Abstract
Childhood obesity and its negative relation with children’s brain health has become a growing health concern. Over the last decade, literature has indicated that physical activity attenuates cognitive impairment associated with obesity and excess adiposity in children. However, there is no comprehensive review that considers the extent to which these factors affect different domains of cognition. This narrative review comprehensively summarizes behavioral, neuroimaging, and neuroelectric findings associated with chronic physical activity and fitness on brain and cognition in childhood obesity. Based on the literature reviewed, increased adiposity has a demonstrated relationship with neurocognitive health via mechanisms triggered by central inflammation and insulin resistance, with the most pronounced decrements observed for cognitive domains that are prefrontal- and hippocampal-dependent. Fortunately, physical activity, especially interventions enhancing aerobic fitness and motor coordination, have demonstrated efficacy for attenuating the negative effects of obesity across different subdomains of structural and functional brain imaging, cognition, and multiple academic outcomes in children with overweight or obesity. Such mitigating effects may be accounted for by attenuated central inflammation, improved insulin sensitivity, and increased expression of neurotrophic factors. Lastly, individual differences appear to play a role in this relationship, as the manipulation of physical activity characteristics, the employment of a wide array of cognitive and academic measures, the inclusion of different adiposity measures that are sensitive to neurocognitive function, and the utilization of an inter-disciplinary approach have been found to influence the relationship between physical activity and excess adiposity on brain and cognition.
Similar content being viewed by others
Introduction
The obesity epidemic continues to affect a remarkably high proportion of the world’s population. It is projected that the percentage of adults who are overweight or obese across the world could increase from 33% in 2005 to 58% by 2030 (Kelly et al., 2008). Moreover, a 2016 report from the World Health Organization (WHO) indicated that over 340 million children and adolescents aged 5 to 19 years old worldwide are overweight or obese (WHO, 2020). Given that childhood obesity is projected to continuously increase, accumulation of excessive adiposity has become a concerning public health issue among children and adolescents in the developed world (WHO, 2020).
Obesity is clinically defined as the excessive accumulation of adiposity that impairs health (Caterson & Gill, 2002). The most common measure used to characterize obesity is body mass index (BMI), which is calculated as an individual’s weight in kilograms divided by the square of their height in meters. Due to the variability of height and weight that occurs during growth and development, assessment of a child’s BMI necessitates comparison to an age- and sex-adjusted reference (Ebbeling & Ludwig, 2008). Moreover, with advancements in imaging technology, adiposity variables can be measured using dual-energy x-ray absorptiometry (DXA), which affords characterization of the specific distribution of fat mass within the body. For example, subcutaneous abdominal adipose tissue (SAAT) is the fat present directly under the skin in the abdominal area. SAAT is not only a physical buffer for the body but also where excess energy is stored (Freedland, 2004). In adults, roughly 80% of all body fat is stored as SAAT (Wajchenberg, 2000). When the storage capacity of SAAT is exceeded, or the body is not able to make more fat cells, fat begins to accumulate in other locations such as the viscera. By contrast, visceral adipose tissue (VAT) is the fat stored within the abdominal cavity, including the regions surrounding vital organs such as the liver, pancreas, and intestines. Increased VAT is related to a higher risk of metabolic disease, as it produces inflammatory cytokines and hormones (Chaldakov et al., 2003).
Childhood obesity has been linked to many health complications, including metabolic (e.g., metabolic syndrome [MetS]) and cardiovascular dysfunctions (e.g., dyslipidemia, insulin resistance) (Ebbeling et al., 2002). Over the last decade, a growing body of literature has emerged to suggest that excessive adiposity may also affect cognition, brain function, and academic performance in children (Cadenas-Sanchez et al., 2020a; Davis & Cooper, 2011; García‐Hermoso et al., 2021; Kamijo et al., 2012a, b; Khan et al., 2015; Raine et al., 2018). Although the underlying causes for this relationship are unknown, some have speculated that reduced energy expenditure may be one major cause of childhood obesity (Moreno et al., 2011), which is not surprising given that physical inactivity and obesity are inherently correlated (Hill et al., 2012; Metcalf et al., 2011). According to a worldwide report across 49 countries in 2018, approximately 75% of school children are considered physically inactive (Children’s Hospital of Eastern Ontario Research Institute, 2018), and a few studies have linked sedentarism with obesity and poorer cortical integrity during maturation (Zavala-Crichton et al., 2020). Importantly, intervention data, including randomized controlled trials (RCT), have indicated that physical activity decreases adiposity (Logan et al., 2021; Raine et al., 2017) and alleviates the detrimental influence of adiposity on cognition and brain function in children with overweight and obesity, particularly higher-order aspects of cognition including attention, executive function, and planning/decision making (Davis et al., 2011; Krafft et al., 2014c; Liu et al., 2018; Logan et al., 2021; Raine et al., 2017). Cross-sectional evidence in children with overweight and obesity has further indicated an association of increased fitness with better academic performance, an overall measure of neurocognitive health and integrity that provides insight into real-world cognitive performance (Cadenas-Sanchez et al., 2020b; Davis & Cooper, 2011; García‐Hermoso et al., 2021).
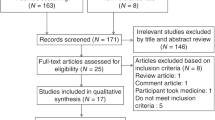
Despite the rapid growth of this line of research, which has led to several literature reviews summarizing the relationship of physical activity on different domains of cognition in children with overweight or obesity (Chang et al., 2017; Martin et al., 2018; Sun et al., 2021), those reviews have focused exclusively on behavioral outcomes of cognition and have not considered the developing body of evidence for changes in brain structure and function concurrent with behavioral outcomes. That is, to date, no literature review exists that comprehensively summarizes findings from both behavioral (i.e., cognitive outcomes, academic performance) and neuroimaging measures (e.g., structural and functional magnetic resonance imaging [MRI, fMRI], event-related brain potentials [ERPs]). A better understanding of the underlying mechanisms reflected by neuroimaging measures can inform tangible biomarkers that can be targeted in the treatment of childhood obesity and its associated relationship with various neurocognitive and health outcomes. Hence, the aim of this review is to consider the recent empirical evidence exploring the association of physical activity with brain structure and function, cognition, and academic performance in children with overweight and obesity. Further, this review aims to summarize the neurobiological mechanisms that may underlie the deleterious effect of obesity and adiposity on brain and cognition and the ameliorative effects of physical activity and fitness on these outcomes. Here, we summarize evidence pertinent to (a) the detrimental relationship of obesity and excess adiposity on brain, cognition, and academic performance during childhood, and the neurobiological mechanisms that may account for the detrimental relationship of obesity and adiposity on brain and cognition, and (b) the effects of physical activity and fitness on brain, cognition, and academic performance in children with overweight or obesity, and the neurobiological mechanisms that may drive the physical activity-induced effects. The goal of this literature review is to critically review the current state of literature addressing the role of physical activity as an effective means to combat childhood obesity and sedentarism, as well as its associated negative impact on cognitive and brain health. It should be noted that, however, the narrative nature of this review precludes estimation of the size of effects of either obesity or chronic physical activity on brain and cognition in children. Caution should be practiced when interpreting the extent in which obesity or physical activity may affect children’s brain and cognition in studies summarized by the current review.
The Detrimental Relationship of Obesity and Adiposity on Brain and Cognition
Potential Mechanisms
A growing body of evidence has suggested that the detrimental effects of excessive adiposity, often characterized by the percentage of whole-body fat (%fat) and VAT in particular, on brain and cognition can be accounted for by increased secretion of proinflammatory cytokines leading to central inflammation and exacerbated insulin resistance resulting in cerebrovascular dysfunctions. Specifically, the accumulation of VAT induces secretion of a series of proinflammatory adipokines/cytokines, including fibrinogen, C-reactive protein, interleukin (IL)-1, and IL-6 (Doupis et al., 2011). These cytokines are able to cross the blood–brain barrier and stimulate hyperactivity of the sympathetic nervous system that has been associated with central inflammation (Erion et al., 2014; Lambert et al., 2015; Miller & Spencer, 2014; Willette & Kapogiannis, 2015; Yates et al., 2012). Central inflammation is a major cause of dysregulation of the hypothalamic–pituitary–adrenal (HPA) axis, which, in turn, results in excessive secretion of stress-related hormones (i.e., cortisol) in brain areas associated with higher-order cognition, including the prefrontal cortex and hippocampus. Excessive secretion of cortisol in the brain can be accompanied by oxidative stress that decreases mRNA expression of neurotrophic factors, including brain-derived neurotrophin factor (BDNF), causing cell apoptosis, and decreased synapse plasticity (Miller & Spencer, 2014; Willette & Kapogiannis, 2015; Yates et al., 2012). These mechanisms driven by central inflammation induce volumetric changes in global and regional gray matter and hippocampal neurodegeneration (Marsland et al., 2015; Takeda et al., 2014). Indeed, structural imaging data have indicated a relationship between greater BMI and decreased gray matter volume in multiple brain areas, including frontal, temporal, and parietal cortices, as well as thalamus, and limbic regions of the cortex (Alosco et al., 2014; Ou et al., 2015).
Additionally, converging evidence has demonstrated that obesity-associated insulin resistance also manifests as reductions in brain insulin sensitivity, and this can negatively impact both neurocognitive functioning as well as synaptic and structural plasticity within the prefrontal cortex, hippocampus, and medial and temporal cortices (Cheke et al., 2017; Heni et al., 2015). Peripheral insulin resistance and hyperinsulinemia negatively affect kidney function. The associated increase in sodium reabsorption ultimately results in hypertension or elevated blood pressure (Alosco et al., 2013), which, in turn, promotes endothelial dysfunction (e.g., arterial stiffness, increased intima-media thickness) and atherosclerosis resulting in deficits in cerebral perfusion and/or exacerbates global and regional brain atrophy (Ross et al., 2015), and white matter hyperintensities (Kullmann et al., 2015; Wickman et al., 2013). Accordingly, there appear to be multiple possible mechanisms in play that may underlie the negative influence of excess adiposity on cognitive and brain health (see Fig. 1). Figure 1 summarizes the detrimental effects of excess adiposity and obesity on children’s cognitive and brain health.
