Abstract
Background
Bipolar disorder (BD) is a chronic relapsing-remitting psychiatric disorder. Sleep and circadian rhythm disturbances persist during acute mood episodes of the disorder and during euthymia. However, the treatment potential of hypnotic agents that might be used to manage sleep disturbance in BD is not well understood. Similarly, melatonin and medications with a melatonin-receptor agonist mechanism of action may have chronotherapeutic potential for treating people with the disorder, but the impact of these substances on sleep and circadian rhythms and core symptoms in BD is unclear.
Objective
Our aim was to conduct a systematic review and meta-analysis evaluating the current evidence for hypnotic and melatonin/melatonin-receptor agonist pharmacotherapy for symptoms of sleep disturbance, mania, and depression in patients with BD.
Methods
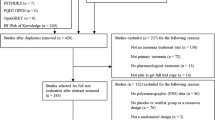
AMED, Embase, MEDLINE and PsychINFO databases were searched for studies published in English from the date of inception to 31 October 2021. Studies included in this review were randomised controlled trials (RCTs) and non-controlled/non-randomised studies for BD that examined hypnotic medications selected based on a common pattern of usage for treating insomnia (i.e. chloral, clomethiazole, diphenhydramine, doxepin, doxylamine, promethazine, suvorexant, zaleplon, zolpidem, zopiclone, and eszopiclone) and melatonin and the melatonin-receptor agonist drugs ramelteon and agomelatine. Risk of bias was assessed using the RoB2 and AXIS tools. Pooled effect sizes for RCT outcomes were estimated using random-effects models.
Results
A total of eleven studies (six RCTs and five experimental feasibility studies) involving 1279 participants were included. Each study examined melatonin or melatonin-receptor agonists. No studies of hypnotics were found that fulfilled the review inclusion criteria. Pilot feasibility studies suggested beneficial treatment effects for symptoms of sleep disturbance, depression, and mania. However, the pooled effect of the two available RCT studies assessing sleep quality via Pittsburgh Sleep Quality Index scores was not statistically significant (g = − 0.04 [95% CI − 0.81 to 0.73]) and neither was the pooled effect for depressive symptoms (four studies; g = − 0.10 [95% CI − 0.27 to 0.08]). Some RCT evidence suggests ramelteon might prevent relapse into depression in BD. The largest efficacy signal detected was for manic symptoms (four studies; g = − 0.44 [95% CI − 1.03 to 0.14]) but there was substantial heterogeneity between studies and patient characteristics. In the two RCTs assessing manic symptoms during acute mania, adjunctive melatonin demonstrated superior treatment effects versus placebo.
Conclusions
There is a paucity of studies examining pharmacological interventions for sleep and circadian rhythm disturbance in BD. Few studies assessed sleep-related symptoms, and none quantitatively examined endogenous melatonin patterns or other circadian rhythms. Melatonin may be a promising candidate for the adjunctive treatment of bipolar mania. However, dose-finding studies and studies with larger sample sizes are needed to confirm its efficacy. We recommend parallel monitoring of sleep and circadian rhythms in future trials. Chronobiology-informed trial designs are needed to improve the quality of future studies.
Protocol registration
PROSPERO (CRD42020167528).


Similar content being viewed by others
References
Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) and International Society for Bipolar Disorders (ISBD) 2018 guidelines for the management of patients with bipolar disorder. Bipolar Disord. 2018;20(2):97–170. https://doi.org/10.1111/bdi.12609.
Perlis RH, Ostacher MJ, Patel JK, Marangell LB, Zhang H, Wisniewski SR, Ketter TA, Miklowitz DJ, Otto MW, Gyulai L, Reilly-Harrington NA. Predictors of recurrence in bipolar disorder: primary outcomes from the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Am J Psychiatry. 2006;163(2):217–24.
Malhi GS, McAulay C, Das P, Fritz K. Maintaining mood stability in bipolar disorder: a clinical perspective on pharmacotherapy. Evid Based Ment Health. 2015;18(1):1–6.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington D.C.: American Psychiatric Association; 2013.
Harvey AG, Schmidt DA, Scarnà A, Semler CN, Goodwin GM. Sleep-related functioning in euthymic patients with bipolar disorder, patients with insomnia, and subjects without sleep problems. Am J Psychiatry. 2005;162(1):50–7. https://doi.org/10.1176/appi.ajp.162.1.50.
