Opinion statement
Purpose of review The management of treatment-resistant posttraumatic stress disorder (TRPTSD) is a complex clinical challenge, and many patients may continue to endure a heavy symptom burden, even despite the best available treatments. We review the recent literature to provide an update on the evidence base and offer guidance to clinicians on available approaches, including a number of novel and emerging options.
Recent findings If adequate trials of treatment with first-line antidepressants (SSRIs or venlafaxine) or trauma-focused psychotherapy have failed, dosage increase, switching to an alternative first-line option, or combining medication and psychotherapy are reasonable initial approaches. If these remain insufficient, augmentation strategies should be offered, including addition of second-generation antipsychotics (such as risperidone) or the adrenergic antagonist prazosin (especially if sleep disturbance or nightmares are problematic). Further options include the use of other antidepressants (most notably mirtazapine, duloxetine, and trazodone), and the anticonvulsants topiramate or lamotrigine, though the evidence for these is relatively weak. Having tried all these possibilities, the clinician may wish to suggest complementary approaches such as yoga, mindfulness meditation, or acupuncture for symptom reduction and overall well-being. Emerging alternatives, if available, could also be considered, such as augmentation of exposure therapy with d-cycloserine or MDMA, or the use of device-based brain stimulation (such as transcranial magnetic stimulation), though the evidence for these is still preliminary.
Summary Comprehensive assessment of TRPTSD, including a thorough evaluation of associated comorbidity, should inform individualized care, incorporating a process of shared decision-making. Despite the complex clinical challenge of TRPTSD, clinicians should remain hopeful however, that translational neuroscience and clinical trials of emerging approaches will allow progressively better treatment alternatives to be established.

Similar content being viewed by others
References and Recommended Reading
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
American Psychiatric Association. The Diagnostic and Statistical Manual (5th ed.). 5th ed. Washington, DC: American Psychiatric Publishing; 2013.
•• Koek RJ, Schwartz HN, Scully S, Langevin JP, Spangler S, Korotinsky A, et al. Treatment-refractory posttraumatic stress disorder (TRPTSD): a review and framework for the future. Prog Neuro-Psychopharmacol Biol Psychiatry. 2016;70:170–218. Comprehensive review of the literature relating to treatment resistant PTSD.
Rodriguez P, Holowka DW, Marx BP. Assessment of posttraumatic stress disorder-related functional impairment: a review. J Rehabil Res Dev. 2012;49(5):649–65.
Brady KT, Killeen TK, Brewerton T, Lucerini S. Comorbidity of psychiatric disorders and posttraumatic stress disorder. J clin psychiatry. 2000;61(Suppl 7):22–32.
Dorrington S, Zavos H, Ball H, McGuffin P, Rijsdijk F, Siribaddana S, et al. Trauma, post-traumatic stress disorder and psychiatric disorders in a middle-income setting: prevalence and comorbidity. Br J Psychiatry. 2014;205(5):383–9.
Koenen KC, Ratanatharathorn A, Ng L, McLaughlin KA, Bromet EJ, Stein DJ, et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med 2017;47(13):2260-74.
Milliken CS, Auchterlonie JL, Hoge CW. Longitudinal assessment of mental health problems among active and reserve component soldiers returning from the Iraq war. JAMA. 2007;298(18):2141–8.
VA/DOD. VA/DOD Clinical Practice Guideline for the management of posttraumatic stress disorder and acute stress disorder. Washington (DC): Department of Veterans Affairs, Department of Defense; 2017. Available from: https://www.healthquality.va.gov/guidelines/MH/ptsd/. Comprehensive guideline for PTSD, including treatment resistance, detailed discussion of evidence behind recommendations.
Ipser JC, Stein DJ. Evidence-based pharmacotherapy of post-traumatic stress disorder (PTSD). Int J Neuropsychopharmacol. 2012;15(6):825–40.
Katz C, Stein M, Richardson JD, Seedat S, Sareen J. A review of interventions for treatment-resistant posttraumatic stress disorder. In: Selek S, editor. Different views on anxiety disorders: InTech; 2011, p. 251-69. Useful overview chapter on treatment resistant PTSD.
Berger W, Mendlowicz MV, Marques-Portella C, Kinrys G, Fontenelle LF, Marmar CR, et al. Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: a systematic review. Prog Neuro-Psychopharmacol Biol Psychiatry. 2009;33(2):169–80.