Brain Structure
As noted above, increased central inflammation, decreased insulin sensitivity, and cerebrovascular abnormalities induced by excess adiposity could result in structural changes in the brain. The relatively recent advent of structural neuroimaging techniques, including structural MRI measures, affords better resolution of structural changes induced by excess adiposity and obesity. As such, structural MRI data have indicated a relationship between greater BMI and decreased gray matter volume in multiple brain areas, including frontal, temporal, and parietal cortices, and as well as thalamic and limbic regions of the subcortex (Alosco et al., 2014; Ou et al., 2015). Other studies have also found that increased BMI is associated with reduced global cortical thickness, as well as specific reductions in cortical thickness in prefrontal cortical regions (Laurent et al., 2020; Ronan et al., 2020). Decreased prefrontal cortical thickness was further found to mediate the association between increased BMI and poorer performance on executive function tasks (Laurent et al., 2020). Using diffusion-tensor imaging (DTI), an MRI technique used to estimate white matter structure, Yau and colleagues observed reduced white matter integrity and enlarged cerebrospinal fluid space in the whole brain and the frontal lobe in particular, in obese adolescents (Yau et al., 2010). Together, these preliminary findings point to a detrimental effect of excess adiposity on macro- and micro-structure correlates of the brain during development.
Brain Function
In addition to structural changes associated with excess adiposity, a growing body of literature points to the relation of adiposity on functional brain correlates of cognition. In particular, electroencephalography, and more specifically ERPs, has been used to delineate real-time neural responses during cognitive tasks (Alatorre-Cruz et al., 2021; Kamijo et al., 2014; Kamijo et al., 2012b; Tsai et al., 2016; Walk et al., 2020). ERPs refer to patterns of neuroelectric activation that occur in response to, or in preparation for, a stimulus or response (Luck, 2014). This approach offers the requisite temporal resolution to gain insight into cognitive operations that occur between stimulus engagement and response execution, and may be more sensitive in parsing the negative effects of childhood obesity on the various cognitive operations underlying overt task performance. As such, Kamijo et al. (2012b) investigated the association of childhood obesity and the N2 component of an ERP in preadolescent children. The N2-ERP occurs approximately 200 to 400 ms after stimulus onset, with a topographic maximum over the frontocentral scalp area (Larson et al., 2014). Studies have proposed that the N2-ERP is associated with processes underlying conflict detection, with greater amplitude representing greater task-evoked conflict between task-relevant and task-irrelevant information (Larson et al., 2014). Specifically, Kamijo et al. (2012b) found that children with obesity had larger N2 amplitude during trials with greater inhibitory control demands relative to lower-demand trials, whereas this task-related difference was not seen in normal-weight children. Further, data from Alatorre-Cruz et al. (2021) indicated that children with obesity revealed no difference in N2 latency between trials with varied inhibitory control, whereas their normal-weight peers manifested longer N2 latency, along with higher response accuracy, during trials with greater inhibitory control relative lower-demands trials. This suggest that while children with normal weight triggered a conflict-monitoring response that compensated for the need of greater inhibitory control, such compensation was not seen in children with obesity due to a decreased ability to modulate conflict-monitoring. The larger task-evoked conflicts and decreased ability in modulate conflict-monitoring mechanism in children with overweight and obesity may reduce efficiency of concomitant processing streams hindering the effective modulation of attentional resource allocation signified by the P3-ERP component. The P3 is elicited between 300 and 700 ms after stimulus onset and is indicative of attentional engagement in the stimulus environment (reflected in the magnitude of the P3 potential) and cognitive processing speed (indexed by the timing of the P3 potential) (Polich, 2007). Data from Kamijo et al. (2012b) found that normal weight children had a more frontally distributed P3 during trials requiring greater inhibitory control relative to trials with low inhibitory control demands, whereas overweight or obese children had similar topographic scalp distributions between trials with low and high inhibitory control demands, suggesting that overweight or obesity children were less capable of flexibly allocating attentional resources between tasks that varied in their inhibitory control requirements. Similar findings were found by Alatorre-Cruz et al. (2021) and Tsai et al. (2016), where ERP data indicated smaller P3 amplitude at the posterior site in obese children relative to their normal-weight counterparts during an inhibitory control (Alatorre-Cruz et al., 2021) or a visuospatial attention task (Tsai et al., 2016). Collectively, these N2- and P3-ERP findings indicate that, relative to normal weight children, who are able to more flexibly modulate attentional resources allocation based on inhibitory control demands, obese children have greater task-evoked conflict along with less flexible attentional adjustment when cognitive demands increase, which may be a result of naturally biasing their responses toward task components with low cognitive demands.
In addition to adiposity-related differences in ERP indices of stimulus processing, adiposity also appears to influence ERP indices of response execution, including action monitoring and motor preparation. Specifically, error-related negativity (ERN) is an ERP component that is thought to reflect the action monitoring system, with larger amplitude following an error response that reflects better implementation of top-down cognitive control and behavior adjustment (Gehring et al., 1993). Kamijo et al. (2014) demonstrated that obese children had smaller ERN amplitude, along with poorer post-error response accuracy, compared to their normal weight counterparts. Such findings imply a maladaptive relationship between excess adiposity and action monitoring that may reflect slower development of the prefrontal-cingulate network (Kamijo et al., 2014). Moreover, Walk and colleagues (2020) indicated that children with greater whole body %fat have lower amplitude of the lateralized-readiness potential (LRP), an ERP component reflecting neural resource allocation during motor preparation (Hsieh, 2006). Such findings were observed during task components requiring the upregulation of inhibitory control, suggesting that children with greater adiposity were unable to recruit sufficient neural resources to support response preparation. Additionally, whole body %fat was negatively related to the onset of the LRP during task trials with lower inhibitory control demands, implying that children with greater adiposity have a prolonged window of time between motor response activation and the motor movement itself. The ERN and LRP findings, collectively, indicate that obesity appears to be associated with poorer behavioral adjustment following an error response and failures in motor response preparation in preadolescent children.
Cognition
Task Performance
Cross-sectional investigations have pointed to a negative association between excess adiposity and performance on higher-order cognitive operations. For example, in preadolescent children, Chojnacki et al. (2018) and Kamijo et al. (2012a) observed a relationship between increased adiposity (measured via a DXA scan) and poorer inhibitory control, an aspect of executive function that describes the ability to suppress task irrelevant information in the stimulus environment and halt an ongoing but undesirable behavioral response (Wöstmann et al., 2013). The results indicated that higher BMI (Kamijo et al., 2012a), greater whole body %fat (Chojnacki et al., 2018; Kamijo et al., 2012a), and greater central adiposity (Kamijo et al., 2012a) were inversely related to performance on tasks that modulated inhibitory control, as reflected by lower response accuracy during task components requiring greater amounts of inhibitory control (Kamijo et al., 2012a) and greater response time variability, a measure of response stability (Chojnacki et al., 2018). Analogous findings were reported by Scudder et al. (2015), who examined risk factors of metabolic syndrome (MetS) on inhibitory control. MetS risk factors included (1) high-density lipoprotein cholesterol < 50 mg/dL, (2) waist circumference > 75th percentile scores, (3) systolic and/or diastolic blood pressure > 90th percentile scores, (4) triglyceride > 100 mg/dL, and (5) fasting blood glucose > 110 mg/dL. Group comparisons indicated that children without any MetS risk factors demonstrated overall faster response speed than the at-risk children, who met at least one of the abovementioned risk criteria. In addition, at-risk children experienced larger failures of inhibition (i.e., reduced response accuracy) between task-relevant and task-irrelevant information (Scudder et al., 2015).
The negative relationship of excess adiposity can be extended to other aspects of cognition, including relational memory (i.e., often termed: associative memory), which is hippocampal-dependent. Specifically, in preadolescent children, research has associated excess adiposity with both hippocampal-dependent and hippocampal-independent (i.e., item recall) memory (Hassevoort et al., 2017; Khan et al., 2015). Relational memory refers to the ability to bind information together into memory including the relationship among constituent elements of an experience, such as co-occurrences of people, places, and/or objects and their spatial and temporal context, which is thought to be hippocampal-dependent (Konkel & Cohen, 2009). Item memory, by contrast, requires no binding of memory between related representations but simply their recall. This cognitive domain requires modest engagement of the hippocampus (Sullivan Giovanello et al., 2004). The existing data suggests that greater central adiposity is associated with poorer accuracy for relational memory tasks in overweight and obese children. Such an inverse relationship, however, was not seen in item memory, suggesting a selectively negative influence of central adiposity on hippocampal-dependent memory. These findings, which stem from behavioral outcomes of task engagement, provide support for prefrontal- and hippocampal-dependent cognition as the most vulnerable to increased adiposity in children.
Academic Achievement
The negative effects of increased adiposity have been further extended to academic achievement, an overall measure of neurocognitive health and integrity that also provides insight into real-world cognitive performance (Martin et al., 2017; Santana et al., 2017). Research has shown a close relationship between children’s academic performance and higher-order cognition, including inhibitory control (Hillman et al., 2012) and relational memory (Hassevoort et al., 2018), and its associated structural (Chaddock-Heyman et al., 2015; Cheema & Cummine, 2018) and functional (Chaddock-Heyman et al., 2018; Westfall et al., 2020) modulation. Hence, it is not surprising that the negative effects of adiposity extend to scholastic performance. For example, Kamijo et al. (2012a) were the first to indicate that greater BMI, whole body %fat, and abdominal fat mass are associated with lower performance on academic achievements tests of reading, spelling and mathematics. Such findings were supported by Raine et al. (2018), who showed that obese children had lower performance on tests of reading and math than their normal-weight peers. Further, these relationships may begin early in childhood, as Khan et al. (2020) recently found that greater VAT was associated with poorer early academic skills, including reading-writing ability and oral language performance in a group of preschoolers. Such preliminary evidence is suggestive of a negative effect of increased adiposity (i.e., central adiposity in particular) on various academic skills in children.
