Abstract
Although treatment with biologic disease-modifying antirheumatic drugs (bDMARDs) has significantly improved clinical outcomes in patients with rheumatoid arthritis (RA), many patients do not have access to these treatments. As cost-effective alternatives to their reference products (RPs), biosimilars provide an opportunity to increase access to bDMARDs. The European Medicines Agency and the US Food and Drug Administration have detailed pathways for the approval of biosimilars based on establishing the similarity of the biosimilar to the RP in terms of structure and function, pharmacokinetics (PK), efficacy, safety, and immunogenicity. A number of biosimilars of adalimumab, infliximab, etanercept, and rituximab RPs have been approved in the United States and/or European Union. This article is focused on the seven adalimumab biosimilars. A review of the data for the biosimilars FKB327, ABP 501, BI 695501, GP2017, MSB11022, PF-06410293, and SB5 confirm that these products are highly similar to the adalimumab RP with regard to structure, physicochemical and biological properties, PK, safety, immunogenicity, and efficacy in the treatment of RA and other chronic immune-mediated, inflammatory conditions. Data from several switching studies showed no changes in efficacy, safety, trough serum drug concentration, or immunogenicity between the biosimilars and their RP.
Trial registration: ClinicalTrials.gov identifiers: NCT02260791, NCT02405780, NCT01970475, NCT02137226, NCT02045979, NCT02744755, NCT02144714, NCT02167139, NCT03014947, NCT02114931, NCT02640612, NCT02167139, NCT03052322, NCT02480153. EudraCT numbers: 2012-005140-23, 2012-000785-37, 2013-003722-84, 2015-000579-28, 2014-002879-29, 2014-000662-21, 2013-004654-13, 2015-002634-41, 2014-005229-11, 2016-002852-26, 2014-000352-29
Plain Language Summary
Biologic disease-modifying antirheumatic drugs (bDMARDs) improve outcomes for patients with rheumatoid arthritis (RA); however, many patients do not have access to these treatments. Biosimilars offer a cost-effective alternative to their reference product (RP) and provide the opportunity to increase access to bDMARDs. This article reviews available data regarding the pharmacokinetics (PK), safety, immunogenicity, and effectiveness of the adalimumab RP and its biosimilars (FKB327, ABP 501, BI 695501, GP2017, MSB11022, PF-06410293, and SB5) in the treatment of RA. Based on the published literature, we concluded that these products are similar to the adalimumab RP in terms of their structure, physicochemical and biological properties, and PK. We also found that these biosimilars have similar safety and effectiveness to the adalimumab RP in the treatment of patients with RA. In addition, switching between a biosimilar and the adalimumab RP resulted in no impact on safety, effectiveness, serum concentrations, or immunogenicity.
Similar content being viewed by others
Biosimilars offer a cost-effective alternative to their reference product (RP) and provide an opportunity to increase access to bDMARDs for patients with rheumatoid arthritis (RA). |
The objective of this review was to summarize the available data regarding the pharmacokinetics (PK), safety, immunogenicity, and efficacy of adalimumab RP biosimilars (FKB327, ABP 501, BI 695501, GP2017, MSB 11022, PF-06410293, and SB5) in the treatment of RA. |
Based on the findings from this review, we conclude that FKB327, ABP 501, BI 695501, GP2017, MSB11022, PF-06410293, and SB5 are similar to adalimumab RP with respect to their structure and physicochemical and biological properties. |
These products have also demonstrated similar safety and efficacy to adalimumab RP in the treatment of patients with RA. |
Single switching studies conducted with BI 695501, ABP 501, and SB5, and a double switching study conducted with FKB327 found that switching between these biosimilars and adalimumab RP did not significantly impact safety, efficacy, trough serum concentrations, or immunogenicity. |
Digital Features
This article is published with digital features, including a summary slide and plain language summary, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.13221110.
Introduction
Since its introduction in the late 1990s, the use of biologic-based therapy in the treatment of rheumatoid arthritis (RA) has improved outcomes for patients [1]. Biologic disease-modifying antirheumatic drugs (bDMARDs) have been shown to improve symptoms, reduce joint inflammation, limit erosive damage, decrease disability, and improve quality of life [1, 2]. Despite improved outcomes associated with biologics, many patients do not have access to these treatments [2]. The high costs of novel therapies have curbed widespread use, resulting in inequity with regard to access to biologics [3].
Biosimilars are cost-effective alternatives to their reference product (RP), and offer an opportunity to increase access to biologics [2]. A biosimilar is defined as a biotherapeutic product that is similar to an already-licensed biotherapeutic RP in terms of quality, safety, and efficacy [4]. Biosimilars have been shown to introduce price competition and subsequently reduce the cost of treatment [5]. Reductions in expenditures on biologics and cost-savings to improve access to important medicines are essential to allowing all patients to receive optimal treatment for their disease [2].
The European Medicines Agency (EMA) and the US Food and Drug Administration (FDA) have both provided guidance regarding the regulatory requirements for biosimilar approval. The FDA employs a totality-of-evidence approach to review applications for biosimilar products and recommends a stepwise methodology for demonstrating biosimilarity based on comparisons of the proposed biosimilar and the RP in terms of structure, function, animal toxicity, human pharmacokinetics (PK) and pharmacodynamics (PD), clinical immunogenicity, and clinical safety and effectiveness [6]. Similar to the FDA, the EMA requires similarity of the proposed product to the authorized product to be established in terms of quality characteristics, biological activity, safety, and efficacy based on a comprehensive comparability exercise, which includes physicochemical and biological characterization [7]. In addition, the active substance of a biosimilar must be similar to the RP in both molecular and biological terms. The goal of the comparability exercise is to exclude any relevant differences between the biosimilar and the RP, which requires that studies be adequately sensitive regarding design, conduct, endpoints, and/or population to detect such differences. Furthermore, the comparable safety and efficacy of a biosimilar to the RP must be demonstrated or otherwise justified. A confirmatory clinical trial may not be necessary if similar efficacy and safety can clearly be deduced from the similarity of physicochemical characteristics, biological activity/potency, and PK and/or PD profiles of the biosimilar and the RP.
If biosimilarity has been established for a given indication, extrapolation to other indications of the RP can be approved with appropriate scientific justification. Scientific justification for extrapolation should include: (1) the mechanism(s) of action in each condition of use for which licensure is sought; (2) the PK, biodistribution, and immunogenicity of the product in different patient populations; (3) differences in expected toxicities in each patient population; and (4) any other fact that may affect the safety or efficacy of the product in each patient population. It is also important to note that even if evidence is sufficient to support the extrapolation of indications, biosimilars may have fewer indications than the RP [8]. For example, an RP may have unexpired exclusivity for an indication that prevents other manufacturers from receiving approval for that indication.
