: healthcare dollars saved by reducing iatrogenic triplets. Fertil Steril. 2016;106(1):189–95.e3. https://doi.org/10.1016/j.fertnstert.2016.03.014.
Ben-Nagi J, Walker A, Jurkovic D, Yazbek J, Aplin JD. Effect of cesarean delivery on the endometrium. Int J Gynaecol Obstet. 2009;106(1):30–4. https://doi.org/10.1016/j.ijgo.2009.02.019.
Naji O, Wynants L, Smith A, Abdallah Y, Saso S, Stalder C, et al. Does the presence of a caesarean section scar affect implantation site and early pregnancy outcome in women attending an early pregnancy assessment unit? Human Reprod. 2013;28(6):1489–96. https://doi.org/10.1093/humrep/det110.
Zhang N, Chen H, Xu Z, Wang B, Sun H, Hu Y. Pregnancy, delivery, and neonatal outcomes of in vitro fertilization-embryo transfer in patient with previous cesarean scar. Med Sci Monit. 2016;22:3288–95. https://doi.org/10.12659/msm.900581.
Maheshwari A, Griffiths S, Bhattacharya S. Global variations in the uptake of single embryo transfer. Hum Reprod Update. 2011;17(1):107–20. https://doi.org/10.1093/humupd/dmq028.
Guidance on the limits to the number of embryos to transfer: a committee opinion. Fertil Steril. 2017;107(4):901–3. https://doi.org/10.1016/j.fertnstert.2017.02.107.
Newton CR, McBride J, Feyles V, Tekpetey F, Power S. Factors affecting patients' attitudes toward single- and multiple-embryo transfer. Fertil Steril. 2007;87(2):269–78. https://doi.org/10.1016/j.fertnstert.2006.06.043.
Veleva Z, Vilska S, Hyden-Granskog C, Tiitinen A, Tapanainen JS, Martikainen H. Elective single embryo transfer in women aged 36–39 years. Human Reprod (Oxford, England). 2006;21(8):2098–102. https://doi.org/10.1093/humrep/del137.
Roque M, Lattes K, Serra S, Sola I, Geber S, Carreras R, et al. Fresh embryo transfer versus frozen embryo transfer in in vitro fertilization cycles: a systematic review and meta-analysis. Fertil Steril. 2013;99(1):156–62. https://doi.org/10.1016/j.fertnstert.2012.09.003.
Shapiro BS, Daneshmand ST, Garner FC, Aguirre M, Hudson C. Clinical rationale for cryopreservation of entire embryo cohorts in lieu of fresh transfer. Fertil Steril. 2014;102(1):3–9. https://doi.org/10.1016/j.fertnstert.2014.04.018.
Bottin P, Achard V, Courbiere B, Paci M, Gnisci A, Jouve E, et al. Elective single embryo transfer policy at 48/72 h: which results after fresh transfers and frozen/thawed transfers? Gynecol Obstet Fertil. 2015;43(4):297–303. https://doi.org/10.1016/j.gyobfe.2015.02.007.
Glujovsky D, Farquhar C, Quinteiro Retamar AM, Alvarez Sedo CR, Blake D. Cleavage stage versus blastocyst stage embryo transfer in assisted reproductive technology. Cochrane Database Syst Rev. 2016;6:Cd002118. https://doi.org/10.1002/14651858.CD002118.pub5.
Mullin CM, Fino ME, Talebian S, Krey LC, Licciardi F, Grifo JA. Comparison of pregnancy outcomes in elective single blastocyst transfer versus double blastocyst transfer stratified by age. Fertil Steril. 2010;93(6):1837–43. https://doi.org/10.1016/j.fertnstert.2008.12.137.
Berin I, McLellan ST, Macklin EA, Toth TL, Wright DL. Frozen-thawed embryo transfer cycles: clinical outcomes of single and double blastocyst transfers. J Assist Reprod Genet. 2011;28(7):575–81. https://doi.org/10.1007/s10815-011-9551-7.
Harbottle S, Hughes C, Cutting R, Roberts S, Brison D. Elective single embryo transfer: an update to UK Best Practice Guidelines. Human Fertil (Cambridge, England). 2015;18(3):165–83. https://doi.org/10.3109/14647273.2015.1083144.
Zegers-Hochschild F, Adamson GD, Dyer S, Racowsky C, de Mouzon J, Sokol R, et al. The international glossary on infertility and fertility care, 2017. Fertil Steril. 2017;108(3):393–406. https://doi.org/10.1016/j.fertnstert.2017.06.005.
Acknowledgments
The authors thank professor Qing ling Yang and Dr. Lan Lan Fang for the revision of the manuscripts, and the patients included in this study.
Author information
Authors and Affiliations
Contributions
TC: protocol development, data collection, data analysis, and manuscript writing. BL: data collection, data analysis, and manuscript writing. HS: data collection and data analysis. QZB: protocol development and revised manuscript. QFZ: protocol development and revised manuscript. CYS: protocol development, revised manuscript, and manuscript writing.
Corresponding author
Ethics declarations
Conflict of Interests
The authors declare that they have no conflict of interest.
Ethics Approval
This study was approved by the Institutional ethics committee Review Board of The First Affiliated Hospital of Zheng Zhou University (Science-2019-KY-365).
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 51 kb)
Rights and permissions
About this article
Cite this article
Chen, T., Li, B., Shi, H. et al. Reproductive Outcomes of Single Embryo Transfer in Women with Previous Cesarean Section. Reprod. Sci. 28, 1049–1059 (2021). https://doi.org/10.1007/s43032-020-00345-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s43032-020-00345-w