Summary
In short, the current state of the literature suggests a negative relationship of obesity and excess adiposity on cognitive and brain health on structural, functional, and behavioral correlates of executive function and memory. The negative effects of obesity are extended to poorer performance in multiple academic outcomes. The negative effects may be triggered by central inflammation induced by the over-secretion of proinflammatory adipokines/cytokines, increased insulin resistance, and cerebrovascular abnormalities.
The Beneficial Role of Physical Activity on Brain and Cognition in Children with Obesity
Despite the known negative effects of obesity on brain, cognition, and academic performance in children, there is a growing body of evidence supporting physical activity as an effective means to counteract, in part, obesity-related impairments during childhood (Davis et al., 2011; Krafft et al., 2014c; Liu et al., 2018; Logan et al., 2021; Raine et al., 2017). Physical activity refers to any bodily movement produced by skeletal muscles that requires energy expenditure (Donnelly et al., 2016). Fitness, on the other hand, is a physiological state of well-being that reduces the risk of hypokinetic disease, a basis for participation in sports, and good health, which enables one to complete the tasks of daily living. Subcomponents of fitness include aerobic fitness, muscle strength and endurance, and flexibility (Donnelly et al., 2016). Recent studies also shed light on motor coordination, another domain of fitness, and its association with brain health given the close relationship between motor and cognitive development during childhood (Diamond, 2000), Motor coordination represents the degree of proficiency in performing a wide variety of motor skills including both gross (e.g., jumping, hand–eye coordination) and fine (e.g., manual dexterity, precision) motor skills as well as the underlying mechanisms including coordination, control, and quality of movement (Haga, 2008). The ensuing section summarizes the relationship of physical activity, physical fitness, and motor coordination on brain and cognition from a behavioral, structural, and functional level. We further summarize preliminary evidence regarding the association of physical activity and fitness on scholastic performance in children with excess body mass. Figure 2 depicts how physical activity may alleviate the negative influence of excess adiposity and obesity on brain, cognition, and academic performance in children.
Possible Mechanisms
Although structural and functional findings provide markers of cognition, molecular mechanisms underlying physical activity effects provide a more detailed understanding of neural alterations after intervention in overweight or obese children. As such, rodent models have indicated that aerobic exercise decreases the secretion of proinflammatory cytokines (e.g., IL-1), which may, in turn, result in attenuated central inflammation, decreased oxidative stress in the brain, and eventually normalized synaptic plasticity and cortical growth (Erion et al., 2014). Similarly, human research found that aerobic exercise decreases plasma proinflammatory cytokines (i.e., CRP, IL-6, leptin) and attenuates insulin resistance in individuals with overweight or obesity (Many et al., 2013; Trachta et al., 2014). Importantly, research has indicated the mediating role of insulin resistance on the relationship between aerobic fitness and memory. That is, increased aerobic fitness may favor memory performance via decreased insulin resistance (Tarumi et al., 2013). This finding has been expanded by a study showing close relationships between increased aerobic fitness, increased insulin sensitivity, and greater cortical thickness in the frontal lobes in adolescent children, with higher insulin sensitivity showing stronger association with frontal cortical thickness (Ross et al., 2015). Considering that insulin resistance is a major cause of vascular and endothelial dysfunctions in cortical areas (Miller & Spencer, 2014; Willette & Kapogiannis, 2015; Yates et al., 2012), the mediating role of insulin resistance is not surprising. On the other hand, one recent study in children with overweight and obesity found that higher levels of daily moderate-to-vigorous physical activity, as assessed by accelerometry, was related to higher plasma BDNF levels (Mora-Gonzalez et al., 2019c). Findings from that study imply that, in children with overweight and obesity, greater amounts of daily physical activity are associated with increased expression of neurotrophic factors, such as BDNF. The above findings suggest that physical activity may counteract the detrimental effects of obesity and adiposity on brain functioning and cognition via (a) decreased secretion of proinflammatory cytokines (and thereby attenuated central inflammation and oxidative stress in the brain), (b) increased insulin sensitivity (and therefore normalized vascular and endothelial functions), and (c) increased expression of neurotrophic factors that favor neural growth and plasticity. However, it should be noted that the majority of findings stem from either animal models or cross-sectional human studies, data from studies using a RCT design in children with overweight and/or obesity are needed to provide a clearer picture of neural and molecular mechanisms underlying the effects of physical activity in childhood obesity.
Brain Structure
As indicated above, increased adiposity has detrimental effects on gray matter volume and white matter integrity, particularly in the prefrontal cortex and hippocampus (Marsland et al., 2015; Takeda et al., 2014; Wickman et al., 2013). Fortunately, data stemming from DTI has indicated a positive influence of physical activity on structural integrity of white matter in children with overweight and obesity. The majority of data stem from cross-sectional research (Esteban-Cornejo et al., 2019b; Rodriguez-Ayllon et al., 2020). For example, the current state of the literature suggests that increased aerobic fitness measured by a field-based shuttle run test and motor-coordination fitness (e.g., coordination, speed-agility) are associated with white matter coherence in fiber tracts (i.e., superior and inferior longitudinal fasciculus) linking frontal-parietal, parietal-occipital, and temporal lobes (Esteban-Cornejo et al., 2019b), but not global white matter integrity (Rodriguez-Ayllon et al., 2020). In addition, upper-limb muscular strength was associated with white matter integrity within the left lateral frontal lobe (Rodriguez-Ayllon et al., 2020), thalamic radiations, and projection fiber tracts linking fronto-cingulate regions (Esteban-Cornejo et al., 2019b). Using structural MRI, a few cross-sectional studies have indicated that increased aerobic and motor-coordination fitness, but not muscular fitness, are associated with greater gray matter volume in frontal, temporal, and hippocampal regions as well as greater global cortical thickness (Esteban-Cornejo et al., 2017). In fact, it has recently been reported that the overall brain volume is larger in fit children with overweight/obesity than in their unfit peers (Cadenas-Sanchez et al., 2020a). Notably, decreased adiposity appears to mediate the relationship between increased fitness and greater cortical thickness (Esteban-Cornejo et al., 2019a). Please see Table 1 for details of abovementioned cross-sectional studies.
Furthermore, by implementing 8 months of a multifaceted after-school physical activity intervention (running games, jump rope), Krafft et al. (2014b) and Schaeffer et al. (2014) found improved white matter structural coherence and myelination in the uncinate fasciculus (Schaeffer et al., 2014), a white matter tract linking the dorsolateral prefrontal cortex and hippocampus (Schmahmann et al., 2007), and the superior longitudinal fasciculus (Krafft et al., 2014b), which links the frontal-parietal network governing executive function (Østby et al., 2011; Vestergaard et al., 2010). Interestingly, Krafft et al. (2014b) further indicated a dose-related effect within the exercise group, such that better attendance, higher intensity (reflected by in-exercise HR), and a greater total dose of exercise (reflected by attendance x in-exercise HR) were associated with greater changes in white matter integrity. Collectively, structural data corroborate the behavioral data indicating that aerobic and motor-coordination fitness are relevant components embedded into physical activity which foster structural integrity in brain regions that are vulnerable to obesity (e.g., frontal, temporal regions), as well as regions that are closely related to attention and executive function (e.g., frontal-parietal and frontal-cingulate regions). There is also preliminary evidence indicating that muscular strength appears to be a relevant means to support regional white matter integrity, but the current data remains contradictory. For further information of abovementioned RCT studies, please see Table 2.
Brain Function
Neuroimaging research using EEG and functional MRI (fMRI) has supported a positive influence of physical activity or fitness on brain functioning in children with overweight and obesity. For example, cross-sectional data indicate that higher aerobic fitness and better motor-coordination (measured by speed-agility performance) are associated with larger P3 amplitude during task components modulating inhibitory control and working memory, suggesting increased activation of neural networks underlying attentional engagement during task components with varied amounts of inhibitory control (Mora-Gonzalez et al., 2020) or working memory requirements (Mora-Gonzalez et al., 2019b). Higher speed-agility fitness was also associated with shorter P3 latency during a working memory task, indicating faster stimulus processing speed (Mora-Gonzalez et al., 2019b). The positive association of aerobic fitness and motor-coordination with the P3-ERP is supported by findings from a 9-month RCT where overweight or obese children who underwent an aerobic- and motor coordination-based intervention showed sustained P3 amplitude over time, along with sustained inhibitory control performance, whereas overweight or obese children in the waitlist control group showed decreased P3 amplitude from pre- to post-test despite no change in task performance (Logan et al., 2021). Such findings corroborate cross-sectional data which suggest that physical activity may be relevant to maintain brain functioning during inhibitory control in children with overweight or obesity. In contrast, a few studies point to an association between muscular strength and P3-ERP, with greater muscular strength (measured by upper-limb strength) found to be associated with larger P3 amplitude during a working memory task (Mora-Gonzalez et al., 2019b), but not during an inhibitory control task (Mora-Gonzalez et al., 2020). These findings, together, suggest that the association of fitness with neuroelectric outcomes of cognition in overweight and obese children may be dependent upon the specific aspect of fitness enhanced by intervention and/or aspect of cognition assessed (please see Table 1 and Table 2 for further information of abovementioned cross-sectional studies and intervention study, respectively).