Moreover, it is important to realize that with the introduction of biosimilars, multiple manufacturers with different quality systems will produce similar biologics [9]. Over time, it is possible that clinically meaningful differences among these products could emerge as a result of different patterns of product drift and evolution, a process that has been defined as divergence [9]. By establishing robust pharmacovigilance systems, manufacturers and policymakers can minimize the potential impact of divergence.
Consistent with this concept, the FDA and EMA have established positions regarding the importance of pharmacovigilance. As with all biological products, the FDA considers robust postmarketing safety monitoring an important component in ensuring the safety and effectiveness of biosimilars [6].
Currently, biosimilars are approved for four originator biologic agents that are used to treat RA, including adalimumab (Humira®; AbbVie Inc.), etanercept (Enbrel®; Amgen), infliximab (Remicade®; Janssen), and rituximab (US: Rituxan®; Genentech/Biogen, EU: MabThera®; Roche). Adalimumab, etanercept, and infliximab are tumor necrosis factor (TNF) inhibitors, and rituximab is a CD20-directed cytolytic antibody. The EU and US indications for these biologic agents are shown in Table 1. Twelve biosimilars are currently approved for these RPs. Table 2 shows the approved biosimilars, their indications, and their approval dates.
The focus of this review is on the available biosimilars for adalimumab and on the evidence that demonstrates their biosimilarity to the RP. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors. The aim of this article is to summarize the available data regarding the PK, safety, immunogenicity, and efficacy of FKB327, ABP 501, BI 695501, GP2017, MSB11022, PF-06410293, and SB5 in the treatment of RA, as well as evidence of their biosimilarity to the adalimumab RP.
Methods
Searches of the PubMed and Cochrane databases were conducted on July 24, 2020, with no date restrictions, to identify publications reporting data on adalimumab biosimilars. The primary outcomes studied included PK, safety, immunogenicity, and efficacy. In brief, the search strategy included the terms “FKB327,” “ABP 501,” “BI 695501,” “GP2017,” “MSB11022,” “PF-06410293,” and “SB5.” Clinical studies of any phase were included. Studies were excluded if they were not published in English, if they were review articles or conference abstracts, or if they did not discuss data related to the PK or safety and efficacy of adalimumab biosimilars for the treatment of RA. Studies comparing bioavailability between injection devices were also excluded.
Preliminary screening of all publications identified in this literature search was conducted by a single reviewer to assess titles and abstracts based on the eligibility criteria. Consensus to include screened studies was reached by a second reviewer. Any discrepancies between the findings of the two reviewers were resolved by a third reviewer. Following inclusion confirmation, a reviewer extracted relevant data from the studies and a second reviewer provided validation of all extracted data.
Results
FKB327
Based on the results from characterization studies employing physicochemical and biological methods, FKB327 was found to have the expected structure of a human immunoglobulin (Ig)G1-type antibody and was determined to be highly similar to the adalimumab RP in physicochemical and biological properties [9].
The PK, safety, tolerability, and immunogenicity of FKB327 were compared with those of EU-approved Humira (EU-Humira) and US-approved Humira (US-Humira) in a randomized, double-blind, parallel group study among 180 healthy subjects who received a single subcutaneous (SC) injection of 40 mg EU-Humira, US-Humira, or FKB327 [10]. PK similarity was concluded among all three treatments, as the 90% confidence interval (CI) for the ratio of the geometric means for the primary PK parameters of area under the serum concentration–time curve to the last detectable value (AUC0–t), area under the serum concentration–time curve extrapolated to infinity (AUC0–∞), and peak serum concentration (Cmax) from the analysis of covariance were all within the predefined limits of 0.80–1.25. FKB327 was well tolerated by healthy subjects in this study, and adverse events (AEs) were similar across all treatments. A total of 110 subjects (61.1%) experienced ≥ 1 AEs (FKB327, 35 [58%]; EU-Humira, 39 [65%]; US-Humira, 36 [60%]). Most of the AEs were mild or moderate in severity. Two patients, one each in the FKB327 and US-Humira treatment groups, experienced a serious AE (SAE). No important differences were found among treatments regarding the nature of the AEs. Regarding immunogenicity, the proportion of subjects with positive antidrug antibody (ADA) activity at the last sampling point was similar among treatments: 69.5% for FKB327, 73.3% for EU-Humira, and 70.0% for US-Humira. The development of ADAs specific to FKB327, EU-Humira, and US-Humira was also similar among treatments, along with the proportion of subjects at each level of ADA titer, and cross reactivity was high among the three DA assays.
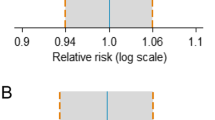
The efficacy and safety of FKB327 in the treatment of RA was compared with the adalimumab RP in a 24-week, double-blind phase 3 study among 730 patients whose disease was inadequately controlled with methotrexate (MTX) [11]. The primary and key secondary endpoints were American College of Rheumatology (ACR)20 (a composite measure defined as 20% improvement in both the number of tender and swollen joints and in three of the following five criteria: patient global assessment, physician global assessment, functional ability measure, visual analog pain scale, and C-reactive protein [CRP]) and Disease Activity Score (DAS)28-CRP response rates at week 24, respectively. Other secondary endpoints included safety, ADAs, and PK. The ACR20 response rates were comparable: 74.1% in the FKB327 group and 75.7% in the adalimumab RP group, a difference of 1.6 (95% CI – 7.9 to 4.7), which was within the ± 13% equivalence margins set by the EMA. The least square means (LSMs) for DAS28-CRP were also comparable: 3.43 in the FKB327 group and 3.42 in the adalimumab RP group, a difference of 0.01 (95% CI – 0.16 to 0.18), which was within the ± 0.6 equivalence margins set by the EMA [11]. The immunogenicity observed in this study was consistent with previous findings. The proportion of patients positive for neutralizing antibodies (NAbs) at week 24 was similar: 57.7% and 55.5% in the FKB327 and adalimumab RP groups, respectively [11]. Nearly all ADAs developed during this study were shown to be neutralizing, as assessed by sensitive competitive ligand binding. Regarding PK parameters, the mean serum trough concentration–time profiles for adalimumab were broadly comparable, as were the serum trough concentrations at week 24: 1.10 [0.95–1.27]) [11].
