Abstract
Background
Excessive alcohol intake complicated by liver dysfunction has been presumed to affect skeletal muscles. This study aimed to examine the association between excessive alcohol intake, liver fibrosis, and loss of skeletal muscle mass in elderly men.
Methods
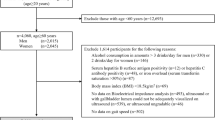
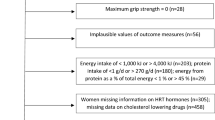
The study participants comprised 799 community-dwelling elderly men (age, 71 ± 3 years) with no history of treatment for liver disease. Bioelectrical impedance analysis was performed to estimate the appendicular skeletal muscle mass (ASM) of each participant. The ASM values were also normalized for height (ASM index). Liver fibrosis was evaluated using the Fib4 index, which was calculated using participant age, AST level, ALT level, and platelet count. Usual alcohol intake was estimated based on the type of alcohol, frequency of drinking, and amount of alcohol consumed per day.
Results
Among the excess drinkers (≥ 20 g/day), the ASM index of the subgroup with liver fibrosis (Fib4 index ≥ 2.67) was significantly lower than that of the subgroup with no liver fibrosis (Fib4 index < 2.67). However, no significant difference between the subgroups was found in the non-drinkers and moderate drinkers (< 20 g/day). In multiple regression analysis, the Fib4 index was significantly associated with the ASM index, independent of potential confounding factors. The association between the Fib4 index and ASM index was more pronounced in excess drinkers than in non-drinkers and moderate drinkers.
Conclusion
These results suggest that liver fibrosis is associated with loss of skeletal muscle mass in elderly men, and excessive alcohol intake combined with liver fibrosis may lead to greater muscle mass reduction than each individual condition.
Similar content being viewed by others
References
Fielding RA, Vellas B, Evans WJ et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12:249–256. https://doi.org/10.1016/j.jamda.2011.01.003
Cruz-Jentoft AJ, Landi F, Schneider SM et al (2014) Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 43:748–759. https://doi.org/10.1093/ageing/afu115
Santilli V, Bernetti A, Mangone M et al (2014) Clinical definition of sarcopenia. Clin Cases Miner Bone Metab 11:177–180
Kim JA, Choi KM (2019) Sarcopenia and fatty liver disease. Hepatol Int 13:674–687. https://doi.org/10.1007/s12072-019-09996-7
Steffl M, Bohannon RW, Petr M et al (2016) Alcohol consumption as a risk factor for sarcopenia—a meta-analysis. BMC Geriatr 16:99. https://doi.org/10.1186/s12877-016-0270-x
Sung JH, Uojima H, Hidaka H et al (2019) Risk factors for loss of skeletal muscle mass in patients with cirrhosis. Hepatol Res 49:550–558. https://doi.org/10.1111/hepr.13308
Hanai T, Shiraki M, Ohnishi S et al (2016) Rapid skeletal muscle wasting predicts worse survival in patients with liver cirrhosis. Hepatol Res 46:743–751. https://doi.org/10.1111/hepr.12616
Kamachi S, Mizuta T, Otsuka T et al (2016) Sarcopenia is a risk factor for the recurrence of hepatocellular carcinoma after curative treatment. Hepatol Res 46:201–208. https://doi.org/10.1111/hepr.12562
Onishi S, Miyai N, Utsumi M et al (2016) Liver fibrosis is associated with loss of skeletal muscle mass in community-dwelling older adults with no history of liver diseases. Jpn J Hyg 74:1–10. https://doi.org/10.1265/jjh.18031
Simon L, Jolley SE, Molina PE (2017) Alcoholic myopathy: pathophysiologic mechanisms and clinical implications. Alcohol Res 38:207–217
Haugvad A, Haugvad L, Hamarsland H, Paulsen G (2014) Ethanol does not delay muscle recovery but decreases testosterone/cortisol ratio. Med Sci Sports Exerc 46:2175–2183. https://doi.org/10.1249/MSS.0000000000000339
Hong-Brown LQ, Frost RA, Lang CH (2001) Alcohol impairs protein synthesis and degradation in cultured skeletal muscle cells. Alcohol Clin Exp Res 25:1373–1382. https://doi.org/10.1111/j.1530-0277.2001.tb02361.x
Lang CH, Frost RA, Vary TC (2007) Skeletal muscle protein synthesis and degradation exhibit sexual dimorphism after chronic alcohol consumption but not acute intoxication. Am J Physiol Endocrinol Metab 292:497–506. https://doi.org/10.1152/ajpendo.00603.2006
Korzick DH, Sharda DR, Pruznak AM et al (2013) Aging accentuates alcohol-induced decrease in protein synthesis in gastrocnemius. Am J Physiol Regul Integr Comp Physiol 304:887–898. https://doi.org/10.1152/ajpregu.00083.2013
The Ministry of Health, Labor and Welfare (2012) A basic direction for comprehensive implementation of national health promotion, Japan. https://www.mhlw.go.jp/file/06-Seisakujouhou-10900000-Kenkoukyoku/0000047330.pdf. Accessed 27 Apr 2021
Craig CL, Marshall AL, Sjöström M et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35:1381–1395. https://doi.org/10.1249/01.mss.0000078923.96621.1d