By way of contrast, the current data on the association of objectively measured physical activity (using accelerometry) and P3-ERP is rather contradictory (see Table 1 for more details). Unlike intervention studies in which children’s physical activity behavior is increased beyond their normal physical activity patterns, studies using objectively measured physical activity assess children’s daily, lifestyle-based physical activity. Specifically, data from Mora-Gonzalez et al. (2020) indicated that higher vigorous physical activity was associated with larger P3 amplitude during trials with greater inhibitory control, but this relation disappeared upon adjusting for aerobic fitness; further, higher moderate and moderate-to-vigorous physical activity were found to be associated with longer P3 latency during an inhibitory control task. In contrast, no association was found between objectively measured physical activity and P3-ERP during a working memory task (Mora-Gonzalez et al., 2019b).
Research assessing resting-state fMRI measures revealed that overweight and obese children with greater fitness had more favorable resting-state hippocampal connectivity (Table 1). Specifically, using the resting-state blood oxygenation level dependent (BOLD) signal from fMRI, Esteban-Cornejo and colleagues (2021) found that overweight and obese children with greater aerobic fitness had greater connectivity between the anterior hippocampus and the frontal regions, and increased motor-coordination was associated with diminished connectivity between the posterior hippocampus and frontal regions. These differences in frontal-hippocampal connectivity were attributed to regional specificities of aerobic fitness and motor coordination. That is, data from rodent models support the role of aerobic exercise on neurogenesis in the frontal hippocampus (i.e., the dentate gyrus) (van Praag et al., 2005), whereas motor activity appears to increase synaptic activity in the cerebellar cortex (Black et al., 1990). It is therefore reasonable to speculate that the role of motor fitness on synaptogenesis may spread to the posterior hippocampus. These findings suggest a favorable albeit differential effects of aerobic versus motor-coordination on functional connectivity between frontal regions and the hippocampus (Esteban-Cornejo et al., 2021). In contrast, Esteban-Cornejo and colleagues did not find a relation between increased muscular strength and hippocampal functional connectivity at a resting state (Table 1).
Further, Krafft et al. (2014a) randomly assigned children who were overweight or obese to either an 8-month physical activity intervention (running games, jump rope; 40 min per session, 5 session per week) or an active control intervention (instructor-led attention games), and found that physical activity resulted in decreased spatial synchrony (i.e., decreased coherence of BOLD activation between cortices within specific brain networks) over time in the default-mode network (medial prefrontal cortex, anterior and posterior cingulate cortex, inferior parietal cortex), the executive function network (prefrontal and parietal cortex), and the motor network (supplementary and primary motor cortex, thalamus, putamen, cerebellum) during resting state (see Table 2 for more details), implying better cortical specialization (decreased between-network synchrony and increased within-network synchrony) and better cortical maturation (Kannurpatti et al., 2012; Rubia, 2013) as a function of physical activity. Furthermore, studies assessing BOLD signal changes during executive function tasks revealed that overweight children who underwent physical activity intervention had better in-task cortical resource recruitment, particularly in the prefrontal cortex (Table 2). That is, Davis et al. (2011) found that overweight children who engaged into a 3-month vigorous aerobic- and motor coordination-based physical activity intervention (running games, basketball drills, soccer drills, jump rope; 5 sessions per week), with 20 to 40 min per session, had increased bilateral prefrontal activation and decreased bilateral parietal activation during an inhibitory control-related task, suggesting that multifaceted physical activity facilitates prefrontal development and prefrontal cortical recruitment in overweight children (Davis et al., 2011). In addition, Krafft et al. (2014c) found differential physical activity-induced effects on task performance and brain functioning. In their study, overweight children were randomly assigned to either an 8-month physical activity intervention (running games, jump rope) or an active control intervention. The results indicated that, compared to the active control group, the exercise group showed decreased BOLD activation in brain regions supporting attentional performance (i.e., precentral gyrus, posterior parietal cortex) and increased activation in regions supporting inhibitory control (i.e., anterior cingulate, superior frontal gyrus). Both groups showed improved task performance over time (Table 2). These findings suggest that 8 months of physical activity alters cortical efficiency or favors neural circuitry supporting attention and inhibitory control (e.g., fronto-cingulate area) without changing overt task performance in children with overweight. Taken together, findings from fMRI studies generally corroborate findings from ERP studies and highlight the relevance of an aerobic- and motor coordination-based physical activity program to resting-state and in-task cortical functioning in overweight and obese children.
Cognition
Task Performance
A growing body of literature has begun to investigate the effects of physical activity and fitness on behavioral outcomes of cognition in children with overweight and obesity with either cross-sectional (Davis & Cooper, 2011; Mora-Gonzalez et al., 2019a, 2019b, 2020; Table 1) or interventional design (Crova et al., 2014; Gallotta et al., 2015; Liu et al., 2018; Raine et al., 2017; Table 2). While one cross-sectional study showed a null association between objectively measured physical activity and performance on executive function tasks (Mora-Gonzalez et al., 2019a), the majority of studies point to a positive relationship of aerobic fitness (measured by VO2peak or performance on a 20-m shuttle run test; Davis & Cooper, 2011; Mora-Gonzalez et al., 2019b; Mora-Gonzalez et al., 2020) and motor-coordination (measured by speed-agility performance; Mora-Gonzalez et al., 2019a, 2019b, 2020) on inhibitory control (Davis & Cooper, 2011; Mora-Gonzalez et al., 2020), working memory (Mora-Gonzalez et al., 2019b), and cognitive flexibility (Mora-Gonzalez et al., 2019a) tasks; the latter of which is an aspect of executive function involved in the adjustment of attention allocation between two distinct mental representations and/or rule sets. Others have also found significant associations of aerobic fitness (Davis & Cooper, 2011) and muscular strength (measured by handgrip strength; Mora-Gonzalez et al., 2019a) with planning, a higher-order executive function involved in maintaining task-relevant information in mind while organizing and adjusting goal-directed actions simultaneously (Dehaene & Changeux, 1997; Polk et al., 2002).
The positive relationship between fitness and executive function in children with overweight and obesity has been further supported by RCTs to test the effects of a structured moderate-to-vigorous physical activity intervention. For example, Crova et al. (2014) randomly assigned overweight children into either a 6-month physical education program including cognitively demanding exercise (curricular physical education + additional hours of skill-based and tennis-specific training) or curricular physical education only, with one session per week. Results showed that overweight children had more pronounced pre- to post-intervention improvements in inhibitory control than their normal-weight counterparts only if involved in the enhanced physical activity program, and such an intervention effect was not mediated by changes in aerobic fitness. The authors concluded that the cognitive and social interaction components inherent in the enhanced physical activity program, even when embedded in a lower dose (one session per week), may represent an effective means to promote inhibitory control in overweight children. However, results from Crova et al. may have been confounded by either greater physical activity time in the enhanced physical activity program (i.e., 58% of intervention time in contrast to 46% of intervention time in the curricular physical education intervention) or the addition of cognitive and social intervention components on top of curricular physical activity. In contrast, Gallotta et al. (2015) controlled both the physical activity dose and session duration in their random assignment of overweight and obese children into two school-based interventions: traditional physical activity (aerobic circuit training, shuttle run) and coordinative physical activity (basketball mini-games and drills). Sustained attention was assessed before and after 5 months of intervention. The authors found that while both physical activity groups improved sustained attention, the coordinative physical activity had stronger facilitative effect, implying that an aerobic- and motor coordination-based physical activity intervention may be an effective means of fostering attention performance in overweight or obese children. Interestingly, by manipulating the duration of intervention (40 min per session vs. 20 min per session), Davis and colleagues (2007) only found facilitative effects of a 40-min session of vigorous aerobic- and motor coordination-based intervention (running games, basketball drills, soccer drills, jump rope) over a 3-month period on planning performance. Such an effect was not observed in the 20-min session intervention in overweight children, suggesting a “threshold effect” of physical activity in modulating behavioral outcomes of cognition.
To better characterize whether changes in task performance are associated with changes in adiposity following physical activity intervention, a few RCTs expanded previous findings by showing an inherent relationship between energy expenditure, adiposity, and cognition. For example, Raine et al. (2017) was the first to test whether changes in adiposity and specific types of adipose tissue were related to the effectiveness of a physical activity intervention on changes in cognition. Obese children were randomly assigned to a 9-month, after-school aerobic- and motor coordination-based physical activity intervention or a waitlist control group, with 5 sessions per week. Following the 9-month physical activity intervention, children exhibited a reduction in whole body %fat as well as VAT. Further, the degree of reduction in VAT was related to the degree of gain in inhibitory control in obese children. Similarly, in overweight or obese adolescents, Liu et al. (2018) randomly assigned participants into either a 4-month motor-coordination exercise program or a waitlist control group. The exercise program involved an after-school multifaceted jump rope program performed twice weekly. The authors found that the jump rope group had improved inhibitory control, along with improved aerobic and muscular fitness, and decreased BMI. However, pre- to post-intervention change in aerobic fitness, muscular fitness, and BMI did not mediate enhanced inhibitory control performance. Together, research incorporating behavioral outcomes of cognition support the positive influence of physical activity, aerobic fitness, and motor coordination on cognition in children with overweight and obesity, with a few studies supporting the inherent relationships between increased physical activity, decreased adiposity, and improved cognition (Raine et al., 2017). Preliminary data also indicated the potential of muscular fitness for further investigation.
