Abstract
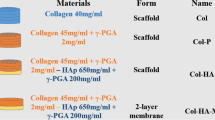
Bone is known to have a natural function to heal itself. However, if the bone damage is beyond a critical degree, intervention such as bone grafting may be imperative. In this work, the fabrication of a novel bone scaffold composed of natural bone components and polycaprolactone (PCL) using 3D printing is put forward. α1, 3-galactosyltransferase deficient pigs were used as the donor source of a xenograft. Decellularized porcine bone (DCB) with attenuated immunogenicity was used as the natural component of the scaffold with the aim to promote bone regeneration. The 3D printed DCB-PCL scaffolds combined essential advantages such as uniformity of the interconnected macropores and high porosity and enhanced compressive strength. The biological properties of the DCB-PCL scaffolds were evaluated by studying cell adhesion, viability, alkaline phosphatase activity and osteogenic gene expression of human bone marrow-derived mesenchymal stem cells. The in vitro results demonstrated that the DCB-PCL scaffolds exhibit an enhanced performance in promoting bone differentiation, which is correlated to the DCB content. Furthermore, critical-sized cranial rat defects were used to assess the effect of DCB-PCL scaffolds on bone regeneration in vivo. The results confirm that in comparison with PCL scaffolds, the DCB-PCL scaffolds can significantly improve new bone formation in cranial defects. Thus, the proposed 3D printed DCB-PCL scaffolds emerge as a promising regeneration alternative in the clinical treatment of large bone defects.








Similar content being viewed by others
References
Bone Grafts and Substitutes Market is Likely to Garner $3.91 Bn by 2025 (EB/OL) (2019). https://finance.yahoo.com/news/bone-grafts-substitutes-market-likely-130055628.html. Accessed 6 May 2019
Liu Y, Jing L, Teoh SH (2013) Review: development of clinically relevant scaffolds for vascularised bone tissue engineering. Biotechnol Adv 31(5):688–705
Zhang X, Awad HA, O’Keefe RJ, Guldberg RE, Schwarz EM (2008) A perspective: engineering periosteum for structural bone graft healing. Clin Orthop Relat Res 466(8):1777–1787
Alio del Barrio JL, Chiesa M, Garagorri N, Garcia-Urquia N, Fernandez-Delgado J, Bataille L, Rodriguez A, Arnalich-Montiel F, Zarnowski T, Alvarez de Toledo JP, Alio JL, De Miguel MP (2015) Acellular human corneal matrix sheets seeded with human adipose-derived mesenchymal stem cells integrate functionally in an experimental animal model. Exp Eye Res 132:91–100
Papadimitropoulos A, Scotti C, Bourgine P, Scherberich A, Martin I (2015) Engineered decellularized matrices to instruct bone regeneration processes. Bone 70:66–72
Magre S, Takeuchi Y, Bartosch B (2003) Xenotransplantation and pig endogenous retroviruses. Rev Med Virol 13(5):311–329
Sachs DH, Sykes M, Robson SC, Cooper DKC (2001) Xenotransplantation. Adv Immunol 79(11):129–223
Pearce AI, Richards RG, Milz S, Schneider E, Pearce SG (2007) Animal models for implant biomaterial research in bone: a review. Eur Cells Mater 13(1):1
Salamanca E, Lee W-F, Lin C-Y, Huang H-M, Lin C-T, Feng S-W, Chang W-J (2015) A novel porcine graft for regeneration of bone defects. Materials 8(5):2523–2536
Salamanca E, Hsu C-C, Huang H-M, Teng N-C, Lin C-T, Pan Y-H, Chang W-J (2018) Bone regeneration using a porcine bone substitute collagen composite in vitro and in vivo. Sci Rep 8(1):984
Phelps CJ, Koike C, Vaught TD, Boone J, Wells KD, Chen S-H, Ball S, Specht SM, Polejaeva IA, Monahan JA, Jobst PM, Sharma SB, Lamborn AE, Garst AS, Moore M, Demetris AJ, Rudert WA, Bottino R, Bertera S, Trucco M, Starzl TE, Dai Y, Ayares DL (2003) Production of alpha 1,3-galactosyltransferase-deficient pigs. Science 299(5605):411–414
