Abstract
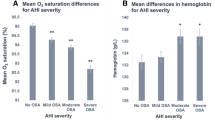
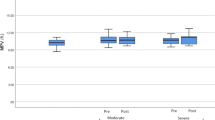
It is recently found that the red blood cell distribution width (RDW) is independently associated with cardiovascular disease in patients with obstructive sleep apnea (OSA).The goal of this study is to investigate the correlation of RDW with the severity of OSA and whether RDW could be used to monitor the response to continuous positive airway pressure (CPAP) therapy in OSA patients. The study enrolled 70 participants. Control group (n = 24) consisted of patients with normal polysomnography and OSA group (n = 46) comprised patients with OSA of varying severity. RDW was measured before polysomnography in both groups. In addition, RDW was measured in the OSA group following 3 months of CPAP therapy. The RDW was significantly higher in the OSA group (p < 0.001), and this difference remained after adjusting for age and body mass index (p = 0.001). The RDW was approximately twofold greater in the OSA group (OR 2.126, 95% confidence interval 1.32–3.41; p = 0.002). On univariate analysis, the RDW was significantly correlated with hypoxia parameters, which was persistent with multivariate analysis. Furthermore, CPAP therapy reduced RDW (p = 0.002), and the change in the severity of 3% ODI by CPAP was correlated with the change in the RDW (r = 0.416, p = 0.013). The high RDW may be related to the pathophysiology of OSA. The high RDW in OSA may be associated with hypoxia. Therefore, treating OSA with CPAP could improve the RDW.


Similar content being viewed by others
References
Gopalakrishnan P, Tak T. Obstructive sleep apnea and cardiovascular disease. Cardiol Rev. 2011. https://doi.org/10.1097/CRD.0b013e318223bd08.
Fava C, Montagnana M, Favaloro EJ, Guidi GC, Lippi G. Obstructive sleep apnea syndrome and cardiovascular diseases. Semin Thromb Hemost. 2011. https://doi.org/10.1055/s-0031-1273092.
Lavie L, Polotsky V. Cardiovascular aspects in obstructive sleep apnea syndrome molecular issues, hypoxia and cytokine profiles. Respiration. 2009;78(4):361–70. https://doi.org/10.1159/000243552.
Ryan S, Taylor CT, McNicholas WT. Systemic inflammation: a key factor in the pathogenesis of cardiovascular complications in obstructive sleep apnea syndrome? Thorax. 2009. https://doi.org/10.1136/thx.2008.105577.
Ciccone MM, Scicchitano P, Zito A, Cortese F, Boninfante B, Falcone VA, Quaranta VN, Ventura VA, Zucano A, Di Serio F, Damiani MF, Resta O. Correlation between inflammatory markers of atherosclerosis and carotid intima–media thickness in obstructive sleep apnea. Molecules. 2014. https://doi.org/10.3390/molecules19021651.
Berg S. Obstructive sleep apnea syndrome: current status. Clin Respir J. 2008. https://doi.org/10.1111/j.1752-699X.2008.00076.x.
Perkins SL. Examination of blood and bone marrow. In: Greer JP, Foerster J, Lukens JN, Rodgers GM, Paraksevas F, Glader BE, editors. Wintrobe’s clinical hematology. 11th ed. Utah: Lippincott Wilkins & Williams; 2003. pp. 5–25.
Felker GM, Allen LA, Pocock SJ, Shaw LK, McMurray JJ, Pfeffer MA, Swedberg K, Wang D, Yusuf S, Michelson EL, Granger CB, CHARM investigators. Red blood cell distribution width as a novel prognostic factor in heart failure: data from the CHARM program and the Duke databank. J Am Coll Cardiol. 2007. https://doi.org/10.1016/j.jacc.2007.02.067.
Dabbah S, Hammerman H, Markiewicz W, Aronson D. Relation between red cell distribution width and clinical outcomes after acute myocardial infarction. Am J Cardiol. 2010. https://doi.org/10.1016/j.amjcard.2009.09.027.
Drakopoulou M, Toutouzas K, Stefanadi E, Tsiamis E, Tousoulis D, Stefanadis C. Association of inflammatory markers with angiographic severity and extent of coronary artery disease. Atherosclerosis. 2009. https://doi.org/10.1016/j.atherosclerosis.2009.01.041.
Tonelli M, Sacks F. Arnold M, Moye L, Davis B, Pfeffer M, Cholesterol and Recurrent Events (CARE) Trial Investigators. Relation between red blood cell distribution width and cardiovascular event rate in people with coronary disease. Circulation. 2008. https://doi.org/10.1161/circulationaha.107.727545.
Weiss G, Goodnough LT. Anemia of chronic disease. N Eng J Med. 2005. https://doi.org/10.1056/NEJMra041809.
Mozos I. Mechanisms linking red cell blood disorders and cardiovascular diseases. BioMed Res Int. 2015. https://doi.org/10.1155/2015/682054.
Ozsu S, Abul Y, Gulsoy A, Bulbul Y, Yaman S, Ozlu T. Red cell distribution width in patients with obstructive sleep apnea syndrome. Lung. 2012. https://doi.org/10.1007/s00408-012-9376-x.