Academic Achievement
To date, only a few studies examined the association between physical activity, fitness, and academic achievements in children with overweight and obesity (Cadenas-Sanchez et al., 2020b; Davis & Cooper, 2011; García‐Hermoso et al., 2021; Table 1). Cadenas-Sanchez and colleagues (2020b) examined the association between objectively measured physical activity and academic achievements but found no signification associations. In contrast, a few studies have demonstrated a positive association of fitness with academic achievement. For example, Davis and Cooper (2011) found a positive association of aerobic fitness with reading and math performance in overweight children. In addition, Cadenas-Sanchez and colleagues (2020a) replicated findings from Davis and Cooper (2011) and extended aerobic, muscular strength (measured by handgrip strength), and speed-agility fitness with language skills, and further found that muscular fitness was correlated with mathematics skills as well as natural and social sciences. However, it should be noted that the significant associations for muscular strength and speed-agility were attenuated and disappeared after additional adjustments for BMI and aerobic fitness, suggesting that the two fitness dimensions did not independently associate with academic skills. One recent longitudinal study supported a positive relationship between aerobic fitness and academic achievement in overweight and obese children, wherein increased aerobic fitness over a 2-year period alleviated the negative effects of increased BMI on language, mathematics, and grade point average (García‐Hermoso et al., 2021). These preliminary data, collectively, point to a positive effect of increased fitness on various academic skills in children, especially for aerobic fitness. However, to date, there is no study in the extant literature using an interventional design to test whether increased fitness and/or decreased adiposity induced by a physical activity intervention results in improved academic achievement in children with overweight and obesity. Preliminary data from Davis and colleagues (Davis et al., 2011) found facilitative effects of a 40-min session, not a 20-min session, of vigorous aerobic- and motor coordination-based intervention (running games, basketball drills, soccer drills, jump rope) over a 3-month period on math performance (Table 2). This finding corroborates data from behavioral measures and, again, may imply a “threshold effect” of exercise dose. Nevertheless, since this study did not collect data on fitness or adiposity, whether changes in fitness induced by physical activity would be associated improved academic performance remains underexplored.
Summary
In summary, the current state of literature supports a positive effect of chronic physical activity, ranging from 3 to 9 months, across different subdomains of cognition at a structural, functional, and behavioral level. There is also preliminary data supporting a positive influence of increased fitness on academic achievement in children with overweight or obesity. Such mitigating effects of physical activity may be underpinned by decreased secretion of proinflammatory cytokines, increased insulin sensitivity, and increased expression of neurotrophic factors in association with increased energy expenditure or decreased adiposity. Of note, aerobic fitness (e.g., running) and motor coordination (e.g., speed of movement, agility, coordination) could be two relevant fitness dimensions integrated into physical activity interventions, whereas the impact of muscular fitness remains underexplored. Further, a multifaceted physical activity intervention of moderate-to-vigorous intensity could be most effective in manifesting the physical activity-related benefits. Lastly, it is noteworthy that physical activity may have a “threshold effect” of the exercise dose on behavioral and academic outcomes, such that longer sessions of physical activity (e.g., 40 min) may manifest larger benefits relative to shorter sessions (e.g., 20 min).
Future Research Directions
While we have learned much over the years about the relationship of physical activity and fitness on cognitive and brain health in children with overweight or obesity, there are still many questions worth investigating. First, the majority of studies in this line of research only recruited overweight and/or obese children, with only four studies additionally recruiting normal weight children for comparison (Crova et al., 2014; Gallotta et al., 2015; Logan et al., 2021; Raine et al., 2017). Preliminary findings have pointed to differential modulations of physical activity to behavioral (Crova et al., 2014) and neuroelectric outcomes of inhibitory control in overweight and obese children (Logan et al., 2021), such that physical activity has larger effects in overweight and obese children than their normal-weight peers (Crova et al., 2014; Logan et al., 2021). More research focusing on other subdomains of cognition are needed to better elucidate the moderating role of obesity/adiposity.
Second, more research employing a broader measure of cognition as well as academic achievement is needed. The current state of the literature exclusively focused on executive function (i.e., inhibitory control, working memory, cognitive flexibility) and the planning aspect of cognition, leaving the effects of physical activity and fitness on other subdomains of cognition that are vulnerable to increased adiposity (e.g., hippocampal-dependent relational memory; Khan et al., 2015) unclear. Also, it remains unclear regarding the modulatory effects of physical activity and fitness on several neuroelectric correlates of cognition, including the N2, ERN, and LRP component from ERP (Kamijo et al., 2012b; Kamijo et al., 2014; Walk et al., 2020), in children with overweight and/or obesity. Moreover, as noted above, only three studies (Davis & Cooper, 2011; Cadenez-Sanchez et al., 2020b; García‐Hermoso et al., 2021) examined the association of fitness and academic achievements in childhood obesity. More research is needed to strengthen the educational and practical implications of physical activity as an effective means to prevent and manage childhood obesity and its associated negative impact on health and learning.
Third, it should be noted that most previous studies did not have measures on obesity and/or adiposity. As such, it remains unclear whether physical activity improved brain function and cognition via changes in obesity/adiposity, which limits the interpretation to a causal relationship between physical activity, adiposity, and cognition. Further, in studies who took measures on obesity and/or adiposity, there is a lack of coherence between changes in adiposity and changes in cognition following intervention. While a few studies demonstrated that changes in adiposity/obesity are associated with changes in cognition following months of physical activity intervention (Raine et al., 2017), others found either no association between changes in obesity and changes in cognition (Liu et al., 2018; Schaeffer et al., 2014) or no change in obesity following intervention despite improved neurocognitive function (Gallotta et al., 2015; Krafft et al., 2014b). One reason for the lack of coherence could be that the majority of research only included BMI and/or whole body %fat as a measure of obesity/adiposity, and thus it is possible that BMI or whole body %fat is not a sensitive marker of increased energy expenditure or changes in cognition. In contrast, measures such as VAT and abdominal fat mass may be a more sensitive marker. This assumption may be supported by findings from Raine et al. (2018), who showed that whole body %fat and SAAT were not related to cognitive performance in obese children; rather, higher VAT, which is associated with increased central inflammation and insulin resistance (Doupis et al., 2011), was associated with poorer intellectual abilities and cognitive performance. With this in mind, future research should include VAT and/or abdominal fat measures to better characterize the association between changes in adiposity and changes in cognition following intervention.
Fourth, despite ample data indicating that physical activity incorporating aerobic fitness and motor coordination have facilitative effects on behavioral, structural, and functional neural correlates of cognition in childhood obesity, the effects of muscular fitness remains underexplored, with no intervention study incorporating this fitness dimension and the evidence remains inconsistent across cross-sectional studies. Given that lean body mass is associated with neurocognitive integrity (Gracia‐Marco et al., 2020) and insulin levels (Torres-Costoso et al., 2017), it is worthwhile to investigate if physical activity tapping muscular fitness could increase lean body mass and insulin sensitivity, whereby improve neurocognitive function in children with obesity. Likewise, high-intensity interval training (HIIT) that consists of repeated bouts of vigorous exercise, interspersed by short periods of recovery, has recently been recommended as an effective means to decrease adiposity (Andreato et al., 2019) and facilitate performance of different subdomains of cognition in children (Hsieh et al., 2021). Considering that the relationships of fitness and physical activity to neurocognitive function in childhood obesity may be fitness-dependent, it could be informative to examine whether manipulations of physical activity characteristics (e.g., intensity, mode, duration, fitness dimension tapped) moderate the physical activity-induced neurocognitive changes. Notably, given that children with overweight and obesity may be less motivated and have lower adherence to physical activity (Alberga et al., 2013), it might be worthwhile to increase the diversity and enjoyability of exercise interventions by incorporating other activities (e.g., dual-tasking, cognitive games), rather than implementing exercise alone, when investigating the effects of manipulations of physical activity characteristics.
Fifth, despite the extant literature does not support a positive association between objectively measured physical activity with executive function, brain function, or academic achievements in children with overweight and obesity, we argue that more studies in this regard are needed given that most of the existing research are stemming from the same dataset (Cadenas-Sanchez et al., 2020b; Mora-Gonzalez et al., 2019a, 2019b, 2020). Further, objectively measured physical activity may be advantageous as it represents children’s daily, lifestyle-based physical activity, which provides an accurate measure of children’s typical, daily activity patterns without additional activities imposed by interventions. As such, more research incorporates objectively measured physical activity, along with measures on physical fitness and motor coordination, would better clarify the associations between daily physical activity, fitness, and cognition in children with overweight and obesity.
Lastly, the molecular mechanisms underlying physical activity effects on cognition and brain function remain underexplored. Despite preliminary data pointing to several possible tangible biomarkers (e.g., proinflammatory cytokines, insulin, BDNF), more research with an inter-disciplinary approach that also includes obesity-related biomarkers may expand the current knowledge base by examining the mediating effects of molecular changes in the association between physical activity and neurocognitive function in childhood obesity. A better understanding of the role of these biomarkers may be informative for the development of effective physical activity regimens in children with obesity.
Conclusion
The aim of current narrative review was to consider the recent empirical evidence pertinent to the associations of chronic physical activity and fitness on brain and cognition in children with overweight or obesity. The contribution of this review is an up-to-date and comprehensive consideration of cognitive and academic outcomes, brain structure, and brain function. In summary, the current state of literature points to a detrimental effect of obesity/adiposity on behavioral, structural, and functional correlates of cognition during childhood, especially in cognitive domains that are prefrontal- or hippocampal-dependent. Preliminary data also extended this negative effect to academic achievement. Such negative effects may be undermined by central inflammation and insulin resistance induced by excessive adiposity. Fortunately, a growing body of evidence supports a positive effect of physical activity, especially interventions tapping aerobic fitness and motor coordination, across different subdomains of cognition at a brain, behavioral, and academic level in children with overweight and obesity, including cognitive indices that are shown to be vulnerable to obesity. A piecemeal of research further indicates an association between increased fitness and better performance across multiple academic subjects. Such mitigating effects of physical activity could be accounted for by decreased secretion of proinflammatory cytokines, increased insulin sensitivity, and increased expression of neurotrophic factors in association of increased energy expenditure or decreased adiposity. This area should be expanded via the further exploration of individual differences (e.g., obese children vs. normal weight children), the manipulation of physical activity characteristics, the employment of a broader array of cognitive and academic measures, the inclusion of adiposity measures that are sensitive to neurocognitive function, and the utilization of an inter-disciplinary approach. It should be noted that, however, the narrative nature of this review precludes estimation of the size of effects of either childhood obesity or chronic physical activity on brain and cognition. Future systematic and/or meta-analytical review that provide a better estimation of the effects of childhood obesity as well as the effects of chronic physical activity on brain and cognition in children with overweight/obesity is needed.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Alatorre-Cruz, G. C., Downs, H., Hagood, D., Sorensen, S. T., Williams, D. K., & Larson-Prior, L. (2021). Effect of obesity on inhibitory control in preadolescents during stop-signal task. An event-related potentials study. International Journal of Psychophysiology, 165, 56–67.