De Crescenzo F, Economou A, Sharpley AL, Gormez A, Quested DJ. Actigraphic features of bipolar disorder: a systematic review and meta-analysis. Sleep Med Rev. 2017;33:58–69. https://doi.org/10.1016/j.smrv.2016.05.003.
Ng TH, Chung KF, Ho FY, Yeung WF, Yung KP, Lam TH. Sleep-wake disturbance in interepisode bipolar disorder and high-risk individuals: a systematic review and meta-analysis. Sleep Med Rev. 2015;20:46–58. https://doi.org/10.1016/j.smrv.2014.06.006.
Jackson A, Cavanagh J, Scott J. A systematic review of manic and depressive prodromes. J Affect Disord. 2003;74(3):209–17.
Sylvia LG, Dupuy JM, Ostacher MJ, Cowperthwait CM, Hay AC, Sachs GS, Nierenberg AA, Perlis RH. Sleep disturbance in euthymic bipolar patients. J Psychopharmacol. 2012;26(8):1108–12.
Cretu JB, Culver JL, Goffin KC, Shah S, Ketter TA. Sleep, residual mood symptoms, and time to relapse in recovered patients with bipolar disorder. J Affect Disord. 2016;15(190):162–6.
Morton E, Murray G. Assessment and treatment of sleep problems in bipolar disorder—A guide for psychologists and clinically focused review. Clin Psychol Psychother. 2020;27(3):364–77.
Steinan MK, Scott J, Lagerberg TV, et al. Sleep problems in bipolar disorders: more than just insomnia. Acta Psychiatr Scand. 2016;133(5):368–77. https://doi.org/10.1111/acps.12523.
Harvey AG, Soehner AM, Kaplan KA, et al. Treating insomnia improves mood state, sleep, and functioning in bipolar disorder: a pilot randomized controlled trial. J Consult Clin Psychol. 2015;83(3):564–77. https://doi.org/10.1037/a0038655.
Gottlieb JF, Benedetti F, Geoffroy PA, Henriksen TE, Lam RW, Murray G, Phelps J, Sit D, Swartz HA, Crowe M, Etain B. The chronotherapeutic treatment of bipolar disorders: A systematic review and practice recommendations from the ISBD task force on chronotherapy and chronobiology. Bipolar Disord. 2019;21(8):741–73.
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, Espie CA, Garcia-Borreguero D, Gjerstad M, Gonçalves M, Hertenstein E. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700.
American College of Physicians. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165:125–33.
Wingård L, Taipale H, Reutfors J, Westerlund A, Bodén R, Tiihonen J, Tanskanen A, Andersen M. Initiation and long-term use of benzodiazepines and Z-drugs in bipolar disorder. Bipolar Disord. 2018;20(7):634–46.
Schaffer CB, Schaffer LC, Miller AR, Hang E, Nordahl TE. Efficacy and safety of nonbenzodiazepine hypnotics for chronic insomnia in patients with bipolar disorder. J Affect Disord. 2011;128(3):305–8.
Borbély AA, Daan S, Wirz-Justice A, Deboer T. The two-process model of sleep regulation: a reappraisal. J Sleep Res. 2016;25(2):131–43.
Dibner C, Schibler U, Albrecht U. The mammalian circadian timing system: organization and coordination of central and peripheral clocks. Annu Rev Physiol. 2010;17(72):517–49.
Roenneberg T, Merrow M. The circadian clock and human health. Curr Biol. 2016;26(10):R432–43.
Alloy LB, Ng TH, Titone MK, Boland EM. Circadian rhythm dysregulation in bipolar spectrum disorders. Curr Psychiatry Rep. 2017;19(4):21.
Takaesu Y. Circadian rhythm in bipolar disorder: a review of the literature. Psychiatry Clin Neurosci. 2018;72(9):673–82.
Melo MC, Abreu RL, Neto VB, de Bruin PF, de Bruin VM. Chronotype and circadian rhythm in bipolar disorder: a systematic review. Sleep Med Rev. 2017;1(34):46–58.
Moriya S, Tahara Y, Sasaki H, Ishigooka J, Shibata S. Phase-delay in the light–dark cycle impairs clock gene expression and levels of serotonin, norepinephrine, and their metabolites in the mouse hippocampus and amygdala. Sleep Med. 2015;16(11):1352–9.
