Key summary points
To investigate the association between iron supplementation and blood transfusion risks, hospital length of stay, postoperative infection, and mortality in geriatric patients with hip fracture surgeries.
AbstractSection FindingsData from this meta-analysis suggest that iron supplementation, especially preoperative intravenous use of iron at 200–300 mg, is associated with a reduction in the rate and volume of blood transfusions, infections and length of hospital stay in older patients with hip fracture surgeries.
AbstractSection MessageThese findings support the preoperative intravenous use of iron at 200–300 mg in older adults undergoing hip fracture surgeries.
Abstract
Aims
To assess the efficacy and safety of iron supplementation for perioperative anemia in geriatric patients with hip fracture.
Methods
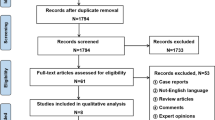
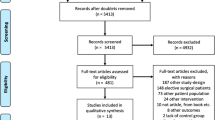
A systematic search was conducted for studies published using PubMed, EMBASE and Cochrane Library Databases that compared iron supplementation with placebo in patients undergoing hip fracture surgery. The outcomes were blood transfusion rate and volume, length of stay, infection and mortality (last follow-up). Sub-group and sensitivity analyses were performed in cases of substantial heterogeneity.
Results
The meta-analysis (6 studies: 1201 patients) indicated that iron supplements were not associated with reducing blood transfusion rate (OR 0.92, 95% CI 0.60–1.41; P = 0.69), but high heterogeneity (I2 = 61%) was detected and a significant association was found in sensitivity analysis of four studies (n = 637; OR 0.68, 95% CI 0.49–0.95; P = 0.02). A significant reduction was detected in transfusion volume (two studies: n = 234; MD − 0.45 units/patient, 95% CI − 0.74 to − 0.16; P = 0.002), hospital stay (five studies: n = 998; MD − 1.42, 95% CI − 2.18 to − 0.67; P = 0.0002) and caused no increased risk of mortality (five studies: n = 937; OR 0.94, 95% CI 0.65–1.36; P = 0.76) and infection (four studies: n = 701; OR 0.58, 95% CI 0.38–0.90; P = 0.01). Sub-group analyses of four studies showed that the preoperative intravenous use of iron at 200–300 mg (two studies) may be the beneficial option for hip fractures patients.
Conclusions
Iron supplementation, especially preoperative intravenous use of 200–300 mg iron, is safe and associated with reducing transfusion requirement and hospital stay. Unfortunately, data were too limited to draw a definite conclusion. Further evaluation is required before recommending iron supplementation for older patients with hip fracture surgeries.






Similar content being viewed by others
References
Beattie WS, Karkouti K, Wijeysundera DN, Tait G (2009) Risk associated with preoperative anemia in noncardiac surgery a single-center cohort study. Anesthesiology 110(3):574–581. https://doi.org/10.1097/ALN.0b013e31819878d3
AAOS (2014) Management of hip fractures in the elderly. 2014:17. https://www.aaos.org/Research/guidelines/HipFxSummaryofRecommendations.pdf Accessed 21 Feb 2015
Carson JL, Duff A, Berlin JA, Lawrence VA, Poses RM, Huber EC et al (1998) Perioperative blood transfusion and postoperative mortality. Jama J Am Med Assoc 279(3):199–205. https://doi.org/10.1001/jama.279.3.199
Nemeth E, Ganz T (2014) Anemia of inflammation. Hematol Oncol Clin N Am 28(4):671–681. https://doi.org/10.1016/j.hoc.2014.04.005
Warner MA, Shore-Lesserson L, Shander A, Patel SY, Perelman SI, Guinn NR (2020) Perioperative anemia: prevention, diagnosis, and management throughout the spectrum of perioperative care. Anesth Analg 130(5):1364–1380. https://doi.org/10.1213/ane.0000000000004727
Girelli D, Nemeth E (2016) Hepcidin in the diagnosis of iron disorders. Blood 127(23):2809–2813. https://doi.org/10.1182/blood-2015-12-639112
Salido JA, Marin LA, Gomez LA, Zorrilla P, Martinez C (2002) Preoperative hemoglobin levels and the need for transfusion after prosthetic hip and knee surgery - analysis of predictive factors. J Bone Jt Surg Am Vol 84A(2):216–220. https://doi.org/10.2106/00004623-200202000-00008
