Abstract
Introduction
Systemic inflammatory response syndrome (SIRS) is one of the most serious complications in patients undergoing percutaneous nephrolithotomy (PCNL). Although glucocorticoids are increasingly used during PCNL, few studies have been concerned about the association between glucocorticoids and postoperative SIRS. The study aims to explore whether preoperative use of glucocorticoids is associated with SIRS after PCNL.
Methods
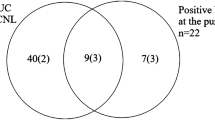
A total of 1259 patients who underwent PCNL between January 2015 and April 2021 were enrolled in the retrospective cohort study. Risk factors for post-PCNL SIRS were identified by univariate and multivariate regression analysis. To further explore the association between preoperative administration of glucocorticoids and SIRS, 113 pairs of patients were matched for the confounding factors using propensity score matching (PSM) analysis. The odds ratios (OR) and 95 % confidence intervals (CI) for the above variables were analyzed.
Results
The incidence of SIRS after PCNL was 9.6 % (121/1259) and the patients who suffered from postoperative SIRS had longer hospital stays and higher hospital costs (all p < 0.05). Multivariate logistic regression analysis indicated that female, preoperative leukocyte count, insertion of central vein catheter, serum albumin, preoperative high-sensitive C-reactive protein/albumin ratio, preoperative transfusion, preoperative administration of glucocorticoids were independent risk factors for SIRS (all p < 0.05). After minimization, the effects of confounding factors by PSM, preoperative administration of glucocorticoids was significantly correlated with SIRS in patients after PCNL (OR=2.44, 95 %CI: 1.31–4.55, p = 0.005).
Conclusion
Preoperative administration of glucocorticoids is an independent risk factor for SIRS in patients undergoing PCNL.
Plain Language Summary
Systemic inflammatory response syndrome (SIRS) is a frequent and severe complication in patients underwent percutaneous nephrolithotomy (PCNL), which can be challenging to diagnose early, potentially leading to delayed treatment. Identifying SIRS risk factors and promptly treating high-risk patients is crucial. Glucocorticoids are commonly used to prevent SIRS in clinical practice, and this study aims to investigate whether preoperative glucocorticoid administration is associated with SIRS after PCNL. In total, 1259 patients underwent PCNL and were enrolled in the study. The study utilized both propensity score matching (PSM) analysis and regression analysis to identify risk factors for post-PCNL SIRS. The incidence of SIRS after PCNL was 9.6 % in the study and patients with postoperative SIRS had longer hospital stays and higher hospital costs. After minimizing the potential influence of confounding factors through the use of PSM, we found a significant association between the preoperative use of glucocorticoids and the occurrence of SIRS in patients undergoing PCNL. Based on our analysis, we can conclude that the preoperative administration of glucocorticoids represents an independent risk factor for the development of SIRS in these patients.

Similar content being viewed by others
References
Khan SR, Pearle MS, Robertson WG, et al. Kidney stones. Nat Rev Dis Primers. 2016;2:16008.
Siener R. Nutrition and kidney stone disease. Nutrients. 2021. https://doi.org/10.3390/nu13061917.
Zeng G, Cai C, Duan X, et al. Mini percutaneous nephrolithotomy is a noninferior modality to standard percutaneous nephrolithotomy for the management of 20–40 mm renal calculi: a multicenter randomized controlled trial. Eur Urol. 2021;79(1):114–21. https://doi.org/10.1016/j.eururo.2020.09.026.
Wollin DA, Preminger GM. Percutaneous nephrolithotomy: complications and how to deal with them. Urolithiasis. 2018;46(1):87–97. https://doi.org/10.1007/s00240-017-1022-x.
Tang Y, Zhang C, Mo C, et al. Predictive model for systemic infection after percutaneous nephrolithotomy and related factors analysis. Front Surg. 2021;8: 696463. https://doi.org/10.3389/fsurg.2021.696463.