Steinan MK, Morken G, Lagerberg TV, Melle I, Andreassen OA, Vaaler AE, Scott J. Delayed sleep phase: an important circadian subtype of sleep disturbance in bipolar disorders. J Affect Disord. 2016;1(191):156–63.
Moon JH, Cho CH, Son GH, Geum D, Chung S, Kim H, Kang SG, Park YM, Yoon HK, Kim L, Jee HJ. Advanced circadian phase in mania and delayed circadian phase in mixed mania and depression returned to normal after treatment of bipolar disorder. EBioMedicine. 2016;1(11):285–95.
Auger RR, Burgess HJ, Emens JS, Deriy LV, Thomas SM, Sharkey KM. Clinical practice guideline for the treatment of intrinsic circadian rhythm sleep-wake disorders: advanced sleep-wake phase disorder (ASWPD), delayed sleep-wake phase disorder (DSWPD), non-24-hour sleep-wake rhythm disorder (N24SWD), and irregular sleep-wake rhythm disorder (ISWRD). An update for 2015: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med. 2015;11(10):1199–236.
Richardson GS, Zee PC, Wang-Weigand S, Rodriguez L, Peng X. Circadian phase-shifting effects of repeated ramelteon administration in healthy adults. J Clin Sleep Med. 2008;4(5):456–61.
Robillard R, Carpenter JS, Feilds KL, Hermens DF, White D, Naismith SL, Bartlett D, Whitwell B, Southan J, Scott EM, Hickie IB. Parallel changes in mood and melatonin rhythm following an adjunctive multimodal chronobiological intervention with agomelatine in people with depression: a proof of concept open label study. Front Psych. 2018;11(9):624.
Bradley AJ, Webb-Mitchell R, Hazu A, Slater N, Middleton BA, Gallagher P, McAllister-Williams H, Anderson KN. Sleep and circadian rhythm disturbance in bipolar disorder. Psychol Med. 2017;47(9):1678–89.
Nurnberger JI, Adkins S, Lahiri DK, Mayeda A, Hu K, Lewy A, Miller A, Bowman ES, Miller MJ, Rau NL, Smiley C. Melatonin suppression by light in euthymic bipolar and unipolar patients. Arch Gen Psychiatry. 2000;57(6):572–9.
Geoffroy PA, Etain B, Franchi JA, Bellivier F, Ritter P. Melatonin and melatonin agonists as adjunctive treatments in bipolar disorders. Curr Pharm Des. 2015; 21(23):3352–8.
Kishi T, Nomura I, Sakuma K, Kitajima T, Mishima K, Iwata N. Melatonin receptor agonists-ramelteon and melatonin-for bipolar disorder: a systematic review and meta-analysis of double-blind, randomized, placebo-controlled trials. Neuropsychiatr Dis Treat. 2019;15:1479–86. https://doi.org/10.2147/NDT.S198899 (Published 2019 May 30).
Li J, Lu WQ, Beesley S, Loudon AS, Meng QJ. Lithium impacts on the amplitude and period of the molecular circadian clockwork. PLoS ONE. 2012;7(3):e33292.
Calabrese F, Savino E, Papp M, Molteni R, Riva MA. Chronic mild stress-induced alterations of clock gene expression in rat prefrontal cortex: modulatory effects of prolonged lurasidone treatment. Pharmacol Res. 2016;1(104):140–50.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Leibenluft E, Feldman-Naim S, Turner EH, Wehr TA, Rosenthal NE. Effects of exogenous melatonin administration and withdrawal in five patients with rapid-cycling bipolar disorder. J Clin Psychiatry. 1997;58(9):383–8.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, Cates CJ, Cheng H-Y, Corbett MS, Eldridge SM, Hernán MA, Hopewell S, Hróbjartsson A, Junqueira DR, Jüni P, Kirkham JJ, Lasserson T, Li T, McAleenan A, Reeves BC, Shepperd S, Shrier I, Stewart LA, Tilling K, White IR, Whiting PF, Higgins JPT. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:I4898.
Downes MJ, Brennan ML, Williams HC, Dean RS. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open. 2016;6(12):e011458.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. www.training.cochrane.org/handbook. Accessed October 2020
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177–88.