Abdullah HR, Sim YE, Hao Y, Lin GY, Liew GHC, Lamoureux EL et al (2017) Association between preoperative anaemia with length of hospital stay among patients undergoing primary total knee arthroplasty in Singapore: a single-centre retrospective study. BMJ Open 7(6):e016403. https://doi.org/10.1136/bmjopen-2017-016403
Brunskill SJ, Millette SL, Shokoohi A, Pulford EC, Doree C, Murphy MF et al (2015) Red blood cell transfusion for people undergoing hip fracture surgery. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD009699.pub2
Foss NB, Kehlet H (2006) Hidden blood loss after surgery for hip fracture. J Bone Jt Surg Br Vol 88B(8):1053–1059. https://doi.org/10.1302/620x.88b8
Theusinger OM, Leyvraz PF, Schanz U, Seifert B, Spahn DR (2007) Treatment of iron deficiency anemia in orthopedic surgery with intravenous iron: efficacy and limits: a prospective study. Anesthesiology 107(6):923–927. https://doi.org/10.1097/01.anes.0000291441.10704.82
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P (2013) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
Prasad N, Rajamani V, Hullin D, Murray JM (2009) Post-operative anaemia in femoral neck fracture patients: ddoes it need treatment? A single blinded prospective randomised controlled trial. Injury 40(10):1073–1076. https://doi.org/10.1016/j.injury.2009.02.021
Crooks J, O’Malley K, Stevenson IH (1976) Pharmacokinetics in the elderly. Clin Pharmacokinet 1(4):280–296. https://doi.org/10.2165/00003088-197601040-00003
Lipschitz DA, Udupa KB, Milton KY, Thompson CO (1984) Effect of age on hematopoiesis in man. Blood 63(3):502–509
Parker MJ (2010) Iron supplementation for anemia after hip fracture surgery: a randomized trial of 300 patients. J Bone Jt Surg Am Vol 92(2):265–269. https://doi.org/10.2106/jbjs.i.00883
Cuenca J, Garcia-Erce JA, Martinez AA, Solano VM, Molina J, Munoz M (2005) Role of parenteral iron in the management of anaemia in the elderly patient undergoing displaced subcapital hip fracture repair: preliminary data. Arch Orthop Trauma Surg 125(5):342–347. https://doi.org/10.1007/s00402-005-0809-3
Serrano-Trenas JA, Ugalde PF, Cabello LM, Chofles LC, Lázaro PS, Benítez PC (2011) Role of perioperative intravenous iron therapy in elderly hip fracture patients: a single-center randomized controlled trial. Transfusion 51(1):97–104. https://doi.org/10.1111/j.1537-2995.2010.02769.x
Cuenca J, Garcia-Erce JA, Munoz M, Izuel M, Martinez AA, Herrera A (2004) Patients with pertrochanteric hip fracture may benefit from preoperative intravenous iron therapy: a pilot study. Transfusion 44(10):1447–1452. https://doi.org/10.1111/j.1537-2995.2004.04088.x
Yang Y, Li H, Li B, Wang Y, Jiang S, Jiang L (2011) Efficacy and safety of iron supplementation for the elderly patients undergoing hip or knee surgery: a meta-analysis of randomized controlled trials. J Surg Res 171(2):e201–e207. https://doi.org/10.1016/j.jss.2011.08.025
Shin HW, Park JJ, Kim HJ, You HS, Choi SU, Lee MJ (2019) Efficacy of perioperative intravenous iron therapy for transfusion in orthopedic surgery: a systematic review and meta-analysis. PLoS ONE. https://doi.org/10.1371/journal.pone.0215427
García-Erce JACJ, Gómez-Ramírez S et al (2009) Posibilidades de tratamiento de la anemia perioperatoriaen cirugía ortopédica y traumatología. Anemia 2:17–27
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF (2000) Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Onkologie 23(6):597–602. https://doi.org/10.1159/000055014
Mantel N, Haenszel W (1959) Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst 22(4):719–748
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7(3):177–188
Higgins JPT, Green S, eds (2011) Cochrane handbook for systematic reviews of interventions; version 5.1.0 [updated March 2011]. The cochrane collaboration. https://www.cochrane-handbook.org. Published 2011. Accessed 28 June 2011
Bernabeu-Wittel M, Romero M, Ollero-Baturone M, Aparicio R, Murcia-Zaragoza J, Rincon-Gomez M et al (2016) Ferric carboxymaltose with or without erythropoietin in anemic patients with hip fracture: a randomized clinical trial. Transfusion 56(9):2199–2211. https://doi.org/10.1111/trf.13624
Izuel Rami M, Gomez Barrera M, Villar Fernandez I, Rabanaque Hernandez MJ, Cuenca Espierrez J, Garcia-Erce JA (2007) Budget impact analysis of a blood saving program for urgent traumatological surgery. Med Clin 128(1):7–11