Johns MW. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991. https://doi.org/10.1093/sleep/14.6.540.
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra M, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM. American Academy of Sleep Medicine. Rules for scoring respiratory events in sleep: update of the 2007 AASM manual for the scoring of sleep and associated events. Deliberations of the sleep apnea definitions task force of the American academy of sleep medicine. J Clin Sleep Med. 2012. https://doi.org/10.5664/jcsm.2172.
Flemons WW, Buysse D, Redline S, Pack A, Strohl K, Wheatley T, Young T, Douglas N, Levy P, McNicholas W, Fleetham J, White D, Schmidt-Nowarra W, Carley D, Romaniuk J. Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22:667–89.
Feliciano A, Linhans R, Marçôa R, Cysneiros A, Martinho C, Reis RP, Penque D, Pinto P, Bárbara C. Hematologic evaluation in males with obstructive sleep apnea before and after positive airway pressure. Rev Port Pneumol. 2017. https://doi.org/10.1016/j.rppnen.2016.12.001.
Sokucu N, Özdemir C, Dalar L, Karasulu L, Aydin Ş, Altin S. Complete blood count alterations after six months of continuous positive airway pressure treatment in patients with severe obstructive sleep apnea. J Clin Sleep Med. 2014. https://doi.org/10.5664/jcsm.3958.
Gunbatar H, Sertogullarından B, Ekin S, Akdag S, Arisoy A, Sayhan H. The correlation between red blood cell distribution width levels with the severity of obstructive sleep apnea and carotid intima media thickness. Med Sci Monit. 2014. https://doi.org/10.12659/MSM.891001.
Sokucu NS, Karasulu L, Dalar L, Seyhan EC, Altin S. Can red blood cell distribution width predict severity of obstructive sleep apnea syndrome? J Clin Sleep Med. 2012. https://doi.org/10.5664/jcsm.2146.
Gordon P, Sanders MH. Sleep 7: positive airway pressure therapy for obstructive sleep apnea/hypopnea syndrome. Thorax. 2005. https://doi.org/10.1136/thx.2003.007195.
Xie X, Pan L, Ren D, Du C, Guo Y. Effects of continuous positive airway pressure therapy on systemic inflammation in obstructive sleep apnea: a meta-analysis. Sleep Med. 2013. https://doi.org/10.1016/j.sleep.2013.07.006.
Hegglin A, Schoch OD, Korte W, Hahn K, Hurny C, Münzer T. Eight months of continuous positive airway pressure (CPAP) decrease tumor necrosis factor alpha (TNFA) in men with obstructive sleep apnea syndrome. Sleep Breath. 2012. https://doi.org/10.1007/s11325-011-0512-2.
Tsiara S, Elisaf M, Jagroop IA, Mikhailidis DP. Platelets as predictors of vascular risk: is there a practical index of platelet activity? Clin Appl Thromb Hemost. 2003; 9:177–190.
Yilmaz Avci A, Avci S, Lakadamyali H, Can U. Hypoxia and inflammation indicate significant differences in the severity of obstructive sleep apnea within similar apnea–hypopnea index groups. Sleep Breath. 2017. https://doi.org/10.1007/s11325-017-1486-5.
Varol E, Ozturk O, Gonca T, Has M, Ozaydın M, Erdogan D, Akkaya A. Mean platelet volume is increased in patients with severe obstructive sleep apnea. Scand J Clin Lab Investig. 2010. https://doi.org/10.3109/00365513.2010.520733.
Kurt OK, Yildiz N. The importance of laboratory parameters in patients with obstructive sleep apnea syndrome. Blood Coagul Fibrinolysis. 2013. https://doi.org/10.1097/mbc.0b013e32835d53d4.
Kivanç T, Kulaksizoglu S, Lakadamyali H, Eyupoglu F. Importance of laboratory parameters in patients with obstructive sleep apnea and their relationship with cardiovascular disease. J Clin Lab. 2018. https://doi.org/10.1002/jcla.22199.
Funding
No funding was received for this research.
Author information
Authors and Affiliations
Contributions
HL and TK conceived and designed the study, acquired the data, and wrote the manuscript. AYA critically revised the manuscript and contributed important intellectual content.
Corresponding author
Ethics declarations
Conflict of interest
Lakadamyali H. declares that he has no conflict of interest. Kivanc T. declares that he has no conflict of interest. Yilmaz Avci A. declares that she has no conflict of interest.
Ethical approval
This study was approved by Ministry of Health Research and Training Center Clinical Research Ethical Committee approval number 2015-110 and conducted in accordance with Declaration of Helsinki 1964.
Informed consent
Informed consent was obtained from all participants included in the study.
Rights and permissions
About this article
Cite this article
Lakadamyali, H., Kivanc, T. & Yilmaz Avci, A. Correlation of changes in the red blood cell distribution width with the response to continuous positive airway pressure in patients with obstructive sleep apnea. Sleep Biol. Rhythms 17, 141–148 (2019). https://doi.org/10.1007/s41105-018-0191-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s41105-018-0191-5