Patients who completed the double-blind study with clinical response and no SAEs (period 1) were rerandomized to FKB327 or the adalimumab RP in an open-label extension (OLE) so that two-thirds of patients continued receiving the same treatment as in the double-blind study and one-third switched to the alternate treatment for 30 weeks (period 2) [12]. After 30 weeks, all patients received FKB327 until week 76 and were followed for an additional 4 weeks until week 80 (period 3) Fig. 1. The primary endpoint in this study was safety; secondary endpoints were efficacy, ADAs, and PK. A total of 645 patients were enrolled in period 2 (FKB327–FKB327, n = 216; adalimumab RP–adalimumab RP, n = 213; FKB327–adalimumab RP, n = 108; adalimumab RP–FKB327, n = 108). Results suggest the long-term safety, efficacy, PK, and immunogenicity of FKB327 and the adalimumab RP are comparable with continuous and switched treatment. Over the 30 weeks (period 2), ACR20 response rates were sustained and comparable for all treatment groups. ACR20 response rates for continuous-use patients ranged from 71.3 to 75.5% and 77.5 to 82.6% for the FKB327–FKB327 and adalimumab RP–adalimumab RP groups, respectively [12]. ACR20 response rates for switched patients ranged from 67.6 to 82.4% and 73.1 to 75.9% for the FKB327–adalimumab RP and the adalimumab RP–FKB327 groups, respectively [12]. No consistent differences in PK and ADA profiles were observed between continuous and switched treatments.

Adapted by permission from BMJ Publishing Group Limited. Long-term safety, immunogenicity and efficacy comparing FKB327 with adalimumab reference product in patients with active rheumatoid arthritis: data from randomised double-blind and open-label extension studies, Genovese MC, et al., vol 6, e000987, 2020
Schema of period 1, period 2, and period 3 Studies. DB double-blind, EOW every other week, F FKB327, OLE open-label extension, R randomized, RA rheumatoid arthritis, RP reference product, SC subcutaneous, w week.
In the integrated safety analysis (periods 1 and 2), no correlation was found between ADA response and hypersensitivity reactions [11]. The incidence of AEs from the integrated analysis is shown in Table 3. No differences were found in the safety profiles between FKB327 and the adalimumab RP [11].
Through the end of the study (period 3), 59.4% of patients experienced ≥ 1 treatment-emergent AEs (TEAEs) [12]. The percentage of patients experiencing ≥ 1 TEAEs was similar for all four groups, with a slightly lower percentage reported for the adalimumab RP–FKB327–FKB327 group (FKB327–adalimumab RP–FKB327, 61.0%; FKB327–FKB327–FKB327, 60.3%; adalimumab RP–adalimumab RP–FKB327, 60.0%; adalimumab RP–FKB327–FKB327, 54.8%). The ACR20 response rate ranges were also similar for all four groups (FKB327–adalimumab RP–FKB327, 74.5–78.6%; FKB327–FKB327–FKB327, 75.7–84.3%; adalimumab RP–adalimumab RP–FKB327, 83.6–86.8%; adalimumab RP–FKB327–FKB327, 83.7–88.0%) [12]. At week 80, the percentage of patients testing positive for ADAs ranged from 42.4% in the adalimumab RP-adalimumab RP-FKB327 sequence to 55.2% in the FKB327-adalimumab RP-FKB327 sequence. In addition, NAbs did not increase in any sequence during the study, ranging from 41.8 to 55.2% [12].
ABP 501
A comprehensive similarity assessment was conducted to compare ABP 501 with EU-Humira and US-Humira [13, 14]. Results from this assessment demonstrated functional similarity among these products with regard to biological properties, including binding to soluble and transmembrane TNF-α; neutralization of TNF-α–induced caspase activation, TNF-α— and lymphotoxin-α—induced chemokine production, and cytotoxicity; Fc-receptor binding; and effector function activation [13]. ABP 501 was found to be similar to the adalimumab RP in terms of physicochemical and biological properties [14].
The PK, safety, tolerability, and immunogenicity of ABP 501 was assessed in a randomized, single-blind study in 203 healthy subjects who received a single, SC injection of ABP 501, EU-Humira, or US-Humira [15]. The geometric means for all PK parameters (AUC0-∞ and Cmax), as well as the peak and overall exposures, were similar across all treatment groups. The PK equivalence among ABP 501 and EU-Humira and US-Humira was confirmed, as the 90% CIs for geometric mean ratios of AUC0-∞ and Cmax were fully contained within the standard equivalence criteria of 0.80–1.25 for all group comparisons. No deaths, SAEs, or AEs leading to study discontinuation were reported in the study. The percentage of subjects reporting any AEs in the ABP 501, EU-Humira, and US-Humira groups were 58.2, 68.7, and 47.8%, respectively. The most frequent AEs reported during the study were headache (ABP 501, 19; EU-Humira, 13; US-Humira, 16), oropharyngeal pain (ABP 501, 19; EU-Humira, 13; US-Humira, 16), sinus congestion (ABP 501, 6; EU-Humira, 0; US-Humira, 6), nasopharyngitis (ABP 501, 4; EU-Humira, 7; US-Humira, 0), and nausea (ABP 501, 5; EU-Humira, 4; US-Humira, 2). The incidence of ADAs at the end of the study was similar for all three treatment groups (ABP 501, 43.3%; EU-Humira, 50.7%; US-Humira, 50.0%). The incidence of NAbs, as measured by a cell-based assay using a TNF-α—responding cell line, was also similar among treatment groups and was detected in 17.9, 19.4, and 21.7% of the subjects of the ABP 501, EU-Humira, and US-Humira groups, respectively.
The efficacy and safety of ABP 501 was compared with the adalimumab RP in patients with moderate-to-severe RA despite treatment with MTX in a 26-week, randomized, double-blind phase 3 equivalence study [16]. The primary endpoint was the risk ratio (RR) between ABP 501 and the adalimumab RP at week 24, with the primary hypothesis being that the treatments were equivalent if the 90% CI RR was between 0.738 and 1.355. Secondary endpoints included DAS28-CRP, and safety endpoints were AEs, SAEs, and the incidence of ADAs. A total of 526 patients were randomized and treated with ABP 501 (n = 264) and the adalimumab RP (n = 262). At week 24, ACR20 response rates were 74.6% in the ABP 501 group and 72.4% in the adalimumab RP group. The RR for ABP 501 versus the adalimumab RP was 1.039 (90% CI 0.954–1.133). Clinical equivalence between ABP 501 and the adalimumab RP was demonstrated, as the 90% CI fell within the predefined equivalence margin. The mean change from baseline in DAS28-CRP decreased similarly for both treatment groups over the study period and was – 2.32 for both groups at week 24 (between-group difference, 0.01 [90% CI – 0.18 to 0.17]). In total, 52.3% of patients experienced an AE during the study, with similar percentages of patients reporting an AE in the ABP 501 (50.0%) and adalimumab RP (54.6%) groups. AEs reported by > 3% of patients in either group were nasopharyngitis (6.4%, 7.3%), headache (4.5%, 4.2%), arthralgia (3.0%, 3.4%), cough (2.7%, 3.1%), and upper respiratory tract infection (1.5%, 3.8%) in the ABP 501 and adalimumab RP groups, respectively. Overall, 4.4% of patients experienced an SAE; the percentage of patients with an SAE was similar in both groups (ABP 501, 3.8%; adalimumab RP, 5.0%). No deaths occurred in this study, and no clinically significant changes were observed from laboratory evaluations and vital sign examinations.