Alberga, A. S., Medd, E. R., Adamo, K. B., Goldfield, G. S., Prud’homme, D., Kenny, G. P., & Sigal, R. J. (2013). Top 10 practical lessons learned from physical activity interventions in overweight and obese children and adolescents. Applied Physiology, Nutrition, and Metabolism, 38(3), 249–258.
Alosco, M. L., Brickman, A. M., Spitznagel, M. B., Griffith, E. Y., Narkhede, A., Raz, N., ... & Gunstad, J. (2013). Independent and interactive effects of blood pressure and cardiac function on brain volume and white matter hyperintensities in heart failure. Journal of the American Society of Hypertension, 7(5), 336-343.
Alosco, M. L., Stanek, K. M., Galioto, R., Korgaonkar, M. S., Grieve, S. M., Brickman, A. M., ... & Gunstad, J. (2014). Body mass index and brain structure in healthy children and adolescents. International Journal of Neuroscience, 124(1), 49-55.
Andreato, L. V., Esteves, J. V., Coimbra, D. R., Moraes, A. J. P., & de Carvalho, T. (2019). The influence of high-intensity interval training on anthropometric variables of adults with overweight or obesity: A systematic review and network meta-analysis. Obesity Reviews, 20(1), 142–155.
Black, J. E., Isaacs, K. R., Anderson, B. J., Alcantara, A. A., & Greenough, W. T. (1990). Learning causes synaptogenesis, whereas motor activity causes angiogenesis, in cerebellar cortex of adult rats. Proceedings of the National Academy of Sciences, 87(14), 5568–5572.
Cadenas-Sanchez, C., Migueles, J. H., Erickson, K. I., Esteban-Cornejo, I., Catena, A., & Ortega, F. B. (2020a). Do fitter kids have bigger brains? Scandinavian Journal of Medicine & Science in Sports, 30(12), 2498–2502.
Cadenas-Sanchez, C., Migueles, J. H., Esteban-Cornejo, I., Mora-Gonzalez, J., Henriksson, P., Rodriguez-Ayllon, M., ... & Catena, A. (2020b). Fitness, physical activity and academic achievement in overweight/obese children. Journal of Sports Sciences, 38(7), 731-740.
Caterson, I. D., & Gill, T. P. (2002). Obesity: Epidemiology and possible prevention. Best Practice and Research Clinical Endocrinology and Metabolism, 16, 595–610.
Chaddock-Heyman, L., Erickson, K. I., Kienzler, C., King, M., Pontifex, M. B., Raine, L. B., ... & Kramer, A. F. (2015). The role of aerobic fitness in cortical thickness and mathematics achievement in preadolescent children. PloS One, 10(8), e0134115.
Chaddock-Heyman, L., Weng, T. B., Kienzler, C., Erickson, K. I., Voss, M. W., Drollette, E. S., ... & Kramer, A. F. (2018). Scholastic performance and functional connectivity of brain networks in children. PloS One, 13(1): e0190073.
Chaldakov, G. N., Stankulov, I. S., Hristova, M., & Ghenev, P. I. (2003). Adipobiology of disease: Adipokines and adipokine-targeted pharmacology. Current Pharmaceutical Design, 9(12), 1023–1031.
Chang, Y. K., Chu, C. H., Chen, F. T., Hung, T. M., & Etnier, J. L. (2017). Combined effects of physical activity and obesity on cognitive function: Independent, overlapping, moderator, and mediator models. Sports Medicine, 47(3), 449–468.
Cheema, K., & Cummine, J. (2018). The relationship between white matter and reading acquisition, refinement and maintenance. Developmental Neuroscience, 40(3), 209–222.
Cheke, L. G., Bonnici, H. M., Clayton, N. S., & Simons, J. S. (2017). Obesity and insulin resistance are associated with reduced activity in core memory regions of the brain. Neuropsychologia, 96, 137–149.
Children’s Hospital of Eastern Ontario Research Institute. (2018, November 26). Childhood physical inactivity reaches crisis levels around the globe: report compares 49 countries; says 75 percent of countries have failing physical activity grades. ScienceDaily. Retrieved May 17, 2020 from www.sciencedaily.com/releases/2018/11/181126123331.htm
Chojnacki, M. R., Raine, L. B., Drollette, E. S., Scudder, M. R., Kramer, A. F., Hillman, C. H., & Khan, N. A. (2018). The negative influence of adiposity extends to intraindividual variability in cognitive control among preadolescent children. Obesity, 26(2), 405–411.
Crova, C., Struzzolino, I., Marchetti, R., Masci, I., Vannozzi, G., Forte, R., & Pesce, C. (2014). Cognitively challenging physical activity benefits executive function in overweight children. Journal of Sports Sciences, 32, 201–211.
Davis, C. L., & Cooper, S. (2011). Fitness, fatness, cognition, behavior, and academic achievement among overweight children: Do cross-sectional associations correspond to exercise trial outcomes? Preventive Medicine, 52, S65–S69.
Davis, C. L., Tomporowski, P. D., Boyle, C. A., Waller, J. L., Miller, P. H., Naglieri, J. A., & Gregoski, G. (2007). Effects of aerobic exercise on overweight children’s cognitive functioning: A randomized controlled trial. Research Quarterly for Exercise and Sport, 78, 510–519.
Davis, C. L., Tomporowski, P. D., McDowell, J. E., Austin, B. P., Miller, P. H., Yanasak, N. E., & …Naglieri, J. A. (2011). Exercise improves executive function and achievement and alters brain activation in overweight children: A randomized, controlled trial. Health Psychology, 30, 91–98.
Dehaene, S., & Changeux, J. P. (1997). A hierarchical neuronal network for planning behavior. Proceedings of the National Academy of Sciences of the United States of America, 25, 13293–13298.
Diamond, A. (2000). Close interrelation of motor development and cognitive development and of the cerebellum and prefrontal cortex. Child Development, 71(1), 44–56.
Donnelly, J. E., Hillman, C. H., Castelli, D., Etnier, J. L., Lee, S., Tomporowski, P., ... & Szabo-Reed, A. N. (2016). Physical activity, fitness, cognitive function, and academic achievement in children: a systematic review. Medicine & Science in Sports & Exercise, 48(6), 1197.
Doupis, J., Rahangdale, S., Gnardellis, C., Pena, S. E., Malhotra, A., & Veves, A. (2011). Effects of diabetes and obesity on vascular reactivity, inflammatory cytokines, and growth factors. Obesity, 19(4), 729–735.
Ebbeling, C. B., Pawlak, D. B., & Ludwig, D. S. (2002). Childhood obesity: Public-health crisis, common sense cure. Lancet, 360(9331), 473–482.
Ebbeling, C. B., & Ludwig, D. S. (2008). Tracking pediatric obesity. JAMA, 299(20), 2442–2443.
Erion, J. R., Wosiski-Kuhn, M., Dey, A., Hao, S., Davis, C. L., Pollock, N. K., & Stranahan, A. M. (2014). Obesity elicits interleukin 1-mediated deficits in hippocampal synaptic plasticity. Journal of Neuroscience, 34, 2618–2631.
Esteban-Cornejo, I., Cadenas-Sanchez, C., Contreras-Rodriguez, O., Verdejo-Roman, J., Mora-Gonzalez, J., Migueles, J. H., ... & Ortega, F. B. (2017). A whole brain volumetric approach in overweight/obese children: Examining the association with different physical fitness components and academic performance. The ActiveBrains project. NeuroImage, 159, 346-354.
Esteban-Cornejo, I., Mora-Gonzalez, J., Cadenas-Sanchez, C., Contreras-Rodriguez, O., Verdejo-Román, J., Henriksson, P., ... & Hillman, C. H. (2019a). Fitness, cortical thickness and surface area in overweight/obese children: The mediating role of body composition and relationship with intelligence. NeuroImage, 186, 771-781.
Esteban-Cornejo, I., Rodriguez-Ayllon, M., Verdejo-Roman, J., Cadenas-Sanchez, C., Mora-Gonzalez, J., Chaddock-Heyman, L., ... & Catena, A. (2019b). Physical fitness, white matter volume and academic performance in children: findings from the ActiveBrains and FITKids2 projects. Frontiers in Psychology, 10: 208.
Esteban-Cornejo, I., Stillman, C. M., Rodriguez-Ayllon, M., Kramer, A. F., Hillman, C. H., Catena, A., ... & Ortega, F. B. (2021). Physical fitness, hippocampal functional connectivity and academic performance in children with overweight/obesity: the ActiveBrains project. Brain, Behavior, and Immunity.
Freedland, E. S. (2004). Role of a critical visceral adipose tissue threshold (CVATT) in metabolic syndrome: Implications for controlling dietary carbohydrates: A review. Nutrition & Metabolism, 1(1), 1–24.
Gallotta, M. C., Emerenziani, G. P., Iazzoni, S., Meucci, M., Baldari, C., & Guidetti, L. (2015). Impacts of coordinative training on normal weight and overweight/obese children’s attentional performance. Frontiers in Human Neuroscience, 9, 577.