Hisashi Y, Yamada K, Kuwaki K, Tseng YL, Dor FJMF, Houser SL, Robson SC, Schuurman HJ, Cooper DKC, Sachs DH, Colvin RB, Shimizu A (2008) Rejection of Cardiac Xenografts Transplanted from α1,3-Galactosyltransferase Gene-Knockout (GalT-KO) Pigs to Baboons. Am J Transpl 8(12):2516–2526
Cheng CW, Solorio LD, Alsberg E (2014) Decellularized tissue and cell-derived extracellular matrices as scaffolds for orthopaedic tissue engineering. Biotechnol Adv 32(2):462–484
Hashimoto Y, Funamoto S, Kimura T, Nam K, Fujisato T, Kishida A (2011) The effect of decellularized bone/bone marrow produced by high-hydrostatic pressurization on the osteogenic differentiation of mesenchymal stem cells. Biomaterials 32(29):7060–7067
Hoch AI, Mittal V, Mitra D, Vollmer N, Zikry CA, Leach JK (2016) Cell-secreted matrices perpetuate the bone-forming phenotype of differentiated mesenchymal stem cells. Biomaterials 74:178–187
Lu H, Hoshiba T, Kawazoe N, Koda I, Song M, Chen G (2011) Cultured cell-derived extracellular matrix scaffolds for tissue engineering. Biomaterials 32(36):9658–9666
Xin W, Man J, Zhou Z, Gou J, Hui D (2017) 3D printing of polymer matrix composites: a review and prospective. Compos Part B Eng 110:442–458
Amini AR, Laurencin CT, Nukavarapu SP (2012) Bone tissue engineering: recent advances and challenges. Crit Rev Biomed Eng 40(5):363–408
Trakoolwannachai V, Kheolamai P, Ummartyotin S (2019) Characterization of hydroxyapatite from eggshell waste and polycaprolactone (PCL) composite for scaffold material. Compos Part B Eng 173:106974
Qi X, Pei P, Zhu M, Du X, Xin C, Zhao S, Li X, Zhu Y (2017) Three dimensional printing of calcium sulfate and mesoporous bioactive glass scaffolds for improving bone regeneration in vitro and in vivo. Sci Rep 7:42556
Zhang J, Zhao S, Zhu Y, Huang Y, Zhu M, Tao C, Zhang C (2014) Three-dimensional printing of strontium-containing mesoporous bioactive glass scaffolds for bone regeneration. Acta Biomater 10(5):2269–2281
Seyednejad H, Gawlitta D, Kuiper RV, Bruin AD, Nostrum CFV, Vermonden T, Dhert WJA, Hennink WE (2012) Invivo biocompatibility and biodegradation of 3D-printed porous scaffolds based on a hydroxyl-functionalized poly(ε-caprolactone). Biomaterials 33(17):4309–4318
Su AP, Su HL, Wan DK (2011) Fabrication of porous polycaprolactone/hydroxyapatite (PCL/HA) blend scaffolds using a 3D plotting system for bone tissue engineering. Bioproc Biosyst Eng 34(4):505–513
Tarafder S, Bose S (2014) Polycaprolactone-coated 3D printed tricalcium phosphate scaffolds for bone tissue engineering: in vitro alendronate release behavior and local delivery effect on in vivo osteogenesis. ACS Appl Mater Interfaces 6(13):9955–9965
Saito E, Suarez-Gonzalez D, Murphy WL, Hollister SJ (2015) Biomineral coating increases bone formation by ex vivo BMP-7 gene therapy in rapid prototyped poly(l-lactic acid) (PLLA) and poly(ε-caprolactone) (PCL) porous scaffolds. Adv Healthc Mater 4(4):621–632
Mitsak AG, Kemppainen JM, Harris MT, Hollister SJ (2011) Effect of polycaprolactone scaffold permeability on bone regeneration in vivo. Tissue Eng PT A 17(13–14):1831
Pei X, Ma L, Zhang B, Sun J, Sun Y, Fan Y, Gou Z, Zhou C, Zhang X (2017) Creating hierarchical porosity hydroxyapatite scaffolds with osteoinduction by three-dimensional printing and microwave sintering. Biofabrication 9(4):045008
Zhang B, Sun H, Wu L, Ma L, Xing F, Kong Q, Fan Y, Zhou C, Zhang X (2019) 3D printing of calcium phosphate bioceramic with tailored biodegradation rate for skull bone tissue reconstruction. Bio Des Manuf 2(3):161–171
Oladapo BI, Zahedi SA, Adeoye AOM (2019) 3D printing of bone scaffolds with hybrid biomaterials. Compos Part B Eng 158:428–436
Mandair GS, Morris MD (2015) Contributions of Raman spectroscopy to the understanding of bone strength. Bonekey Rep 4:620
Taddei P, Tinti A, Reggiani M, Fagnano C (2005) In vitro mineralization of bioresorbable poly(ɛ-caprolactone)/apatite composites for bone tissue engineering: a vibrational and thermal investigation. J Mol Struct 744(4):135–143