In an OLE, 229 patients receiving ABP 501 and 237 receiving the adalimumab RP who completed the final visit in the parent study were treated with 40 mg ABP 501 every other week for 68 weeks. Efficacy was maintained throughout the OLE and no new safety findings emerged in both the ABP 501/ABP 501 and RP/ABP 501 groups. Medication switching did not affect immunogenicity [17].
BI 695501
Based on extensive comparisons regarding the physicochemical structure and biologic function of BI 695501 and the adalimumab RP, BI 695501 has demonstrated structural similarity and comparable functionality [18]. The bioequivalence, safety, and immunogenicity of BI 695501 compared with EU-Humira and US-Humira were studied in a randomized, double-blind, active-comparator phase 1 clinical study in 327 healthy male subjects (n = 109 in each treatment group) who received a single, 40-mg SC dose of BI 695501, EU-Humira, or US-Humira [19]. Three-way PK bioequivalence was demonstrated, as the 90% CIs for the geometric mean ratios of all primary PK parameters (AUC0–t, AUC0-∞, and Cmax, comparing BI 695501 with EU-Humira and US-Humira, and EU-Humira with US-Humira) were within the predefined acceptance ranges of 80% to 125%. In total, 72% of subjects experienced ≥ 1 AEs, with similar percentages across all three groups (BI 695501, 70.4%; EU-Humira, 71.3%; US-Humira, 73.1%). SAEs were reported in 2.8% of the BI 695501 and US-Humira groups, and in 1.9% in the EU-Humira group. No deaths or AEs leading to discontinuation occurred during the study. The percentage of subjects with positive ADA activity at the end of the study was similar across treatment groups (BI 695501, 92.5%; EU-Humira, 84.3%; US-Humira, 88.0%). The percentage of subjects with NAbs at the end of the study, as assessed using a cell-based, antibody-dependent, cell-mediated cytotoxicity method, was also similar for each group (BI 695501, 59.8%; EU-Humira, 58.3%; US-Humira, 63.9%).
The efficacy, safety, and immunogenicity of BI 695501 was compared with the adalimumab RP among patients with moderate-to-severe RA receiving stable MTX in a 58-week, randomized phase 3 equivalence study [18]. Patients were randomized to receive a 40-mg dose of BI 695501 or the adalimumab RP once every 2 weeks for 24 weeks. At week 24, patients in the adalimumab RP group were rerandomized to receive BI 695501 or continue the adalimumab RP. The primary endpoints were ACR20 response rates at 12 and 24 weeks. Efficacy, safety, and immunogenicity were further assessed up to week 58. A total of 645 patients were randomized to the BI 695501 (n = 324) and adalimumab RP (n = 321) treatment groups. At week 24, 593 patients were rerandomized to continuous BI 695501 (n = 298), continuous adalimumab RP (n = 148), and the adalimumab RP to BI 695501 (n = 147). Therapeutic equivalence of BI 695501 and the adalimumab RP was demonstrated, as both primary endpoints met the predefined criteria. At week 12, ACR20 response rates were 67.0% for BI 695501 and 61.1% for the adalimumab RP (difference of 5.9 [90% CI – 0.9 to 12.7]). At week 24, ACR20 response rates were 69.0% for BI 695501 and 64.5% for the adalimumab RP (difference of 4.5 [90% CI – 3.4 to 12.5]). The mean change from baseline in DAS28- erythrocyte sedimentation rate (ESR) was also similar between groups at weeks 24 and 48. The ACR20/50/70 (ACR50/70 are the same measure as ACR20, with improvement levels defined as 50% and 70%, respectively) response rates and mean change from baseline in DAS28-ESR showed a similar trend over the course of 48 weeks across continuous and switched treatment groups. The emergence of AEs and SAEs was similar across treatment groups. The percentage of patients experiencing ≥ 1 AEs over the course of 58 weeks was 59.6%, 63.7%, and 60.0% in the BI 695501 to BI 695501, adalimumab RP to BI 695501, and adalimumab RP to adalimumab RP groups, respectively. In these same groups, 5.6, 6.8, and 9.7%, respectively, experienced ≥ 1 SAEs. AEs leading to study drug discontinuation occurred in 4.0, 4.1, and 6.9% of patients in the BI 695501 to BI 695501, adalimumab RP to BI 695501, and adalimumab RP to adalimumab RP groups, respectively. The proportion of patients who were ADA positive at any time up to week 24 was similar for BI 905501 (47.4%) and the adalimumab RP (53.0%). Switching from the adalimumab RP to BI 95501 did not influence subsequent ADA frequency.
In a long-term OLE, patients who previously received BI 695501 for 48 weeks were assigned to a group (n = 225), patients who previously received adalimumab RP for 24 weeks and were switched to BI 695501 were assigned to another group (n = 102), and patients who previously received adalimumab RP for 48 weeks were assigned to a third group (n = 103). All patients received BI 695501 40 mg/0.8 ml solution every 2 weeks for up to 48 weeks (treatment duration 98 weeks) [20]. The treatment efficacy established in the main trial was maintained throughout the OLE, and no new safety signals were identified. No differences in efficacy, safety, or immunogenicity were seen among the treatment groups [20].
GP2017
Results from sensitive in vitro binding, functional characterization studies, and nonclinical evaluations have established that GP2017 is similar to the adalimumab RP regarding target binding, functional PK, and PD properties [21]. The PK of GP2017 were compared with EU-Humira and US-Humira in a randomized, double-blind, parallel-group study among 316 healthy male subjects [22]. Ten subjects were ADA positive at baseline and were excluded from the PK analysis and two subjects discontinued the study, leaving 306 subjects in the PK analysis set (GP2017, n = 104; EU-Humira, n = 103; US-Humira, n = 99). The primary endpoints in the study were AUC0-∞ and Cmax. The PK equivalence of GP2017, EU-Humira, and US-Humira was demonstrated, as the 90% CIs of the geometric means for the AUC0-∞ and Cmax were within the predefined limits of 0.8 to 1.25 for all comparisons. A total of 70.1% subjects experienced ≥ 1 AEs (GP2017, 71.0%; EU-Humira, 70.8%; US-Humira, 68.6%), most of which were mild to moderate in severity. The most frequently reported AEs were headache (GP2017, 14.0%; EU-Humira, 13.2%; US-Humira, 18.1%), nasopharyngitis (GP2017, 24.3%; EU-Humira, 29.2%; US-Humira, 22.9%), and rhinitis (GP2017, 5.6%; EU-Humira, 14.2%; US-Humira, 10.5%). The two SAEs reported in the study were an angioedema in the GP2017 group and a femoral neck fracture in the US-Humira arm. The angioedema was of moderate intensity and was considered related to the study drug, and the femoral neck fracture was of severe intensity and was not considered related to the study drug. The overall proportion of subjects positive for ADAs was 57.9, 69.8, and 69.5% in the GP2017, EU-Humira, and US-Humira groups, respectively. The majority of ADAs were neutralizing, as assessed using a competitive ligand-binding assay (GP2017, 54.2%; EU-Humira, 64.2%; US-Humira, 62.9%).