Bernardy NC, Friedman MJ. Psychopharmacological strategies in the management of posttraumatic stress disorder (PTSD): what have we learned? Curr psychiatry rep. 2015;17(4):564.
Ahearn EP, Juergens T, Cordes T, Becker T, Krahn DA. Review of atypical antipsychotic medications for posttraumatic stress disorder. Int Clin Psychopharmacol. 2011;26(4):193–200.
• Pruiksma KE, Taylor DJ, Wachen JS, Mintz J, Young-McCaughan S, Peterson AL, et al. Residual sleep disturbances following PTSD treatment in active duty military personnel. Psychol trauma : theory res prac policy. 2016;8(6):697–701. Helpful review regarding sleep disturbance as a refractory PTSD symptom.
Schmidt U. A plea for symptom-based research in psychiatry. Eur J Psychotraumatol. 2015;6(1).
• Kelmendi B, Adams TG, Yarnell S, Southwick S, Abdallah CG, Krystal JH. PTSD: from neurobiology to pharmacological treatments. Eur J Psychotraumatol. 2016;7:31858. Summarises the translational research relating to pharmacology in PTSD.
Steckler T, Risbrough V. Pharmacological treatment of PTSD—established and new approaches. Neuropharmacology. 2012;62(2):617–27.
Ravindran LN, Stein MB. Pharmacotherapy of PTSD: premises, principles, and priorities. Brain Res. 2009;1293:24–39.
Averill LA, Purohit P, Averill CL, Boesl MA, Krystal JH, Abdallah CG. Glutamate dysregulation and glutamatergic therapeutics for PTSD: evidence from human studies. Neurosci Lett. 2017;649:147–55.
Myers KM, Carlezon WA Jr, Davis M. Glutamate receptors in extinction and extinction-based therapies for psychiatric illness. Neuropsychopharmacol : off pub Am College Neuropsychopharmacol. 2011;36(1):274–93.
Marin MF, Camprodon JA, Dougherty DD, Milad MR. Device-based brain stimulation to augment fear extinction: implications for PTSD treatment and beyond. Depress Anxiety. 2014;31(4):269–78.
Thomas E, Stein DJ. Novel pharmacological treatment strategies for posttraumatic stress disorder. Expert Rev Clin Pharmacol. 2017;10(2):167–77.
Ursano RJ, Bell C, Eth S, Friedman M, Norwood A, Pfefferbaum B, et al. Practice guideline for the treatment of patients with acute stress disorder and posttraumatic stress disorder. Am J Psychiatry. 2004;161(11 Suppl):3–31.
Hoge CW, Grossman SH, Auchterlonie JL, Riviere LA, Milliken CS, Wilk JE. PTSD treatment for soldiers after combat deployment: low utilization of mental health care and reasons for dropout. Psychiatric services (Washington, DC). 2014;65(8):997–1004.
Meltzer EC. Discrepancy in diagnosis and treatment of post-traumatic stress disorder (PTSD): Treatment for the wrong reason. J Behav Health Serv Res. 2012;39(2):190–201.
Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, Friedman MJ. Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. J clin psychiatry. 2013;74(6):e541–50.
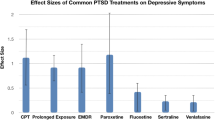
•• Lee DJ, Schnitzlein CW, Wolf JP, Vythilingam M, Rasmusson AM, Hoge CW. Psychotherapy versus pharmacotherapy for posttraumatic stress disorder: systemic review and meta-analyses to determine first-line treatments. Depress Anxiety. 2016;33(9):792–806. Comprehensive systematic review and meta-analysis with balanced discussion of role of pharmacotherapy.
Hoskins M, Pearce J, Bethell A, Dankova L, Barbui C, Tol WA, et al. Pharmacotherapy for post-traumatic stress disorder: systematic review and meta-analysis. Br J Psychiatry. 2015;206(2):93–100. Recent meta-analysis with a useful discussion on quality of evidence
Baldwin DS, Anderson IM, Nutt DJ, Allgulander C, Bandelow B, den Boer JA, et al. Evidence-based pharmacological treatment of anxiety disorders, post-traumatic stress disorder and obsessive-compulsive disorder: a revision of the 2005 guidelines from the British Association for Psychopharmacology. J Psychopharmacol. 2014;28(5):403–39.
Brownlow JA, Harb GC, Ross RJ. Treatment of sleep disturbances in post-traumatic stress disorder: a review of the literature. Current psychiatry rep. 2015;17(6):41.