Kister G, Cassanas G, Bergounhon M, Hoarau D, Vert M (2000) Structural characterization and hydrolytic degradation of solid copolymers of D, L-lactide-co-epsilon-caprolactone by Raman spectroscopy. Polymer 41(3):925–932
Zhang W, Ullah I, Shi L, Zhang Y, Ou H, Zhou J, Ullah MW, Zhang X, Li W (2019) Fabrication and characterization of porous polycaprolactone scaffold via extrusion-based cryogenic 3D printing for tissue engineering. Mater Des 180:107946
Lam CX, Savalani MM, Teoh SH, Hutmacher DW (2008) Dynamics of in vitro polymer degradation of polycaprolactone-based scaffolds: accelerated versus simulated physiological conditions. Biomed Mater 3(3):034108
Dimitriou R, Tsiridis E, Giannoudis PV (2005) Current concepts of molecular aspects of bone healing. Injury 36(12):1392–1404
Narayanan K, Leck KJ, Gao S, Wan AC (2009) Three-dimensional reconstituted extracellular matrix scaffolds for tissue engineering. Biomaterials 30(26):4309–4317
Zhao F, Kirby M, Roy A, Hu Y, Guo XE, Wang X (2018) Commonality in the microarchitecture of trabecular bone: a preliminary study. Bone 111:59–70
Liu F, Liu Y, Li X, Wang X, Li D, Chung S, Chen C, Lee I-S (2019) Osteogenesis of 3D printed macro-pore size biphasic calcium phosphate scaffold in rabbit calvaria. J Biomater Appl 33(9):1168–1177
Wu C, Luo Y, Cuniberti G, Yin X, Gelinsky M (2011) Three-dimensional printing of hierarchical and tough mesoporous bioactive glass scaffolds with a controllable pore architecture, excellent mechanical strength and mineralization ability. Acta Biomater 7(6):2644–2650
Millis D, Levine D (2014) Acknowledgments. In: Millis D, Levine D (eds) Canine rehabilitation and physical therapy, 2nd edn. W.B. Saunders, St. Louis
Ma J, Lin L, Zuo Y, Zou Q, Ren X, Li J, Li Y (2019) Modification of 3D printed PCL scaffolds by PVAc and HA to enhance cytocompatibility and osteogenesis. RSC Adv 9:5338–5346
Orr TE, Villars PA, Mitchell SL, Hsu HP, Spector M (2001) Compressive properties of cancellous bone defects in a rabbit model treated with particles of natural bone mineral and synthetic hydroxyapatite. Biomaterials 22(14):1953–1959
Beresford JN, Graves SE, Smoothy CA (2010) Formation of mineralized nodules by bone derived cells in vitro: a model of bone formation? Am J Med Genet 45(2):163–178
Ramaswamy Y, Wu C, Zhou H, Zreiqat H (2008) Biological response of human bone cells to zinc-modified Ca-Si-based ceramics. Acta Biomater 4(5):1487–1497
Acknowledgements
The authors acknowledge the financial support from National Natural Science Foundation of China (81601626), Zhejiang Provincial Natural Science of Foundation of China (Y20C070010), start-up funding from Wenzhou Institute, University of Chinese Academy of Sciences (WIUCASQD2019002) and Singapore MOE Tier 1 Grant RG46/18. The authors would also like to acknowledge the Yifan Dai’s lab for providing bone tissue from alpha 1, 3 GT deficient pigs.
Author information
Authors and Affiliations
Contributions
H.Q. Li and L.P. Tan designed the experiments. Q.X. Pan, C.Y. Gao, Y.Y. Wang and Y.L. Wang performed the experiments. Q.X. Pan and C.Y. Gao drafted the manuscript. C. Mao, Q. Wang, F. Wen, S.N. Economidou and D. Douroumis performed the data analysis. H.Q. Li provided funding for this project and supervised the experiments. All authors edited and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Ethical approval
Any related research on animal experiments included in this study is in line with ethical requirements.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pan, Q., Gao, C., Wang, Y. et al. Investigation of bone reconstruction using an attenuated immunogenicity xenogenic composite scaffold fabricated by 3D printing. Bio-des. Manuf. 3, 396–409 (2020). https://doi.org/10.1007/s42242-020-00086-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s42242-020-00086-4