The efficacy and safety of GP2017 were compared with the adalimumab RP in a 24-week, randomized, double-blind, parallel-group, multicenter phase 3 study in patients with moderate-to-severe RA with inadequate response to DMARDs, including MTX [23]. A total of 353 patients were randomized to receive a 40-mg SC dose of GP2017 (n = 177) or the adalimumab RP (n = 176). The primary endpoint was change in DAS28-CRP from baseline at week 12. Secondary endpoints included time-weighted average change in DAS28-CRP from baseline to week 24, safety, and immunogenicity. At week 12, the mean change from baseline in DAS28-CRP was – 2.16 for GP2017 (n = 140) and –2.18 for the adalimumab RP (n = 144; mean difference of 0.02 [95% CI – 0.24 to 0.27]). The time-weighted average change from baseline to week 24 in DAS28-CRP was – 1.85 for GP2017 (n = 127) and – 1.93 for the adalimumab RP (n = 138; mean difference, 0.08 [95% CI – 0.11 to 0.27]). AEs were reported in 61.6% of patients in the GP2017 group and in 60.2% of patients in the adalimumab RP group. The majority of AEs were of mild or moderate severity. Infections and infestations were the most common category of AEs, largely driven by mild viral upper respiratory tract infections (GP2017, 14.7%; adalimumab RP, 9.1%). Over 24 weeks, ADAs were detected in 21.8% and 24.4% of patients treated with GP2017 and the adalimumab RP groups, respectively. More than 70% of the ADAs in both groups were neutralizing.
To assess interindividual differences in immunogenicity among the two study populations, a cross-study comparison was completed [24]. Approximately 70% of subjects in the two-arm study were ADA positive versus 58% in the three-arm study. Mean serum concentration–time profiles revealed that exposure was significantly different (lower in the two-arm study population vs the three-arm study), with the 90% CI for geometric mean ratios of AUC0–t and AUC0-∞ outside the prespecified bioequivalence margin of 0.80–1.25. Among those who were ADA negative, the 90% CI was in range for all PK parameters. The authors concluded that the differences between the two groups are not product related, but are the result of unknown differences in the study populations [24].
MSB11022
Biochemical and biophysical analysis was performed on MSB11022 in comparison with the adalimumab RP [25]. MSB11022 was shown to have similar physicochemical and in vitro PD properties [25]. In a phase 1, double-blind, parallel-group study, 237 healthy subjects were randomized to receive a single 40-mg dose of MSB11022, EU-Humira, or US-Humira [26]. MSB11022 demonstrated PK equivalence (90% CI within the 80–125% equivalence margin) to both EU- and US-Humira for AUC0-∞, Cmax, and AUC0–t. Approximately 60% of subjects experienced an AE, but none led to study withdrawal. Two SAEs were reported in the MSB11022 group but were determined to be unrelated to study drug. The most common AEs related to study drugs were headache, injection-site pain, and oropharyngeal pain. No differences in AEs were seen among MSB11022 (63%), EU-Humira (62%), and US-Humira (56%). The detection of ADAs occurred in 82.1% of the MSB11022 group, 83.5% of the EU-Humira group, and 81.3% of the US-Humira group. The presence of ADAs had no effect on PK parameters or the frequency of AEs [26].
In a phase 3, randomized, double-blind, 52-week trial of 288 patients with moderate-to-severe, active RA receiving either MSB11022 (n = 143) or the adalimumab RP (n = 145), the primary endpoint was the incidence of TEAEs of special interest (AESIs) [27]. The ACR20 at week 12 was the key secondary endpoint. At 52 weeks, the incidence of AESIs (hypersensitivity) was similar across treatment groups (MSB11022, 4.2%; adalimumab RP, 5.5%). Two treatment-related hypersensitivity reactions were considered serious, including 1 case of grade 3 dermatitis in the adalimumab RP arm and 1 case of grade 4 anaphylactic reaction in the MSB11022 arm. No treatment-related deaths were reported, and no hypersensitivity reactions led to study discontinuation. The incidence of other TEAEs was similar between treatment arms (MSB11022, 58.0%; adalimumab RP, 64.1%). Approximately 79.6% of patients in the MSB11022 group and 80.9% in the adalimumab RP group achieved ACR20 at week 12 (difference of 1.3% [95% CI –10.55 to 8.04]). The similarity in response between groups was maintained through week 52. Other efficacy endpoints, including ACR50/70, DAS28-ESR, and Simple Disease Activity Index and Clinical Disease Activity Index scores, were all similar across treatment groups up to week 52. The presence of ADAs was confirmed in 80.4% of patients in the MSB11022 arm and 71.7% of patients in the adalimumab RP arm. NAbs were identified in 39.9% of patients in the MSB11022 arm and 39.3% of the adalimumab RP arm [27].
PF-06410293
Characterization of PF-06410293 showed that PF-06410293 is both structurally and functionally similar to US-Humira and EU-Humira [28]. In a double-blind, randomized 78-week study, 597 patients with active RA received either PF-06410293 (n = 297) or adalimumab RP (n = 300) 40 mg subcutaneously every other week, and efficacy, safety, immunogenicity, PK, and PD were evaluated [29]. The primary endpoint was ACR20 at week 12, and therapeutic equivalence was determined if the 95% CI fell between the symmetric equivalence margin of ± 14%. Secondary endpoints included ACR20/50/70, DAS28 based on high-sensitivity CRP (DAS28-4[CRP]), European League Against Rheumatism (EULAR) response, and ACR/EULAR remission at 26 weeks. The percentage of patients achieving the primary endpoint of ACR20 at 12 weeks was 68.7% in the PF-06410293 arm and 72.7% in the adalimumab RP arm (difference of 2.98% [95% CI – 10.38 to 4.44]). According to the prespecified equivalence margin for ACR20 response rates, PF-06410293 and the adalimumab RP were considered therapeutically equivalent. The ACR 20/50/70 response rates at week 26 were also similar between the treatment arms. TheDAS28-4(CRP) mean change from baseline at 26 weeks was – 2.7 for the PF-06410293 group and – 2.8 for the adalimumab RP group, and 29.3% and 33.0% of the PF-06410293 and adalimumab RP groups, respectively, achieved a DAS28-4(CRP) score < 2.6. Approximately 54.5% and 12.8% of the PF-06410293 group and 49.0% and 14.7% of the adalimumab RP group had a good EULAR response and total remission, respectively. TEAEs were reported by 48.1% of patients in the PF-06410293 arm and 47.8% of the adalimumab RP arm. The most frequent AEs were viral upper respiratory tract infections, increased alanine aminotransferase (ALT), hypertension, and headaches. Injection-site reactions occurred in approximately 2% of patients. Serious AEs were reported by 4.0% of patients in the PF-06410293 group and 4.3% of patients in the adalimumab RP group. The presence of ADAs occurred in 44.4% of patients receiving PF-06410293 and 50.5% of patients receiving the adalimumab RP. Of those patients, 31.1% in the PF-06410293 group and 27.8% in the adalimumab RP group tested positive for NAbs [29].