García‐Hermoso, A., Martinez‐Gomez, D., del Rosario Fernández‐Santos, J., Ortega, F. B., Castro‐Piñero, J., Hillman, C. H., ... & Esteban‐Cornejo, I. (2021). Longitudinal associations of physical fitness and body mass index with academic performance. Scandinavian Journal of Medicine & Science in Sports, 31(1), 184-192.
Gehring, W. J., Goss, B., Coles, M. G., Meyer, D. E., & Donchin, E. (1993). A neural system for error detection and compensation. Psychological Science, 4(6), 385–390.
Gracia‐Marco, L., Esteban‐Cornejo, I., Ubago‐Guisado, E., Rodriguez‐Ayllon, M., Mora‐Gonzalez, J., Solis‐Urra, P., ... & Ortega, F. B. (2020). Lean mass index is positively associated with white matter volumes in several brain regions in children with overweight/obesity. Pediatric Obesity, 15(5): e12604.
Haga, M. (2008). The relationship between physical fitness and motor competence in children. Child: Care, Health and Development, 34(3), 329–334.
Hassevoort, K. M., Khan, N. A., Hillman, C. H., Kramer, A. F., & Cohen, N. J. (2018). Relational memory is associated with academic achievement in preadolescent children. Trends in Neuroscience and Education, 13, 8–16.
Hassevoort, K. M., Khazoum, S. E., Walker, J. A., Barnett, S. M., Raine, L. B., Hammond, B. R., ... & Cohen, N. J. (2017). Macular carotenoids, aerobic fitness, and central adiposity are associated differentially with hippocampal-dependent relational memory in preadolescent children. Journal of Pediatrics, 183, 108-114.
Heni, M., Kullmann, S., Preissl, H., Fritsche, A., & Häring, H. U. (2015). Impaired insulin action in the human brain: Causes and metabolic consequences. Nature Reviews Endocrinology, 11(12), 701.
Hill, J. O., Wyatt, H. R., & Peters, J. C. (2012). Energy balance and obesity. Circulation, 126(1), 126–132.
Hillman, C. H., Pontifex, M. B., Motl, R. W., O’Leary, K. C., Johnson, C. R., Scudder, M. R., ... & Castelli, D. M. (2012). From ERPs to academics. Developmental Cognitive Neuroscience, 2, S90-S98.
Hsieh, S. (2006). The lateralized readiness potential and P300 of stimulus-set switching. International Journal of Psychophysiology, 60(3), 284–291.
Hsieh, S. S., Chueh, T. Y., Huang, C. J., Kao, S. C., Hillman, C. H., Chang, Y. K., & Hung, T. M. (2021). Systematic review of the acute and chronic effects of high-intensity interval training on executive function across the lifespan. Journal of Sports Sciences, 39(1), 10–22.
Kamijo, K, Khan, N. A., Pontifex, M. B., Scudder, M. R., Drollette, E. S., Raine, L. B., … Hillman, C. H. (2012a). The relation of adiposity to cognitive control and scholastic achievement in preadolescent children. Obesity, 20, 2406-2411
Kamijo, K., Pontifex, M. B., Khan, N. A., Raine, L. B., Scudder, M. R., Drollette, E. S., … Hillman, C. H. (2012b). The association of childhood obesity to neuroelectric indices of inhibition. Psychophysiology, 49, 1361-1371.
Kamijo, K., Pontifex, M. B., Khan, N. A., Raine, L. B., Scudder, M. R., Drollette, E. S., … Hillman, C. H. (2014). The negative association of childhood obesity to cognitive control of action monitoring. Cerebral Cortex, 24, 654-662
Kannurpatti, S. S., Rypma, B., & Biswal, B. B. (2012). Prediction of task-related BOLD fMRI with amplitude signatures of resting-state fMRI. Frontiers in System Neuroscience, 6, 7.
Kelly, T., Yang, W., Chen, C., Reynolds, K., & He, J. (2008). Global burden of obesity in 2005 and projections to 2030. International Journal of Obesity, 32, 1431–1437.
Khan, N. A., Baym, C. L., Monti, J. M., Raine, L. B., Drollette, E. S., Scudder, M. R., … Cohen, N. J. (2015). Central adiposity is negatively associated with hippocampal-dependent relational memory among overweight and obese children. Journal of Pediatrics, 166, 302-308.
Khan, N. A., Cannavale, C., Iwinski, S., Liu, R., McLoughlin, G. M., Steinberg, L. G., & Walk, A. M. (2020). Visceral adiposity and diet quality are differentially associated with cognitive abilities and early academic skills among preschool-age children. Frontiers in Pediatrics, 7, 548.
Konkel, A., & Cohen, N. J. (2009). Relational memory and the hippocampus: Representations and methods. Frontiers in Neuroscience, 3, 166–174.
Krafft, C. E., Pierce, J. E., Schwarz, N. F., Chi. L., Weinberger, A. L., Schaeffer, D. J., … McDowell, J. E. (2014a). An eight month randomized controlled exercise intervention alters resting state synchrony in overweight children. Neuroscience, 256, 445-455.
Krafft, C. E., Schaeffer, D. J., Schwarz, N. F., Chi. L., Weinberger, A. L., Pierce, J. E., …McDowell, J. E. (2014b). Improved fronto-parietal white matter integrity in overweight children is associated with attendance in an after-school exercise program. Developmental Neuroscience, 36, 1-9.
Krafft, C. E., Schwarz, N. F., Chi. L., Weinberger, A. L., Schaeffer, D. J., Pierce, J. E., … McDowell, J. E. (2014c). An 8-month randomized controlled exercise trial alters brain activation during cognitive tasks in overweight children. Obesity, 22, 232-242.
Kullmann, S., Schweizer, F., Veit, R., Fritsche, A., & Preissl, H. (2015). Compromised white matter integrity in obesity. Obesity Reviews, 16, 273–281.
Lambert, E. A., Straznicky, N. E., Dixon, J. B., & Lambert, G. W. (2015). Should the sympathetic nervous system be a target to improve cardiometabolic risk in obesity? American Journal of Physiology Heart and Circulatory Physiology, 309, H244–H258.
Larson, M. J., Clayson, P. E., & Clawson, A. (2014). Making sense of all the conflict: A theoretical review and critique of conflict-related ERPs. International Journal of Psychophysiology, 93(3), 283–297.
Laurent, J. S., Watts, R., Adise, S., Allgaier, N., Chaarani, B., Garavan, H., ... & Mackey, S. (2020). Associations among body mass index, cortical thickness, and executive function in children. JAMA Pediatrics, 174(2), 170-177.
Liu, J. H., Alderman, B. L., Song, T. F., Chen, F. T., Hung, T. M., & Chang, Y. K. (2018). A randomized controlled trial of coordination exercise on cognitive function in obese adolescents. Psychology of Sport and Exercise, 34, 29–38.
Logan, N. E., Raine, L. B., Drollette, E. S., Castelli, D. M., Khan, N. A., Kramer, A. F., & Hillman, C. H. (2021). The differential relationship of an afterschool physical activity intervention on brain function and cognition in children with obesity and their normal weight peers. Pediatric Obesity, 16(2), 12708.
Luck, S. J. (2014). An introduction to the event-related potential technique. MIT press.
Many, G., Hurtado, M. E., Tanner, C., Hourmard, J., Gordish-Dressman, H., Park, J. J., … Hoffman, E. (2013). Moderate-intensity aerobic training program improves insulin sensitivity and inflammatory markers in a pilot study of morbidly obese minority teens. Pediatric Exercise Science, 25, 12-26.
Marsland, A. L., Gianaros, P. J., Kuan, D. C. H., Sheu, L. K., Krajina, K., & Manuck, S. B. (2015). Brain morphology links systemic inflammation to cognitive function in midlife adults. Brain, Behavior, and Immunity, 48, 195–204.
Martin, A., Booth, J. N., Laird, Y., Sproule, J., Reilly, J. J., & Saunders, D. H. (2018). Physical activity, diet and other behavioural interventions for improving cognition and school achievement in children and adolescents with obesity or overweight. Cochrane Database of Systematic Reviews, (1).
Martin, A., Booth, J. N., McGeown, S., Niven, A., Sproule, J., Saunders, D. H., & Reilly, J. J. (2017). Longitudinal associations between childhood obesity and academic achievement: Systematic review with focus group data. Current Obesity Reports, 6(3), 297–313.
Metcalf, B. S., Hosking, J., Jeffery, A. N., Voss, L. D., Henley, W., & Wilkin, T. J. (2011). Fatness leads to inactivity, but inactivity does not lead to fatness: A longitudinal study in children (EarlyBird 45). Archives of Disease in Childhood, 96(10), 942–947.
Miller, A. A., & Spencer, S. J. (2014). Obesity and neuroinflammation: A pathway to cognitive impairment. Brain, Behavior, and Immunity, 42, 10–21.
Mora‐Gonzalez, J., Esteban-Cornejo, I., Cadenas-Sanchez, C., Migueles, J. H., Molina-Garcia, P., Rodriguez-Ayllon, M., ... & Ortega, F. B. (2019a). Physical fitness, physical activity, and the executive function in children with overweight and obesity. Journal of Pediatrics, 208, 50-56.
Mora‐Gonzalez, J., Esteban‐Cornejo, I., Cadenas‐Sanchez, C., Migueles, J. H., Rodriguez‐Ayllon, M., Molina‐García, P., ... & Ortega, F. B. (2019b). Fitness, physical activity, working memory, and neuroelectric activity in children with overweight/obesity. Scandinavian Journal of Medicine & Science in Sports, 29(9), 1352-1363.
Mora‐Gonzalez, J., Esteban‐Cornejo, I., Solis‐Urra, P., Migueles, J. H., Cadenas‐Sanchez, C., Molina‐Garcia, P., ... & Ortega, F. B. (2020). Fitness, physical activity, sedentary time, inhibitory control, and neuroelectric activity in children with overweight or obesity: The ActiveBrains project. Psychophysiology, 57(6), e13579.