Lüdecke D. esc: cluster: Effect Size Computation for Meta Analysis. R package version 0.5.1. 2019
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60.
Harrer M, Cuijpers P, Furukawa T, Ebert DD. dmetar: Companion R Package For The Guide 'Doing Meta-Analysis in R'. R package version 0.0.9000. 2019
McGuinness LA. robvis: An R package and web application for visualising risk-of-bias Assessments. 2019 https://github.com/mcguinlu/robvis. Accessed October 2020
Moghaddam HS, Bahmani S, Bayanati S, Mahdavinasa M, Rezaei F, Akhondzadeh S. Efficacy of melatonin as an adjunct in the treatment of acute mania: a double-blind and placebo-controlled trial. Int Clin Psychopharmacol. 2020;35(2):81–8.
Quested DJ, Gibson JC, Sharpley AL, Cordey JH, Economou A, De Crescenzo F, Voysey M, Lawson J, Rendell JM, Al‐Taiar H, Lennox A. Melatonin In Acute Mania Investigation (MIAMI‐UK). A randomised controlled trial of add‐on melatonin in bipolar disorder. Bipolar Disorders. 2020. https://doi.org/10.1111/bdi.12944.
Bersani G, Garavini A. Melatonin add-on in manic patients with treatment resistant insomnia. Prog Neuropsychopharmacol Biol Psychiatry. 2000;24(2):185–91.
Calabrese JR, Guelfi JD, Perdrizet-Chevallier C, Agomelatine Bipolar Study Group. Agomelatine adjunctive therapy for acute bipolar depression: preliminary open data. Bipolar Disord. 2007;9(6):628–35.
Fornaro M, McCarthy MJ, De Berardis D, De Pasquale C, Tabaton M, Martino M, Colicchio S, Cattaneo CI, D’Angelo E, Fornaro P. Adjunctive agomelatine therapy in the treatment of acute bipolar II depression: a preliminary open label study. Neuropsychiatr Dis Treat. 2013;9:243.
Tyuvina NA, Smirnova VN. Comparative Assessment of the Efficacy of Valdoxane (agomelatine) in Recurrent Depression and Bipolar Affective Disorder. Neurosci Behav Physiol. 2014;44(2):187–94.
Mahableshwarkar AR, Calabrese JR, Macek TA, Budur K, Adefuye A, Dong X, Hanson E, Sachs GS. Efficacy and safety of sublingual ramelteon as an adjunctive therapy in the maintenance treatment of bipolar I disorder in adults: a phase 3, randomized controlled trial. J Affect Disord. 2017;15(221):275–82.
McElroy SL, Winstanley EL, Martens B, Patel NC, Mori N, Moeller D, McCoy J, Keck PE. A randomized, placebo-controlled study of adjunctive ramelteon in ambulatory bipolar I disorder with manic symptoms and sleep disturbance. Int Clin Psychopharmacol. 2011;26(1):48–53.
Norris ER, Burke K, Correll JR, Zemanek KJ, Lerman J, Primelo RA, Kaufmann MW. A double-blind, randomized, placebo-controlled trial of adjunctive Ramelteon for the treatment of insomnia and mood stability in patients with euthymic bipolar disorder. J Affect Disord. 2013;144(1–2):141–7.
Yatham LN, Vieta E, Goodwin GM, Bourin M, de Bodinat C, Laredo J, Calabrese J. Agomelatine or placebo as adjunctive therapy to a mood stabiliser in bipolar I depression: randomised double-blind placebo-controlled trial. Br J Psychiatry. 2016;208(1):78–86.
Ferracioli-Oda E, Qawasmi A, Bloch MH. Meta-analysis: melatonin for the treatment of primary sleep disorders. PLoS ONE. 2013;8(5):e63773.
Kuriyama A, Honda M, Hayashino Y. Ramelteon for the treatment of insomnia in adults: a systematic review and meta-analysis. Sleep Med. 2014;15(4):385–92.
Bauer M, Grof P, Rasgon N, Bschor T, Glenn T, Whybrow PC. Temporal relation between sleep and mood in patients with bipolar disorder. Bipolar Disord. 2006;8(2):160–7.
Hallam KT, Begg DP, Olver JS, Norman TR. Abnormal dose-response melatonin suppression by light in bipolar type I patients compared with healthy adult subjects. Acta Neuropsychiatrica. 2009;21(5):246–55.