• Sessa B. MDMA and PTSD treatment: “PTSD: from novel pathophysiology to innovative therapeutics”. Neurosci Lett. 2017;649:176–80. Useful introduction to the potential role of MDMA as an adjunct to psychotherapy in PTSD.
Marshall RD, Beebe KL, Oldham M, Zaninelli R. Efficacy and safety of paroxetine treatment for chronic PTSD: a fixed-dose, placebo-controlled study. Am J Psychiatr. 2001;158(12):1982–8.
• Dunlop BW, Kaye JL, Youngner C, Rothbaum B. Assessing treatment-resistant posttraumatic stress disorder: the Emory treatment resistance interview for PTSD (E-TRIP). Behavi Sci. 2014;4(4):511–27. Discusses a standardised approach to the evaluation of treatment resistance in PTSD.
Bandelow B, Sher L, Bunevicius R, Hollander E, Kasper S, Zohar J, et al. Guidelines for the pharmacological treatment of anxiety disorders, obsessive-compulsive disorder and posttraumatic stress disorder in primary care. Int J Psychiatry Clin Pract. 2012;16(2):77–84.
Jakubovski E, Varigonda AL, Freemantle N, Taylor MJ, Bloch MH. Systematic review and meta-analysis: dose-response relationship of selective serotonin reuptake inhibitors in major depressive disorder. Am J Psychiatry. 2016;173(2):174–83.
Debonnel G, Saint-Andre E, Hebert C, de Montigny C, Lavoie N, Blier P. Differential physiological effects of a low dose and high doses of venlafaxine in major depression. Int J Neuropsychopharmacol. 2007;10(1):51–61.
Rush AJ, Trivedi MH, Wisniewski SR, Stewart JW, Nierenberg AA, Thase ME, et al. Bupropion-SR, sertraline, or venlafaxine-XR after failure of SSRIs for depression. N Engl J Med. 2006;354(12):1231–42.
Hamner MB, Frueh BC. Response to venlafaxine in a previously antidepressant treatment-resistant combat veteran with post-traumatic stress disorder. Int Clin Psychopharmacol. 1998;13(5):233–4.
Simon NM, Connor KM, Lang AJ, Rauch S, Krulewicz S, LeBeau RT, et al. Paroxetine CR augmentation for posttraumatic stress disorder refractory to prolonged exposure therapy. J clin psychiatry. 2008;69(3):400–5.
Rothbaum BO, Cahill SP, Foa EB, Davidson JR, Compton J, Connor KM, et al. Augmentation of sertraline with prolonged exposure in the treatment of posttraumatic stress disorder. J Trauma Stress. 2006;19(5):625–38.
Otto MW, Hinton D, Korbly NB, Chea A, Ba P, Gershuny BS, et al. Treatment of pharmacotherapy-refractory posttraumatic stress disorder among Cambodian refugees: a pilot study of combination treatment with cognitive-behavior therapy vs sertraline alone. Behav Res Ther. 2003;41(11):1271–6.
Katzman MA, Bleau P, Blier P, Chokka P, Kjernisted K, Van Ameringen M, et al. Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders. BMC Psychiatry. 2014;14(Suppl 1):S1.
American Psychological Association. Clinical practice guideline for the treatment of posttraumatic stress disorder in adults. 2017. Available from: http://www.apa.org/about/offices/directorates/guidelines/clinical-practice.aspx.
Jonas DE, Cusack K, Forneris CA, Wilkins TM, Sonis J, Middleton JC, et al. AHRQ comparative effectiveness reviews: psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD). Rockville (MD): Agency for Healthcare Research and Quality (US); 2013.
Stein MB, Kline NA, Matloff JL. Adjunctive olanzapine for SSRI-resistant combat-related PTSD: a double-blind, placebo-controlled study. Am J Psychiatry. 2002;159(10):1777–9.
Ahearn EP, Mussey M, Johnson C, Krohn A, Krahn D. Quetiapine as an adjunctive treatment for post-traumatic stress disorder: an 8-week open-label study. Int Clin Psychopharmacol. 2006;21(1):29–33.
Hamner MB, Deitsch SE, Brodrick PS, Ulmer HG, Lorberbaum JP. Quetiapine treatment in patients with posttraumatic stress disorder: an open trial of adjunctive therapy. J Clin Psychopharmacol. 2003;23(1):15–20.