Izuel-Rami M, Cuenca Espierrez J, Garcia-Erce JA, Gomez-Barrera M, Carcelen Andres J, Rabanaque Hernandez MJ (2005) Perioperative anaemia in geriatric patients with hip fracture. Farmacia hospitalaria : organo oficial de expresion cientifica de la Sociedad Espanola de Farmacia Hospitalaria 29(4):250–257
Gomez-Ramirez S, Angeles Maldonado-Ruiz M, Campos-Garrigues A, Herrera A, Munoz M (2019) Short-term perioperative iron in major orthopedic surgery: state of the art. Vox Sang 114(1):3–16. https://doi.org/10.1111/vox.12718
Bisbe ECJ, Sáez M et al (2008) Prevalence of preoperative anemia and hematinic deficiencies in patients scheduled for major orthopedic surgery. Transfus Altern Transfus Med 4:166–173
Munoz M, Garcia-Erce JA, Remacha AF (2011) Disorders of iron metabolism. Part II: iron deficiency and iron overload. J Clin Pathol 64(4):287–296. https://doi.org/10.1136/jcp.2010.086991
O'Lone EL, Hodson EM, Nistor I, Bolignano D, Webster AC, Craig JC (2019) Parenteral versus oral iron therapy for adults and children with chronic kidney disease. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD007857.pub3
Kulnigg S, Stoinov S, Simanenkov V, Dudar LV, Karnafel W, Garcia LC et al (2008) A novel intravenous iron formulation for treatment of anemia in inflammatory bowel disease: the ferric carboxymaltose (FERINJECT((R))) randomized controlled trial. Am J Gastroenterol 103(5):1182–1192. https://doi.org/10.1111/j.1572-0241.2007.01744.x
Shah A, Palmer AJR, Fisher SA, Rahman SM, Brunskill S, Doree C et al (2018) What is the effect of perioperative intravenous iron therapy in patients undergoing non-elective surgery? A systematic review with meta-analysis and trial sequential analysis. Perioper Med 7:30. https://doi.org/10.1186/s13741-018-0109-4
Halm EA, Wang JJ, Boockvar K, Penrod J, Silberzweig SB, Magaziner J et al (2004) The effect of perioperative anemia on clinical and functional outcomes in patients with hip fracture. J Orthop Trauma 18(6):369–374
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ (2008) Mortality following hip fracture: Trends and geographical variations over the last 40 years. Injury Int J Care Injured 39(10):1157–1163. https://doi.org/10.1016/j.injury.2008.03.022
Zhang L, Yin P, Lv H, Long A, Gao Y, Zhang L et al (2016) Anemia on admission is an independent predictor of long-term mortality in hip fracture population: a prospective study with 2-year follow-up. Medicine 95(5):e2469. https://doi.org/10.1097/MD.0000000000002469
Avenell A, Smith TO, Curtain JP, Mak JC, Myint PK (2016) Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD001880.pub6
Engoren M, Mitchell E, Perring P, Sferra J (2008) The effect of erythrocyte blood transfusions on survival after surgery for hip fracture. J Trauma Injury Infect Crit Care 65(6):1411–1415. https://doi.org/10.1097/TA.0b013e318157d9f9
Chertow GM, Mason PD, Vaage-Nilsen O, Ahlmen J (2006) Update on adverse drug events associated with parenteral iron. Nephrol Dial Transplant 21(2):378–382. https://doi.org/10.1093/ndt/gfi253
Musallam KM, Tamim HM, Richards T, Spahn DR, Rosendaal FR, Habbal A et al (2011) Preoperative anaemia and postoperative outcomes in non-cardiac surgery: a retrospective cohort study. Lancet 378(9800):1396–1407. https://doi.org/10.1016/s0140-6736(11)61381-0
Shokoohi A, Stanworth S, Mistry D, Lamb S, Staves J, Murphy MF (2012) The risks of red cell transfusion for hip fracture surgery in the elderly. Vox Sang 103(3):223–230. https://doi.org/10.1111/j.1423-0410.2012.01606.x
Funding
This work was supported by Sichuan Science and Technology Program (2018SZ0246) and National Nature Science Foundation of China (No. 81571003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not required since it is a review of already published works.
Informed consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Chen, R., Li, L., Xiang, Z. et al. Association of iron supplementation with risk of transfusion, hospital length of stay, and mortality in geriatric patients undergoing hip fracture surgeries: a meta-analysis. Eur Geriatr Med 12, 5–15 (2021). https://doi.org/10.1007/s41999-020-00366-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41999-020-00366-3