Abstract
Background
Few clinical studies have assessed the efficacy and safety of oxcarbazepine (OXC) oral suspension in Asian pediatric patients and particularly in infants. The aim of this study was to investigate and compare the efficacy, tolerability, and side effects of OXC oral suspension in Taiwanese infants and children with various types of epilepsy.
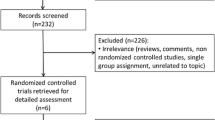
Methods
A retrospective review of the efficacy, tolerability, and side effects of OXC oral suspension in a tertiary medical center in Taiwan was conducted and included children (1–9 years old) and infants (<1 year old) diagnosed with epilepsy, which was classified into idiopathic partial, symptomatic partial, or multifocal subtypes. The OXC oral suspension (Trileptal®; Novartis) was given in a gradual dose titration, from an initial 7.5 mg/kg/day to 30 mg/kg/day within 1 month in all cases.
Results
A total of 20 infants and 38 children were identified. There were no statistically significant differences between the children and infants in efficacy (75 vs. 82 %, p = 0.734) and adverse effects (30 vs. 21 %, p = 0.525) after OXC oral suspension treatment. The efficacy was significantly correlated with the epilepsy subtype (p < 0.01) and the number of combined antiepileptic drugs (AEDs) before OXC treatment (p < 0.01) in both groups. The patients with idiopathic and symptomatic partial epilepsy responded better to OXC oral suspension than those with multifocal epilepsy.
Conclusions
OXC oral suspension is effective and well tolerated in both infants and children with partial epilepsy in Taiwan. Treatment efficacy was related to epilepsy subtype and number of combined AEDs before OXC treatment. Monotherapy had an excellent therapeutic response in partial epilepsy but not in multifocal epilepsy.

Similar content being viewed by others
References
Lopez Pison J, Fernandez Espuelas C, Saenz Moreno I, et al. Immediate switching from carbamazepine to oxcarbazepine. Our experience in children and adolescents. Neurologia. 2008;23:139–44.
Bang L, Goa K. Oxcarbazepine: a review of its use in children with epilepsy. Pediatr Drugs. 2003;5:557–73.
Pariente-Khayat A, Tran A, Vauzelle-Kervuroedan F, et al. Pharmacokinetics of oxcarbazepine as add-on therapy in epileptic children. Epilepsia. 1994;35:119.
Sallas WM, Milosavljev S, D’Souza J, et al. Pharmacokinetic drug interactions in children taking oxcarbazepine. Clin Pharmacol Ther. 2003;74:138–49.
Flesch G, Tudor D, Denouel J, Bonner J, Camisasca R. Assessment of the bioequivalence of two oxcarbazepine oral suspensions versus a film-coated tablet in healthy subjects. Int J Clin Pharmacol Ther. 2003;41:299–308.
Pina-Garza JE, Espinoza R, Nordli D, et al. Oxcarbazepine adjunctive therapy in infants and young children with partial seizures. Neurology. 2005;65:1370–5.
Rufo-Campos M, Casas-Fernandez C, Martinez-Bermejo A, et al. Long-term use of oxcarbazepine oral suspension in childhood epilepsy: open-label study. J Child Neurol. 2006;21:480–5.
Engel J. ILAE classification of epilepsy syndromes. Epilepsy Res. 2006;70:5–10.
Serdaroglu G, Kurul S, Tutuncuoglu S, Dirik E, Sarioglu B. Oxcarbazepine in the treatment of childhood epilepsy. Pediatr Neurol. 2003;28:37–41.
Kothare SV, Mostofi N, Khurana DS, et al. Oxcarbazepine therapy in very young children: a single-center clinical experience. Pediatr Neurol. 2006;35:173–6.
Kothare SV, Khurana DS, Mostofi N, et al. Oxcarbazepine monotherapy in children and adolescents: a single-center clinical experience. Pediatr Neurol. 2006;35:235–9.
Ortenzi A, Paggi A, Foschi N, Sabbatini D, Pistoli E, Ortenzi A, et al. Oxcarbazepine and adverse events: impact of age, dosage, metabolite serum concentrations and concomitant antiepileptic therapy. Funct Neurol. 2008;23:97–100.
Chaudhry MM, Abrar M, Mutahir K, et al. Oxcarbazepine-induced hemolytic anemia in a geriatric patient. Am J Ther. 2008;15:187–9.
Calamaras MR, Stowe ZN, Newport DJ, et al. Pancytopenia associated with the introduction of oxcarbazepine. J Clin Psychopharmacol. 2007;27:217–8.
Holtmann M, Krause M, Opp J, et al. Oxcarbazepine-induced hyponatremia and the regulation of serum sodium after replacing carbamazepine with oxcarbazepine in children. Neuropediatrics. 2002;33:298–300.
Pellock JM. Tricyclic anticonvulsants: safety and adverse effects. Epilepsy Behav. 2002;3:S14–7.
Oxcarbazepine: hyponatremia and skin reactions. Prescrire Int. 2007;16:18.
Chung W-H, Hung S-I, Hong H-S, et al. Medical genetics: a marker for Stevens–Johnson syndrome. Nature. 2004;428:486.
Gaily E, Granstrom ML, Liukkonen E. Oxcarbazepine in the treatment of early childhood epilepsy. J Child Neurol. 1997;12:496–8.
Glauser TA, Nigro M, Sachdeo R, et al. Adjunctive therapy with oxcarbazepine in children with partial seizures. The Oxcarbazepine Pediatric Study Group. Neurology. 2000;54:2237–44.
Franzoni E, Garone C, Sarajlija J, et al. Open prospective study on oxcarbazepine in epilepsy in children: a preliminary report. Seizure. 2006;15:292–8.
Acknowledgments
Shu-Hao Wei has no conflicts of interest that are directly relevant to this study. Cheng-Chao Liu has no conflicts of interest that are directly relevant to this study. Pi-Chuan Fan has no conflicts of interest that are directly relevant to this study. No sources of funding were received for the conduct of the study or publication of the results.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wei, SH., Liu, CC. & Fan, PC. A Comparison of the Efficacy and Tolerability of Oxcarbazepine Oral Suspension Between Infants and Children with Epilepsy: A Retrospective Chart Review at a Single Medical Center in Taiwan. Pediatr Drugs 16, 83–89 (2014). https://doi.org/10.1007/s40272-013-0049-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-013-0049-x