Van der Ploeg HP, Chey T, Korda RJ et al (2012) Sitting time and all-cause mortality risk in 222 497 Australian adults. Arch Intern Med 172:494–500. https://doi.org/10.1001/archinternmed.2011.2174
Tanaka N, Miyatani M, Masuo Y et al (2007) Applicability of a segmental bioelectrical impedance analysis for predicting the whole body skeletal muscle volume. J Appl Physiol 103:1688–1695. https://doi.org/10.1152/japplphysiol.00255.2007
Miyatani M, Kanehisa H, Masuo Y et al (2001) Validity of estimating limb muscle volume by bioelectrical impedance. J Appl Physiol 91:386–394. https://doi.org/10.1152/jappl.2001.91.1.386
Baumgartner RN, Koehler KM, Gallagher D et al (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763. https://doi.org/10.1093/oxfordjournals.aje.a009520
Sterling RK, Lissen E, Clumeck N et al (2006) Development of a simple noninvasive index to predict significant fibrosis in patients with HIV/HCV coinfection. Hepatology 43:1317–1325. https://doi.org/10.1002/hep.21178
Sumida Y, Yoneda M, Hyogo H et al (2012) Validation of the Fib4 index in a Japanese nonalcoholic fatty liver disease population. BMC Gastroenterol 12:1–9. https://doi.org/10.1186/1471-230X-12-2
Shah AG, Lydecker A, Murray K et al (2009) Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol 7:1104–1112. https://doi.org/10.1016/j.cgh.2009.05.033
Gao B, Bataller R (2011) Alcoholic liver disease: pathogenesis and new therapeutic targets. Gastroenterology 141:1572–1585. https://doi.org/10.1053/j.gastro.2011.09.002
Ma X, Svegliati-Baroni G, Poniachik J et al (1997) Collagen synthesis by liver stellate cells is released from its normal feedback regulation by acetaldehyde-induced modification of the carboxyl—terminal propeptide of procollagen. Alcohol Clin Exp Res 21:1204–1211. https://doi.org/10.1111/j.1530-0277.1997.tb04439.x
Hepatitis Information Center (2020) The diagnostic criteria for alcoholic liver disease (version 2011), Japan. http://www.kanen.ncgm.go.jp/cont/010/alcohol.html. Accessed 27 Apr 2021
Ekstedt M, Franzen LE, Holmqvist M et al (2009) Alcohol consumption is associated with progression of hepatic fibrosis in non-alcoholic fatty liver disease. Scand J Gastroenterol 44:366–374. https://doi.org/10.1080/00365520802555991
Dasarathy J, McCullough AJ, Dasarathy S (2017) Sarcopenia in alcoholic liver disease: clinical and molecular advances. Alcohol Clin Exp Res 41:1419–1431. https://doi.org/10.1111/acer.13425
Castillo EM, Goodman-Gruen D, Kritz-Silverstein D (2003) Sarcopenia in elderly men and women: the Rancho Bernardo study. Am J Prev Med 25:226–231. https://doi.org/10.1016/S0749-3797(03)00197-1
Park S, Ham JO, Lee BK (2014) A positive association of vitamin D deficiency and sarcopenia in 50 year old women, but not men. Clin Nutr 33:900–905. https://doi.org/10.1016/j.clnu.2013.09.016
Steffl M, Bohannon RW, Petr M et al (2015) Relation between cigarette smoking and sarcopenia: meta-analysis. Physiol Res 64:419–426. https://doi.org/10.33549/physiolres.932802
Yoshimura K, Sato S, Shigeo M et al (2018) Interdependence of physical inactivity, loss of muscle mass and low dietary intake: extrapulmonary manifestations in older chronic obstructive pulmonary disease patients. Geriatr Gerontol Int 18:88–94. https://doi.org/10.1111/ggi.13146
Sugimoto K, Tabara Y, Ikegami H et al (2019) Hyperglycemia in non-obese patients with type 2 diabetes is associated with low muscle mass: the multicenter study for clarifying evidence for sarcopenia in patients with diabetes mellitus. J Diabetes Investig 10:1471–1479. https://doi.org/10.1111/jdi.13070
Funding
This work was supported by JSPS KAKENHI (Grant Numbers: JP25350894, 17K01861, 18H03054, and 19K10581).
Author information
Authors and Affiliations
Contributions
SO conceived the study design, data collection, statistical analysis, and interpretation, and drafted the manuscript. NM contributed to the statistical analysis, interpretation, drafting, and final revision of the manuscript. YZ, EN, and TO contributed to the data collection and interpretation. MU and MA contributed to the conception and design of the work, drafting, and final revision of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest associated with this manuscript.
Statement of human and animal rights
All procedures performed in this study were approved by the ethical committee of Wakayama Medical University (approval number 92) and in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent and clearance for the use of examination data were obtained from the participants after explaining the purpose of the study and the experimental procedures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Onishi, S., Miyai, N., Zhang, Y. et al. Excessive alcohol intake and liver fibrosis are associated with skeletal muscle mass reduction in elderly men: the Wakayama study. Aging Clin Exp Res 34, 185–192 (2022). https://doi.org/10.1007/s40520-021-01902-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40520-021-01902-2