SB5
SB5 was found to have an identical amino acid sequence, as well as similar physicochemical and in vitro functional properties, when compared with the adalimumab RP [30]. A randomized, single-blind phase 1 PK study compared SB5 with EU- and US-Humira among 189 healthy subjects [30]. PK equivalence was demonstrated in this study, as the 90% CIs for all primary PK parameters (AUC0–t, AUC0-∞, and Cmax) were within the predefined limit of 0.8 to 1.25 for all comparisons (SB5 and EU-Humira and US-Humira, and EU-Humira and US-Humira). No deaths or discontinuations as a result of AEs were reported in this study. SAEs were reported for two subjects (one in the SB5 group and one in the US-Humira group) but were not considered related to the study drug. A total of 55.0% of subjects experienced an AE. All AEs were considered mild or moderate in severity and the distribution of AEs was comparable among treatment groups (SB5, 57.1%; EU-Humira, 46.0%; US-Humira, 61.9%). The most commonly reported AEs were nasopharyngitis (16.4%), headache (11.6%), oral herpes (4.8%), and rhinitis (4.8%). The incidence of ADAs to adalimumab was comparable among all 3 treatment groups (SB5, 98.4%; EU-Humira, 95.2%; US-Humira, 100%). Statistical analysis revealed no significant difference in postdose ADA incidence among treatment groups (SB5 and EU-Humira, P = 0.6189; SB5 and US-Humira, P = 1.0000; EU-Humira and US-Humira, P = 0.2440).
The efficacy, PK, safety, and immunogenicity of SB5 compared with the adalimumab RP were evaluated in a randomized, double-blind, parallel-group phase 3 study among patients with moderate-to-severe RA despite treatment with MTX [31]. A total of 544 patients were randomized to receive a 40-mg SC dose of SB5 (n = 271) or the adalimumab RP (n = 273) every 2 weeks over the course of 24 weeks. The primary endpoint for this study was ACR20 response rate at week 24. Secondary endpoints included ACR50/70 response rates and mean change in DAS28-ESR at 24 weeks. The ACR20 response rates at week 24 were 72.4% in the SB5 group and 72.2% in the adalimumab RP group. The adjusted difference (0.1% [95% CI – 7.83 to 8.13%]) was within the predefined equivalence margin. Response rates for the secondary endpoints of ACR50 (SB5, 38.1%; adalimumab RP, 39.7%) and ACR70 (SB5, 19.2%; adalimumab RP, 20.3%) were also equivalent between SB5 and the adalimumab RP (adjusted difference of – 2.0% [95% CI – 10.69 to 6.75%] and – 1.3% [95% CI – 8.41 to 5.80%], respectively). In addition, the LSM for the treatment difference between SB5 and the adalimumab RP was also within the predefined equivalence margin (– 0.04 [95% CI – 0.26 to 0.17). Most AEs in the study were mild to moderate in severity. A total of 35.8% of patients in the SB5 group and 40.7% in the adalimumab RP group experienced an AE. The most common AEs were nasopharyngitis (SB5, 4.9%; adalimumab RP, 9.2%), headache (SB5, 3.4%; adalimumab RP, 2.6%), bronchitis (SB5, 2.6%; adalimumab RP, 2.6%), and an increase in ALT level (SB5, 2.2%; adalimumab RP, 2.9%). SAEs were reported in 1.1% of patients in the SB5 group and 2.9% in the adalimumab RP group. The incidence of ADAs up to week 24 was similar between the SB5 group (33.1%) and the adalimumab RP group (32.0%). Approximately half of the ADAs were neutralizing in both treatment groups, as assessed using a ligand-binding bioassay.
In a 52-week switching study, patients from the 24-week study were rerandomized to receive the adalimumab RP (adalimumab RP to adalimumab RP, n = 129), switch to SB5 (adalimumab RP to SB5, n = 125), or continue receiving SB5 (SB5, n = 254) [32]. The ACR response rates at 24 weeks were maintained through 52 weeks and were comparable among all groups; switching did not affect efficacy. AEs were comparable among groups, as was the incidence of ADAs, and switching did not increase either [32].
Discussion
In summary, all the adalimumab biosimilars reviewed in this article (FKB327, ABP 501, BI 695501, GP2017, MSB11022, PF-06410293, and SB5) were found to have the expected structure of a human IgG1-type antibody, were highly similar to the adalimumab RP in physicochemical and biological properties, and were similar to the adalimumab RP in PK parameters. These biosimilars also demonstrated comparable efficacy to the adalimumab RP in the treatment of RA. In addition, single- and double-switching treatment between FKB327 and the adalimumab RP, and single switching between BI 695501 and the adalimumab RP, ABP 501 and the adalimumab RP, and SB5 and the adalimumab RP were not associated with differences from the RP in efficacy, safety, trough serum drug concentration, or immunogenicity. These biosimilars all demonstrated similar safety, tolerability, and immunogenicity compared with the adalimumab RP across all studies. Finally, FKB327 and ABP 501 are associated with less injection-site pain, because they do not include the citrate—which is known to cause stinging and pain—that is found in adalimumab RP [33, 34].
The percentage of patients positive for ADAs in the studies reviewed here is consistent with those reported elsewhere [35, 36]. Both non-neutralizing antibodies and NAbs can impact clinical responses to biologics by forming immune complexes that may affect their PK, such as increased clearance, as well as result in lower drug serum concentrations [35]. A study to assess the relationship among the development of ADAs, adalimumab levels, and disease activity in patients with RA showed that although ADAs were associated with decreasing circulating levels of adalimumab, there was no direct effect on disease activity as assessed using the DAS28 [37]. However, this study reported a negative correlation between free adalimumab trough levels and DAS.