Mora‐Gonzalez, J., Migueles, J. H., Esteban-Cornejo, I., Cadenas-Sanchez, C., Pastor-Villaescusa, B., Molina-García, P., ... & Escolano-Margarit, M. V. (2019). Sedentarism, physical activity, steps, and neurotrophic factors in obese children. Medicine & Science in Sports & Exercise, 51, 2325-2333.
Moreno, L. A., Pigeot, I., & Ahrens, W. (2011). Childhood obesity: Etiology-synthesis part II. In L. A. Moreno, I. Pigeot, & W. Ahrens (Eds.), Epidemiology of obesity in children and adolescents (pp. 483–492). Springer.
Østby, Y., Tamnes, C. K., Fjell, A. M., & Walhovd, K. B. (2011). Morphometry and connectivity of the fronto-parietal verbal working memory network in development. Neuropsychologica, 49, 3854–3862.
Ou, X., Andres, A., Pivik, R. T., Cleves, M. A., & Badger, T. M. (2015). Brain gray and white matter differences in healthy normal weight and obese children. Journal of Magnetic Resonance Imaging, 42(5), 1205–1213.
Polich, J. (2007). Updating P300: An integrative theory of P3a and P3b. Clinical Neurophysiology, 118(10), 2128–2148.
Polk, T. A., Simen, P., Lewis, R. L., & Freedman, E. (2002). A computational approach to control in complex cognition. Cognitive Brain Research, 15, 71–83.
Raine, L., Drollette, E., Kao, S. C., Westfall, D., Chaddock-Heyman, L., Kramer, A. F., ... & Hillman, C. (2018). The associations between adiposity, cognitive function, and achievement in children. Medicine & Science in Sports & Exercise, 50(9), 1868-1874.
Raine, L. B., Khan, N. A., Drollette, E. S., Pontifex, M. B., Kramer, A. F., & Hillman, C. H. (2017). Obesity, visceral adipose tissue, and cognitive function in childhood. Journal of Pediatrics, 187, 134–140.
Rodriguez-Ayllon, M., Esteban-Cornejo, I., Verdejo-Román, J., Muetzel, R. L., Mora-Gonzalez, J., Cadenas-Sanchez, C., ... & Ortega, F. B. (2020). Physical fitness and white matter microstructure in children with overweight or obesity: the ActiveBrains project. Scientific Reports, 10(1), 1-9.
Ronan, L., Alexander-Bloch, A., & Fletcher, P. C. (2020). Childhood obesity, cortical structure, and executive function in healthy children. Cerebral Cortex, 30(4), 2519–2528.
Ross, N., Yau, P. L., & Convit, A. (2015). Obesity, fitness, and brain integrity in adolescence. Appetite, 93, 44–50.
Rubia, K. (2013). Functional brain imaging across development. European Child and Adolescent Psychiatry, 22, 719–731.
Santana, C. C. A., Hill, J. O., Azevedo, L. B., Gunnarsdottir, T., & Prado, W. L. (2017). The association between obesity and academic performance in youth: A systematic review. Obesity Reviews, 18(10), 1191–1199.
Schaeffer, D. J., Krafft, C. E., Schwarz, N. F., Chi, L., Rodrigue, A. L., Jordan, R., …, McDowell, J. E. (2014). An 8-month exercise intervention alters frontotemporal white matter integrity in overweight children. Psychophysiology, 51, 728-733.
Schmahmann, J., Pandya, D., Wang, R., Dai, G., D’Arceuil, H., de Crespigny, A., & Wedeen, V. (2007). Association fibre pathways of the brain: parallel observations from diffusion spectrum imaging and autoradiography. Brain, 130, 630–653.
Scudder, M. R., Khan, N. A., Lambourne, K., Drollette, E. S., Herrmann, S. D., Betts, J. L., … Hillman, C. H. (2015). Cognitive control in preadolescent children with risk factors for metabolic syndrome. Health Psychology, 34, 243-252.
Sullivan Giovanello, K., Schnyer, D. M., & Verfaellie, M. (2004). A critical role for the anterior hippocampus in relational memory: Evidence from an fMRI study comparing associative and item recognition. Hippocampus, 14(1), 5–8.
Sun, X., Li, Y., Cai, L., et al. (2021). Effects of physical activity interventions on cognitive performance of overweight or obese children and adolescents: A systematic review and meta-analysis. Pediatric Research, 89(1), 46–53.
Takeda, S., Sato, N., & Morishita, R. (2014). Systemic inflammation, blood-brain barrier vulnerability and cognitive/non-cognitive symptoms in Alzheimer disease: Relevance to pathogenesis and therapy. Frontiers in Aging Neuroscience, 6, 171.
Tarumi, T., Gonzales, M., Fallow, B., Nualnim, N., Lee, J., Tanaka, H., & Haley, A. P. (2013). Aerobic fitness and cognitive function in midlife: An association mediated by plasma insulin. Metabolic Brain Disease, 28, 727–730.
Torres-Costoso, A., Pozuelo-Carrascosa, D. P., Alvarez-Bueno, C., Ferri-Morales, A., Miota Ibarra, J., Notario-Pacheco, B., & Martinez-Vizcaino, V. (2017). Insulin and bone health in young adults: The mediator role of lean mass. PloS One, 12(3), e0173874.
Trachta, P., Drapalova, J., Kavalkova, P., Touskova, V., Cinkajzlova, A., Lacinova, Z., …, Haluzik, M. (2014). Three months of regular aerobic exercise in patients with obesity improve systemic subclinical inflammation without major influence on blood pressure and endocrine production of subcutaneous fat. Physiological Research, 63, S299-S308.
Tsai, C. L., Chen, F. C., Pan, C. Y., & Tseng, Y. T. (2016). The neurocognitive performance of visuospatial attention in children with obesity. Frontiers in Psychology, 7, 1033.
van Praag, H., Shubert, T., Zhao, C., & Gage, F. H. (2005). Exercise enhances learning and hippocampal neurogenesis in aged mice. Journal of Neuroscience, 25(38), 8680–8685.
Vestergaard, M., Madsen, K. S., Baaré, W. F., Skimminge, A., Ejersbo, L. R., Ramsøy, T. Z., …, Jernigan, T. L. (2010). White matter microstructure in superior longitudinal fasciculus associated with spatial working memory performance in children. Journal of Cognitive Neuroscience, 23, 2135-2146.
Wajchenberg, B. L. (2000). Subcutaneous and visceral adipose tissue: Their relation to the metabolic syndrome. Endocrine Reviews, 21(6), 697–738.
Walk, A. M., Raine, L. B., Kramer, A. F., Cohen, N. J., Hillman, C. H., & Khan, N. A. (2020). Adiposity is related to neuroelectric indices of motor response preparation in preadolescent children. International Journal of Psychophysiology, 147, 176–183.
WHO. Obesity and Overweight. 2020; https://www.who.int/en/news-room/fact-sheets/detail/obesity-and-overweight#.
Wickman, C., & Kramer, H. (2013). Obesity and kidney disease: Potential mechanisms. In Seminars in nephrology (Vol. 33, No. 1, pp. 14–22). WB Saunders.
Willette, A. A., & Kapogiannis, D. (2015). Does the brain shrink as the waist expands? Ageing Research Reviews, 20, 86–97.
Wöstmann, N. M., Aichert, D. S., Costa, A., Rubia, K., Möller, H., & Ettinger, U. (2013). Reliability and plasticity of response inhibition and interference control. Brain and Cognition, 81, 82–94.
Yates, K. F., Sweat, V., Yau, P. L., Turchianoa, M. M., & Convit, A. (2012). Impact of metabolic syndrome on cognition and brain: A selected review of the literature. Arteriosclerosis, Thrombosis, and Vascular Biology, 32, 2060–2067.
Yau, P. L., Javier, D. C., Ryan, C. M., Tsui, W. H., Ardekani, B. A., Ten, S., & Convit, A. (2010). Preliminary evidence for brain complications in obese adolescents with type 2 diabetes mellitus. Diabetologia, 53(11), 2298–2306.
Zavala-Crichton, J. P., Esteban-Cornejo, I., Solis-Urra, P., Mora-Gonzalez, J., Cadenas-Sanchez, C., Rodriguez-Ayllon, M., ... & Hillman, C. H. (2020). Association of sedentary behavior with brain structure and intelligence in children with overweight or obesity: The ActiveBrains Project. Journal of Clinical Medicine, 9(4): 1101.
Westfall, D. R., Anteraper, S. A., Chaddock-Heyman, L., Drollette, E. S., Raine, L. B., Whitfield-Gabrieli, S., ... & Hillman, C. H. (2020). Resting-state functional connectivity and scholastic performance in preadolescent children: a data-driven multivoxel pattern analysis (MVPA). Journal of Clinical Medicine, 9(10), 3198
Funding
Shu-Shih Hsieh was supported by the Postdoctoral Research Abroad Program from the Ministry of Science and Technology in Taiwan (reference number: 109–2917-I-564–034). Francisco B. Ortega’s research activity was supported by funds from Spanish Ministry of Economy and Competitiveness (Reference number: DEP2016–79512-R and DEP2017-91544-EXP) and the Andalusian Operational Programme supported with European Regional Development Funds (ERDF in English, FEDER in Spanish, project ref: B-CTS-355-UGR18).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
All authors have agreed to the submission of the manuscript in its current form.
Conflict of Interest
The authors declare no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hsieh, SS., Raine, L.B., Ortega, F.B. et al. The Role of Chronic Physical Activity in Alleviating the Detrimental Relationship of Childhood Obesity on Brain and Cognition. J Cogn Enhanc 6, 248–271 (2022). https://doi.org/10.1007/s41465-021-00230-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41465-021-00230-7