Naylor JC, Kilts JD, Bradford DW, Strauss JL, Capehart BP, Szabo ST, et al. A pilot randomized placebo-controlled trial of adjunctive aripiprazole for chronic PTSD in US military Veterans resistant to antidepressant treatment. Int Clin Psychopharmacol. 2015;30(3):167–74.
Spielmans GI, Berman MI, Linardatos E, Rosenlicht NZ, Perry A, Tsai AC. Adjunctive atypical antipsychotic treatment for major depressive disorder: a meta-analysis of depression, quality of life, and safety outcomes. PLoS Med. 2013;10(3):e1001403.
Monnelly EP, Ciraulo DA, Knapp C, Keane T. Low-dose risperidone as adjunctive therapy for irritable aggression in posttraumatic stress disorder. J Clin Psychopharmacol. 2003;23(2):193–6.
Krystal JH, Pietrzak RH, Rosenheck RA, Cramer JA, Vessicchio J, Jones KM, et al. Sleep disturbance in chronic military-related PTSD: clinical impact and response to adjunctive risperidone in the Veterans Affairs cooperative study #504. J clin psychiatry. 2016;77(4):483–91. A valuable discussion on sleep disturbance in PTSD
Raskind MA, Peskind ER, Kanter ED, Petrie EC, Radant A, Thompson CE, et al. Reduction of nightmares and other PTSD symptoms in combat veterans by prazosin: a placebo-controlled study. Am J Psychiatry. 2003;160(2):371–3.
Taylor FB, Martin P, Thompson C, Williams J, Mellman TA, Gross C, et al. Prazosin effects on objective sleep measures and clinical symptoms in civilian trauma posttraumatic stress disorder: a placebo-controlled study. Biol Psychiatry. 2008;63(6):629–32.
Raskind MA, Peskind ER, Hoff DJ, Hart KL, Holmes HA, Warren D, et al. A parallel group placebo controlled study of prazosin for trauma nightmares and sleep disturbance in combat veterans with post-traumatic stress disorder. Biol Psychiatry. 2007;61(8):928–34.
Raskind MA, Peterson K, Williams T, Hoff DJ, Hart K, Holmes H, et al. A trial of prazosin for combat trauma PTSD with nightmares in active-duty soldiers returned from Iraq and Afghanistan. Am J Psychiatry. 2013;170(9):1003–10.
Taylor FB, Lowe K, Thompson C, McFall MM, Peskind ER, Kanter ED, et al. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59(7):577–81.
Stafstrom CE. Mechanisms of action of antiepileptic drugs: the search for synergy. Curr Opin Neurol. 2010;23(2):157–63.
Akuchekian S, Amanat S. The comparison of topiramate and placebo in the treatment of posttraumatic stress disorder: a randomized, double-blind study. J Res Med Sci. 2004;9(5):240–4.
Lindley SE, Carlson EB, Hill KA. Randomized, double-blind, placebo-controlled trial of augmentation topiramate for chronic combat-related posttraumatic stress disorder. J Clin Psychopharmacol. 2007;27(6):677–81.
Sofuoglu M, Rosenheck R, Petrakis I. Pharmacological treatment of comorbid PTSD and substance use disorder: recent progress. Addict Behav. 2014;39(2):428–33.
Schneier FR, Campeas R, Carcamo J, Glass A, Lewis-Fernandez R, Neria Y, et al. Combined mirtazapine and SSRI treatment of PTSD: a placebo-controlled trial. Depress Anxiety. 2015;32(8):570–9.
Hertzberg MA, Feldman ME, Beckham JC, Davidson JR. Trial of trazodone for posttraumatic stress disorder using a multiple baseline group design. J Clin Psychopharmacol. 1996;16(4):294–8.
Warner MD, Dorn MR, Peabody CA. Survey on the usefulness of trazodone in patients with PTSD with insomnia or nightmares. Pharmacopsychiatry. 2001;34(4):128–31.
Walderhaug E, Kasserman S, Aikins D, Vojvoda D, Nishimura C, Neumeister A. Effects of duloxetine in treatment-refractory men with posttraumatic stress disorder. Pharmacopsychiatry. 2010;43(2):45–9.
Villarreal G, Hamner MB, Canive JM, Robert S, Calais LA, Durklaski V, et al. Efficacy of quetiapine monotherapy in posttraumatic stress disorder: a randomized, placebo-controlled trial. Am J Psychiatry. 2016;173(12):1205–12.