Singh P, Yadav S, Singh A, et al. Systemic inflammatory response syndrome following percutaneous nephrolithotomy: assessment of risk factors and their impact on patient outcomes. Urol Int. 2016;96(2):207–11. https://doi.org/10.1159/000441954.
Akkas F, Karadag S, Haciislamoglu A. Does the duration between urine culture and percutaneous nephrolithotomy affect the rate of systemic inflammatory response syndrome postoperatively? Urolithiasis. 2021;49(5):451–6. https://doi.org/10.1007/s00240-021-01245-7.
Deng Y, Tan F, Gan X, et al. Perioperative application of dexmedetomidine for postoperative systemic inflammatory response syndrome in patients undergoing percutaneous nephrolithotomy lithotripsy: results of a randomised controlled trial. BMJ Open. 2018;8(11): e019008. https://doi.org/10.1136/bmjopen-2017-019008.
Balk RA. Systemic inflammatory response syndrome (SIRS): where did it come from and is it still relevant today? Virulence. 2014;5(1):20–6. https://doi.org/10.4161/viru.27135.
Rello J, Valenzuela-Sánchez F, Ruiz-Rodriguez M, Moyano S. Sepsis: a review of advances in management. Adv Ther. 2017;34(11):2393–411. https://doi.org/10.1007/s12325-017-0622-8.
Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–247. https://doi.org/10.1097/CCM.0000000000005337.
De Oliveira Jr GS, Castro-Alves LJ, Ahmad S, Kendall MC, McCarthy RJ. Dexamethasone to prevent postoperative nausea and vomiting: an updated meta-analysis of randomized controlled trials. Anesth Analg. 2013;116(1):58–74. https://doi.org/10.1213/ANE.0b013e31826f0a0a.
Qi T, Qi X, Chen X, Jin X. The retrospective study of perioperative application of dexamethasone and furosemide for postoperative anti-inflammation in patients undergoing percutaneous nephrolithotomy. Int Urol Nephrol. 2021;53(4):669–77. https://doi.org/10.1007/s11255-020-02718-1.
Chen C, Yang D, Gao S, et al. Development and performance assessment of novel machine learning models to predict pneumonia after liver transplantation. Respir Res. 2021;22(1):94. https://doi.org/10.1186/s12931-021-01690-3.
Chan JY, Wong VK, Wong J, et al. Predictors of urosepsis in struvite stone patients after percutaneous nephrolithotomy. Investig Clin Urol. 2021;62(2):201–9. https://doi.org/10.4111/icu.20200319.
Serafim R, Gomes JA, Salluh J, Póvoa P. A comparison of the quick-SOFA and systemic inflammatory response syndrome criteria for the diagnosis of sepsis and prediction of mortality: a systematic review and meta-analysis. Chest. 2018;153(3):646–55. https://doi.org/10.1016/j.chest.2017.12.015.
Zakharova VV, Pletjushkina OY, Zinovkin RA, Popova EN, Chernyak BV. Mitochondria-targeted antioxidants and uncouplers of oxidative phosphorylation in treatment of the systemic inflammatory response syndrome (SIRS). J Cell Physiol. 2017;232(5):904–12. https://doi.org/10.1002/jcp.25626.
Whitlock RP, Devereaux PJ, Teoh KH, et al. Methylprednisolone in patients undergoing cardiopulmonary bypass (SIRS): a randomised, double-blind, placebo-controlled trial. Lancet. 2015;386(10000):1243–53. https://doi.org/10.1016/s0140-6736(15)00273-1.
Kallidonis P, Tsaturyan A, Lattarulo M, Liatsikos E. Minimally invasive percutaneous nephrolithotomy (PCNL): techniques and outcomes. Turk J Urol. 2020;46(Supp. 1):S58–63. https://doi.org/10.5152/tud.2020.20161.
Wang C, Xu R, Zhang Y, et al. Nomograms for predicting the risk of SIRS and urosepsis after uroscopic minimally invasive lithotripsy. Biomed Res Int. 2022;2022:6808239. https://doi.org/10.1155/2022/6808239.