Nathan PJ, Burrows GD, Norman TR. Melatonin sensitivity to dim white light in affective disorders. Neuropsychopharmacology. 1999;21(3):408–13.
Barbini B, Benedetti F, Colombo C, Dotoli D, Bernasconi A, Cigala-Fulgosi M, Florita M, Smeraldi E. Dark therapy for mania: a pilot study. Bipolar Disord. 2005;7(1):98–101.
Henriksen TE, Skrede S, Fasmer OB, Schoeyen H, Leskauskaite I, Bjørke-Bertheussen J, Assmus J, Hamre B, Grønli J, Lund A. Blue-blocking glasses as additive treatment for mania: a randomized placebo-controlled trial. Bipolar Disord. 2016;18(3):221–32.
Gitlin MJ. Antidepressants in bipolar depression: an enduring controversy. Int J Bipolar Disord. 2018;6(1):25.
Guardiola-Lemaitre B, De Bodinat C, Delagrange P, Millan MJ, Munoz C, Mocaër E. Agomelatine: mechanism of action and pharmacological profile in relation to antidepressant properties. Br J Pharmacol. 2014;171(15):3604–19.
Huedo-Medina TB, Kirsch I, Middlemass J, Klonizakis M, Siriwardena AN. Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: meta-analysis of data submitted to the Food and Drug Administration. BMJ. 2012;17:345.
Bobo WV, Reilly-Harrington NA, Ketter TA, Brody BD, Kinrys G, Kemp DE, Shelton RC, McElroy SL, Sylvia LG, Kocsis JH, McInnis MG. Complexity of illness and adjunctive benzodiazepine use in outpatients with bipolar I or II disorder: results from the Bipolar CHOICE study. J Clin Psychopharmacol. 2015;35(1):68.
Burgess HJ, Wyatt JK, Park M, Fogg LF. Home circadian phase assessments with measures of compliance yield accurate dim light melatonin onsets. Sleep. 2015;38(6):889–97.
van Geijlswijk IM, van der Heijden KB, Egberts AC, Korzilius HP, Smits MG. Dose finding of melatonin for chronic idiopathic childhood sleep onset insomnia: an RCT. Psychopharmacology. 2010;212(3):379–91.
Stefani LC, Muller S, Torres IL, Razzolini B, Rozisky JR, Fregni F, Markus R, Caumo W. A phase II, randomized, double-blind, placebo controlled, dose-response trial of the melatonin effect on the pain threshold of healthy subjects. PLoS ONE. 2013;8(10):e74107.
Slominski RM, Reiter RJ, Schlabritz-Loutsevitch N, Ostrom RS, Slominski AT. Melatonin membrane receptors in peripheral tissues: distribution and functions. Mol Cell Endocrinol. 2012;351(2):152–66.
Acknowledgements
We thank Professor Edward Norris and Professor Lakshmi Yatham for facilitating our requests for access to unreported data from the published Norris et al. and Yatham et al. studies. SDK and KEAS are supported by the NIHR Oxford Health Biomedical Research Centre. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work received no funding.
Author contributions
NMMcG, LB, and KEAS conceived the original idea for the review. NMMcG, DSK, LB, and KEAS designed the review protocol. NMMcG and DSK conducted the literature searches and together with MdAC performed the eligibility screen. Studies that met inclusion criteria were assessed for risk of bias by DSK and MdAC with assistance from NMMcG. Data extraction, quantitative analysis and interpretation was performed by NMMcG with the assistance of LB. NMMcG wrote the draft manuscript with the assistance of DSK. KEAS and SDK critically revised the manuscript and contributed substantially to the discussion of findings. All authors contributed to and approved the final manuscript and agree to be accountable for the work presented in the manuscript.
Conflicts of interest
NMMcG, DSK, MdAC, LB, SDK, and KEAS have no conflicts of interest to disclose.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McGowan, N.M., Kim, D.S., de Andres Crespo, M. et al. Hypnotic and Melatonin/Melatonin-Receptor Agonist Treatment in Bipolar Disorder: A Systematic Review and Meta-Analysis. CNS Drugs 36, 345–363 (2022). https://doi.org/10.1007/s40263-022-00911-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-022-00911-7