The studies reviewed here did not directly assess the effect of NAb and non-neutralizing ADA activity on disease activity; however, for all biosimilars reviewed here, the percentage of patients testing positive for ADAs and the percentage of ADAs determined to be neutralizing were similar to the adalimumab RP. Thus, based on the totality of the evidence reviewed here, these biosimilars are expected to perform in a manner comparable to the adalimumab RP.
Conclusions
Treatment with bDMARDs has significantly improved clinical outcomes in patients with RA and has been shown to improve symptoms, reduce joint inflammation, limit erosive damage, decrease disability, and improve quality of life. Despite improved outcomes associated with bDMARDs, many patients throughout the world do not have access to these treatments. This necessitates worldwide improved access to biological agents for patients with RA.
Biosimilars are cost-effective alternatives to their RPs and serve as an opportunity to increase patient access to bDMARDs. Specific regulatory requirements in the United States and European Union must be met for the approval of biosimilars. In the European Union, EMA guidance details product-specific approval pathways based on biological classification, whereas in the United States, the FDA utilizes a risk-based, case-by-case, totality-of-evidence approach [38]. A potential biosimilar must demonstrate similarity to the reference biologic with regard to structure and function, PK, efficacy, safety, and immunogenicity [39].
Although multiple biosimilars for several bio-originators have been approved in the US and/or EU, this article focuses on the 7 adalimumab biosimilars. A review of the data for the biosimilars FKB327, ABP 501, BI 695501, GP2017, MSB11022, PF-06410293, and SB5 confirmed all these products are similar to the adalimumab RP with regard to structure, physicochemical and biological properties, and PK. Furthermore, comparable efficacy in the treatment of RA between these biosimilars and the adalimumab RP has also been established. A summary of these findings is shown in Table 4. In addition, single- and double-switching between the biosimilar and RP assessed in studies with FKB327 and single-switching assessed with BI 695501, ABP 501, and SB5 did not reveal any differences in efficacy, safety, trough serum drug concentration, or immunogenicity between the biosimilar and the RP. Across all studies, similar safety, tolerability, and immunogenicity were demonstrated between the biosimilars and the adalimumab RP.
References
Scott DL. Biologics-based therapy for the treatment of rheumatoid arthritis. Clin Pharmacol Ther. 2012;91:30–43.
Baumgart DC, Misery L, Naeyaert S, Taylor PC. Biological therapies in immune-mediated inflammatory diseases: can biosimilars reduce access inequities? Front Pharmacol. 2019;10:279.
Smolen JS, Landewé R, Bijlsma J, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann Rheum Dis. 2017;76:960–77.
World Health Organization, Expert Committee on Biological Standardization. Guidelines on evaluation of similar biotherapeutic products (SBPs). 2009. www.who.int/biologicals/areas/biological_therapeutics/BIOTHERAPEUTICS_FOR_WEB_22APRIL2010.pdf. Accessed April 26, 2019.
IMS Institute for Healthcare Informatics. Delivering on the potential of biosimilar medicines, the role of functioning competitive markets. March 2016. www.medicinesforeurope.com/wp-content/uploads/2016/03/IMS-Institute-Biosimilar-Report-March-2016-FINAL.pdf. Accessed April 27, 2019.
US Food and Drug Administration. Scientific considerations in demonstrating biosimilarity to a reference product, guidance for industry. April 2015. www.fda.gov/media/82647/download. Accessed April 22, 2019.
European Medicines Agency. Guideline on similar biological medicinal products. October 23, 2014. www.ema.europa.eu/docs/en_GB/document_library/Scientific_guideline/2014/10/WC500176768.pdf. Accessed April 22, 2019.
US Food and Drug Administration. Prescribing biosimilar and interchangeable products. October 23, 2017. www.fda.gov/drugs/biosimilars/prescribing-biosimilar-and-interchangeable-products. Accessed May 8, 2019.
European Medicines Agency. Assessment report: Hulio. 2018. www.ema.europa.eu/en/documents/assessment-report/hulio-epar-public-assessment-report_en.pdf. Accessed April 22, 2019.
Puri A, Niewiarowski A, Arai Y, et al. Pharmacokinetics, safety, tolerability and immunogenicity of FKB327, a new biosimilar medicine of adalimumab/Humira, in healthy subjects. Br J Clin Pharmacol. 2017;83:1405–15.
Genovese MC, Glover J, Greenwald M, et al. FKB327, an adalimumab biosimilar, versus the reference product: results of a randomized, phase III, double-blind study, and its open-label extension. Arthritis Res Ther. 2019;21:281.
Genovese MC, Kellner H, Arai Y, Muniz R, Alten R. Long-term safety, immunogenicity and efficacy comparing FKB327 with the adalimumab reference product in patients with active rheumatoid arthritis: data from randomised double-blind and open-label extension studies. RMD Open. 2020;6(1):e000987.
Velayudhan J, Chen YF, Rohrbach A, et al. Demonstration of functional similarity of proposed biosimilar ABP 501 to adalimumab. BioDrugs. 2016;30:339–51.
Liu J, Eris T, Li C, Cao S, Kuhns S. Assessing analytical similarity of proposed Amgen biosimilar ABP 501 to adalimumab. BioDrugs. 2016;30:321–38.
Kaur P, Chow V, Zhang N, Moxness M, Kaliyaperumal A, Markus R. A randomised, single-blind, single-dose, three-arm, parallel-group study in healthy subjects to demonstrate pharmacokinetic equivalence of ABP 501 and adalimumab. Ann Rheum Dis. 2017;76:526–33.
Cohen S, Genovese MC, Choy E, et al. Efficacy and safety of the biosimilar ABP 501 compared with adalimumab in patients with moderate to severe rheumatoid arthritis: a randomised, double-blind, phase III equivalence study. Ann Rheum Dis. 2017;76:1679–87.
Cohen S, Pablos JL, Pavelka K, et al. An open-label extension study to demonstrate long-term safety and efficacy of ABP 501 in patients with rheumatoid arthritis. Arthritis Res Ther. 2019;21:84.
Cohen SB, Alonso-Ruiz A, Klimiuk PA, et al. Similar efficacy, safety and immunogenicity of adalimumab biosimilar BI 695501 and Humira reference product in patients with moderately to severely active rheumatoid arthritis: results from the phase III randomised VOLTAIRE-RA equivalence study. Ann Rheum Dis. 2018;77:914–21.
Wynne C, Altendorfer M, Sonderegger I, et al. Bioequivalence, safety and immunogenicity of BI 695501, an adalimumab biosimilar candidate, compared with the reference biologic in a randomized, double-blind, active comparator phase I clinical study (VOLTAIRE®-PK) in healthy subjects. Expert Opin Investig Drugs. 2016;25:1361–70.