Friedman MJ. Pharmacotherapy. In: Benedek DM, GHW, editors. Clinical manual for management of PTSD. Washington, DC: American Psychiatric Publishing, Inc.; 2011. p. 131–82.
Yeh MS, Mari JJ, Costa MC, Andreoli SB, Bressan RA, Mello MF. A double-blind randomized controlled trial to study the efficacy of topiramate in a civilian sample of PTSD. CNS neurosci ther. 2011;17(5):305–10.
Tucker P, Trautman RP, Wyatt DB, Thompson J, SC W, Capece JA, et al. Efficacy and safety of topiramate monotherapy in civilian posttraumatic stress disorder: a randomized, double-blind, placebo-controlled study. J clin psychiatry. 2007;68(2):201–6.
Hertzberg MA, Butterfield MI, Feldman ME, Beckham JC, Sutherland SM, Connor KM, et al. A preliminary study of lamotrigine for the treatment of posttraumatic stress disorder. Biol Psychiatry. 1999;45(9):1226–9.
Kinrys G, Wygant LE, Pardo TB, Melo M. Levetiracetam for treatment-refractory posttraumatic stress disorder. J clin psychiatry. 2006;67(2):211–4.
Hamner M, Ulmer H, Horne D. Buspirone potentiation of antidepressants in the treatment of PTSD. Depression and Anxiety. 1997;5(3):137–9.
Neylan TC, Lenoci M, Samuelson KW, Metzler TJ, Henn-Haase C, Hierholzer RW, et al. No improvement of posttraumatic stress disorder symptoms with guanfacine treatment. Am J Psychiatry. 2006;163(12):2186–8.
Gupta MA, Knapp K. Lithium carbonate decreases acute suicidality in posttraumatic stress disorder. Aust N Z j psychiatry. 2013;47(12):1217.
Pradhan B, Kluewer D'Amico J, Makani R, Parikh T. Nonconventional interventions for chronic post-traumatic stress disorder: ketamine, repetitive trans-cranial magnetic stimulation (rTMS), and alternative approaches. J trauma dissociation : off j Int Soc Study of Dissociation (ISSD). 2016;17(1):35–54.
Wynn GH. Complementary and alternative medicine approaches in the treatment of PTSD. Curr psychiatry rep. 2015;17(8):600.
McLay RN, Loeffler GN, Wynn GH. Research methodology for the study of complementary and alternative medicine in the treatment of military PTSD. Psychiatr Ann. 2013;43(1):38–43.
Price M, Spinazzola J, Musicaro R, Turner J, Suvak M, Emerson D, et al. Effectiveness of an extended yoga treatment for women with chronic posttraumatic stress disorder. J altern complement med (New York, NY). 2017;23(4):300–9.
van der Kolk BA, Stone L, West J, Rhodes A, Emerson D, Suvak M, et al. Yoga as an adjunctive treatment for posttraumatic stress disorder: a randomized controlled trial. J clin psychiatry. 2014;75(6):e559–65.
Rhodes A, Spinazzola J, van der Kolk B. Yoga for adult women with chronic PTSD: a long-term follow-up study. J altern complement med (New York, NY). 2016;22(3):189–96.
Pradhan B, Gray R, Parikh T, Akkireddi P, Pumariega A. Trauma interventions using mindfulness based extinction and reconsolidation (TIMBER©) as monotherapy for chronic PTSD: a pilot study. Adolesc Psychiatry. 2015;5(2):125–31.
Engel CC, Cordova EH, Benedek DM, Liu X, Gore KL, Goertz C, et al. Randomized effectiveness trial of a brief course of acupuncture for posttraumatic stress disorder. Med Care. 2014;52(12 Suppl 5):S57–64.
Kim Y-D, Heo I, Shin B-C, Crawford C, Kang H-W, Lim J-H. Acupuncture for posttraumatic stress disorder: a systematic review of randomized controlled trials and prospective clinical trials. Evid Based Complement Alternat Med. 2013;2013:12.
Lee EE, Della Selva MP, Liu A, Himelhoch S. Ketamine as a novel treatment for major depressive disorder and bipolar depression: a systematic review and quantitative meta-analysis. Gen Hosp Psychiatry. 2015;37(2):178–84.
Feder A, Parides MK, Murrough JW, Perez AM, Morgan JE, Saxena S, et al. Efficacy of intravenous ketamine for treatment of chronic posttraumatic stress disorder: a randomized clinical trial. JAMA Psychiatry. 2014;71(6):681–8.