Cain DW, Cidlowski JA. Immune regulation by glucocorticoids. Nat Rev Immunol. 2017;17(4):233–47. https://doi.org/10.1038/nri.2017.1.
Vandewalle J, Libert C. Glucocorticoids in sepsis: to be or not to be. Front Immunol. 2020;11:1318. https://doi.org/10.3389/fimmu.2020.01318.
Cicarelli DD, Benseñor FE, Vieira JE. Effects of single dose of dexamethasone on patients with systemic inflammatory response. Sao Paulo Med J. 2006;124(2):90–5. https://doi.org/10.1590/s1516-31802006000200008.
Zhou J, Chen C, Cheng N, et al. Perioperative administration of methylprednisolone was associated with postoperative pulmonary complications in elderly patients undergoing hip fracture surgery. Aging Clin Exp Res. 2022;34(9):2005–12. https://doi.org/10.1007/s40520-022-02166-0.
Gan TJ, Diemunsch P, Habib AS, et al. Consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2014;118(1):85–113. https://doi.org/10.1213/ane.0000000000000002.
Lemieux SM, Levine AR. Low-dose corticosteroids in septic shock: has the pendulum shifted? Am J Health Syst Pharm. 2019;76(8):493–500. https://doi.org/10.1093/ajhp/zxz017.
Fang F, Zhang Y, Tang J, et al. Association of corticosteroid treatment with outcomes in adult patients with sepsis: a systematic review and meta-analysis. JAMA Intern Med. 2019;179(2):213–23. https://doi.org/10.1001/jamainternmed.2018.5849.
Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–38. https://doi.org/10.1038/nri.2016.90.
Reynés G, Vila V, Martín M, et al. Circulating markers of angiogenesis, inflammation, and coagulation in patients with glioblastoma. J Neurooncol. 2011;102(1):35–41. https://doi.org/10.1007/s11060-010-0290-x.
Xu H, Hu L, Wei X, et al. The predictive value of preoperative high-sensitive C-reactive protein/albumin ratio in systemic inflammatory response syndrome after percutaneous nephrolithotomy. J Endourol. 2019;33(1):1–8. https://doi.org/10.1089/end.2018.0632.
O’Grady NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Clin Infect Dis. 2011;52(9):e162–93.
Dunne JR, Malone DL, Tracy JK, Napolitano LM. Allogenic blood transfusion in the first 24 hours after trauma is associated with increased systemic inflammatory response syndrome (SIRS) and death. Surg Infect (Larchmt). 2004;5(4):395–404. https://doi.org/10.1089/sur.2004.5.395.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was supported partly by the National Natural Science Foundation of China (Grant No. 82102297), Natural Science Foundation of Guangdong Province (Grant No. 2022A1515012603), Young Talent Support Project of Guangzhou Association for Science and Technology (Grant No. QT20220101257), the “Five and five” Project of the Third Affiliated Hospital of Sun Yat-Sen University (grant No. 2023WW501) and Science and Technology Planning Project of Guangdong Province-Regional Innovation Capacity and Support System Construction (grant No. 2023B110006).
Conflict of interest
Not applicable.
Ethics approval
This study was conducted in accordance with the Declaration of Helsinki and the protocol and it was approved by the Ethics Committee of our hospital on 14 May 2019 (No. [2019]02–609-02). The requirement for informed consent and clinical trial registration were waived by the committee.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
The data and material are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
JPH: data collection, data analysis and write-up of manuscript. CJC and XYL: data collection, data analysis and interpretation. JK: study design, data analysis, and interpretation. XYZ: data collection and critical review of manuscript. SLZ, HYM and CLG: study conception, study design, data analysis and interpretation and critical review of manuscript. All authors read and approved the final version of this manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Hu, J., Chen, C., Li, X. et al. Risk of Systemic Inflammatory Response Syndrome Following Preoperative Glucocorticoids Administration in Patients After Percutaneous Nephrolithotomy: A Retrospective Cohort Study. Drug Saf 47, 465–474 (2024). https://doi.org/10.1007/s40264-024-01402-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-024-01402-y