Cohen SB, Czeloth N, Lee E, et al. Long-term safety, efficacy, and immunogenicity of adalimumab biosimilar BI 695501 and adalimumab reference product in patients with moderately-to-severely active rheumatoid arthritis: results from a phase 3b extension study (VOLTAIRE-RAext). Expert Opin Biol Ther. 2019;19:1097–105.
Kronthaler U, Fritsch C, Hainzl O, Seidl A, da Silva A. Comparative functional and pharmacological characterization of Sandoz proposed biosimilar adalimumab (GP2017): rationale for extrapolation across indications. Expert Opin Biol Ther. 2018;18:921–30.
von Richter O, Lemke L, Haliduola H, et al. GP2017, an adalimumab biosimilar: pharmacokinetic similarity to its reference medicine and pharmacokinetics comparison of different administration methods. Expert Opin Biol Ther. 2019;19:1075–83.
Wiland P, Jeka S, Dokoupilová E, et al. A randomized, double-blind, parallel-group, multicenter study to compare the efficacy, safety and immunogenicity of a proposed adalimumab biosimilar (GP2017) with reference adalimumab in patients with moderate-to-severe active rheumatoid arthritis. Arthritis Rheumatol. 2018;70(Suppl 9):Abstract 1936.
von Richter O, Lemke L, Haliduola H, et al. Differences in immunogenicity associated with non-product related variability: insights from two pharmacokinetic studies using GP2017, an adalimumab biosimilar. Expert Opin Biol Ther. 2019;19:1057–64.
Magnenat L, Palmese A, Fremaux C, et al. Demonstration of physicochemical and functional similarity between the proposed biosimilar adalimumab MSB11022 and Humira®. MAbs. 2017;9:127–39.
Hyland E, Mant T, Vlachos P, et al. Comparison of the pharmacokinetics, safety, and immunogenicity of MSB11022, a biosimilar of adalimumab, with Humira(®) in healthy subjects. Br J Clin Pharmacol. 2016;82:983–93.
Edwards CJ, Monnet J, Ullmann M, et al. Safety of adalimumab biosimilar MSB11022 (acetate-buffered formulation) in patients with moderately-to-severely active rheumatoid arthritis. Clin Rheumatol. 2019;38:3381–90.
Derzi M, Shoieb A, Ripp SL, et al. Comparative nonclinical assessments of the biosimilar PF-06410293 and originator adalimumab. Regul Toxicol Pharmacol. 2020;112:104587.
Fleischmann RM, Alten R, Pileckyte M, et al. A comparative clinical study of PF-06410293, a candidate adalimumab biosimilar, and adalimumab reference product (Humira®) in the treatment of active rheumatoid arthritis. Arthritis Res Ther. 2018;20:178.
Shin D, Lee Y, Kim H, Körnicke T, Fuhr R. A randomized phase I comparative pharmacokinetic study comparing SB5 with reference adalimumab in healthy volunteers. J Clin Pharm Ther. 2017;42:672–8.
Weinblatt ME, Baranauskaite A, Niebrzydowski J, et al. Phase III randomized study of SB5, an adalimumab biosimilar, versus reference adalimumab in patients with moderate-to-severe rheumatoid arthritis. Arthritis Rheumatol. 2018;70:40–8.
Weinblatt ME, Baranauskaite A, Dokoupilova E, et al. Switching from reference adalimumab to SB5 (adalimumab biosimilar) in patients with rheumatoid arthritis: fifty-two-week phase III randomized study results. Arthritis Rheumatol. 2018;70:832–40.
Kellner H, Boyce M, Genovese MC, Alten R, Ito T, Yonemura T. Systematic analysis of injection-site pain and reactions caused by subcutaneous administration of the adalimumab biosimilar FKB327 versus the adalimumab reference product via different delivery methods. GaBI J. 2020;9.
Krishnan E, Zhang N, Wang H. P497 injection site reactions and injection site pain for the adalimumab biosimilar ABP 501: Results from two double-blind, randomised, controlled studies. J Crohns Colitis. 2018;12(suppl 1):S357.
Strand V, Balsa A, Al-Saleh J, et al. Immunogenicity of biologics in chronic inflammatory diseases: a systematic review. BioDrugs. 2017;31:299–316.
Keiserman M, Codreanu C, Handa R, et al. The effect of antidrug antibodies on the sustainable efficacy of biologic therapies in rheumatoid arthritis: practical consequences. Expert Rev Clin Immunol. 2014;10:1049–57.
Cludts I, Spinelli FR, Morello F, Hockley J, Valesini G, Wadhwa M. Anti-therapeutic antibodies and their clinical impact in patients treated with the TNF antagonist adalimumab. Cytokine. 2017;96:16–23.
Daller J. Biosimilars: a consideration of the regulations in the United States and European union. Regul Toxicol Pharmacol. 2016;76:199–208.
Isakov L, Jin B, Jacobs IA. Statistical primer on biosimilar clinical development. Am J Ther. 2016;23:e1903–10.
Acknowledgements
Funding
Funding for the journal’s Rapid Service Fee was provided by Mylan Inc.
Medical Writing and Editorial Assistance
Technical, editorial, and medical writing assistance were provided under the direction of the authors by Stephanie A. Breslan, MS, and Strategix, an affiliate of The Lynx Group LLC. Funding for this support was provided by Mylan Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors criteria for authorship. All authors made substantial contributions to the conception or design of the work or the acquisition, analysis, or interpretation of data. All authors were fully responsible for drafting the work or revising it critically for important intellectual content. The authors made all content and editorial decisions and received no financial support or other form of compensation related to the development of this manuscript. All authors had final approval of the manuscript and are accountable for all aspects of the work in ensuring the accuracy and integrity of this manuscript. No deserving authors have been omitted.
Disclosures
Tom W.J. Huizinga/the Department of Rheumatology at LUMC has received research support, lecture fees, and consultancy fees from Ablynx, Merck, UCB, Bristol Myers Squibb, Biotest AG, Janssen, Pfizer, Novartis, Roche, Sanofi-Aventis, Abbott, Crescendo Bioscience, Galapagos, Nycomed, Boehringer Ingelheim, Takeda, Zydus, Epirus, and Eli Lilly. Yoshifumi Torii is an employee of Fujifilm Kyowa Kirin Biologics. Rafael Muniz is an employee and shareholder of Mylan Inc.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article, as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Huizinga, T.W.J., Torii, Y. & Muniz, R. Adalimumab Biosimilars in the Treatment of Rheumatoid Arthritis: A Systematic Review of the Evidence for Biosimilarity. Rheumatol Ther 8, 41–61 (2021). https://doi.org/10.1007/s40744-020-00259-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40744-020-00259-8