Zohar J, Yahalom H, Kozlovsky N, Cwikel-Hamzany S, Matar MA, Kaplan Z, et al. High dose hydrocortisone immediately after trauma may alter the trajectory of PTSD: interplay between clinical and animal studies. Eur neuropsychopharmacol : j Eur College of Neuropsychopharmacol. 2011;21(11):796–809.
Drexler SM, Wolf OT. The role of glucocorticoids in emotional memory reconsolidation. Neurobiol Learn Mem. 2017;142(Pt A):126–34.
Delahanty DL, Gabert-Quillen C, Ostrowski SA, Nugent NR, Fischer B, Morris A, et al. The efficacy of initial hydrocortisone administration at preventing posttraumatic distress in adult trauma patients: a randomized trial. CNS Spectr. 2013;18(2):103–11.
Suris A, North C, Adinoff B, Powell CM, Greene R. Effects of exogenous glucocorticoid on combat-related PTSD symptoms. Ann clin psychiatry : off j Am Acad Clin Psychiatrists. 2010;22(4):274–9.
Yehuda R, Bierer LM, Pratchett LC, Lehrner A, Koch EC, Van Manen JA, et al. Cortisol augmentation of a psychological treatment for warfighters with posttraumatic stress disorder: randomized trial showing improved treatment retention and outcome. Psychoneuroendocrinology. 2015;51:589–97.
• Mataix-Cols D, Fernandez de la Cruz L, Monzani B, Rosenfield D, Andersson E, Perez-Vigil A, et al. D-cycloserine augmentation of exposure-based cognitive behavior therapy for anxiety, obsessive-compulsive, and posttraumatic stress disorders: a systematic review and meta-analysis of individual participant data. JAMA Psychiatry. 2017;74(5):501–10. In depth evaluation of d-cycloserine as a potential adjunctive treatment.
• McGuire JF, Wu MS, Piacentini J, McCracken JT, Storch EA. A meta-analysis of d-cycloserine in exposure-based treatment: moderators of treatment efficacy, response, and diagnostic remission. J clin psychiatry. 2017;78(2):196–206. A further consideration of d-cycloserine.
Ori R, Amos T, Bergman H, Soares-Weiser K, Ipser JC, Stein DJ. Augmentation of cognitive and behavioural therapies (CBT) with d-cycloserine for anxiety and related disorders. Cochrane Database Syst Rev 2015(5):CD007803. https://doi.org/10.1002/14651858.CD007803.pub2.
• Mithoefer MC, Wagner MT, Mithoefer AT, Jerome L, Martin SF, Yazar-Klosinski B, et al. Durability of improvement in post-traumatic stress disorder symptoms and absence of harmful effects or drug dependency after 3,4-methylenedioxymethamphetamine-assisted psychotherapy: a prospective long-term follow-up study. J Psychopharmacol. 2013;27(1):28–39. Describes one of the major trials carried out on MDMA-assisted psychotherapy.
Mithoefer MC, Wagner MT, Mithoefer AT, Jerome L, Doblin R. The safety and efficacy of {+/−}3,4-methylenedioxymethamphetamine-assisted psychotherapy in subjects with chronic, treatment-resistant posttraumatic stress disorder: the first randomized controlled pilot study. J Psychopharmacol. 2011;25(4):439–52.
Carhart-Harris RL, Murphy K, Leech R, Erritzoe D, Wall MB, Ferguson B, et al. The effects of acutely administered 3,4-methylenedioxymethamphetamine on spontaneous brain function in healthy volunteers measured with arterial spin labeling and blood oxygen level-dependent resting state functional connectivity. Biol Psychiatry. 2015;78(8):554–62.
Sessa B, Nutt D. Making a medicine out of MDMA. Br J Psychiatry. 2015;206(1):4–6.
Amoroso T, Workman M. Treating posttraumatic stress disorder with MDMA-assisted psychotherapy: a preliminary meta-analysis and comparison to prolonged exposure therapy. J Psychopharmacol. 2016;30(7):595–600. A meta-analysis of studies using MDMA in PTSD
Passie T, Emrich HM, Karst M, Brandt SD, Halpern JH. Mitigation of post-traumatic stress symptoms by Cannabis resin: a review of the clinical and neurobiological evidence. Drug test anal. 2012;4(7–8):649–59.
Wilkinson ST, Radhakrishnan R, D'Souza DCA. Systematic review of the evidence for medical marijuana in psychiatric indications. J clin psychiatry. 2016;77(8):1050–64.
Jetly R, Heber A, Fraser G, Boisvert D. The efficacy of nabilone, a synthetic cannabinoid, in the treatment of PTSD-associated nightmares: a preliminary randomized, double-blind, placebo-controlled cross-over design study. Psychoneuroendocrinology. 2015;51:585–8.
• Wilkinson ST, Stefanovics E, Rosenheck RA. Marijuana use is associated with worse outcomes in symptom severity and violent behavior in patients with posttraumatic stress disorder. J clin psychiatry. 2015;76(9):1174–80. Discusses reasons to be cautious with the use of marijuana in PTSD.
O'Reardon JP, Solvason HB, Janicak PG, Sampson S, Isenberg KE, Nahas Z, et al. Efficacy and safety of transcranial magnetic stimulation in the acute treatment of major depression: a multisite randomized controlled trial. Biol Psychiatry. 2007;62(11):1208–16.
Boggio PS, Rocha M, Oliveira MO, Fecteau S, Cohen RB, Campanhã C, et al. Noninvasive brain stimulation with high-frequency and low-intensity repetitive transcranial magnetic stimulation treatment for posttraumatic stress disorder. J clin psychiatry. 2010;71(8):992–9.
Cohen H, Kaplan Z, Kotler M, Kouperman I, Moisa R, Grisaru N. Repetitive transcranial magnetic stimulation of the right dorsolateral prefrontal cortex in posttraumatic stress disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2004;161(3):515–24.
Watts BV, Landon B, Groft A, Young-Xu YA. Sham controlled study of repetitive transcranial magnetic stimulation for posttraumatic stress disorder. Brain stimul. 2012;5(1):38–43.
Langevin JP, Koek RJ, Schwartz HN, Chen JW, Sultzer DL, Mandelkern MA, et al. Deep brain stimulation of the basolateral amygdala for treatment-refractory posttraumatic stress disorder. Biol Psychiatry. 2016;79(10):e82–4.
George MS, Ward HE Jr, Ninan PT, Pollack M, Nahas Z, Anderson B, et al. A pilot study of vagus nerve stimulation (VNS) for treatment-resistant anxiety disorders. Brain Stimul: Basic Trans Clin Res Neuromodulation. 2008;1(2):112–21.
Kellner CH, Knapp R, Husain MM, Rasmussen K, Sampson S, Cullum M, et al. Bifrontal, bitemporal and right unilateral electrode placement in ECT. Br J Psychiatry. 2010;196(3):226–34.
Fosse R, Read J. Electroconvulsive treatment: hypotheses about mechanisms of action. Front Psychiatry 2013;4:1-10. https://doi.org/10.3389/fpsyt.2013.00094.
Baghai TC, Möller HJ. Electroconvulsive therapy and its different indications. Dialogues Clin Neurosci. 2008;10(1):105–17.
Margoob MA, Ali Z, Andrade C. Efficacy of ECT in chronic, severe, antidepressant- and CBT-refractory PTSD: an open, prospective study. Brain stimulation. 2010;3(1):28–35.
Youssef NA, McCall WV, Andrade C. The role of ECT in posttraumatic stress disorder: a systematic review. Ann clin psychiatry : off j Am Acad Clin Psychiatrists. 2017;29(1):62–70.
Bernardy NC, Friedman MJ. Psychopharmacological strategies in the management of posttraumatic stress disorder (PTSD): what have we learned? Curr psychiatry rep. 2015;17(4):20.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
In the past 3 years, Dr. Stein has received research grants and/or consultancy honoraria from Biocodex, Lundbeck, Servier, and Sun. Dr. Starke declares no conflict of interest.
Human and Animal Rights and Informed Consent
With regard to the authors’ research cited in this paper, all procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. In addition, all applicable international, national, and/or institutional guidelines for the care and use of animals were followed.
Additional information
This article is part of the Topical Collection on Anxiety, Obsessive Compulsive, and Related Disorders
Rights and permissions
About this article
Cite this article
Starke, J.A., Stein, D.J. Management of Treatment-Resistant Posttraumatic Stress Disorder. Curr Treat Options Psych 4, 387–403 (2017). https://doi.org/10.1007/s40501-017-0130-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40501-017-0130-0