Abstract
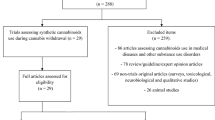
Novel pharmacological treatments are needed for Tourette syndrome. Our goal was to examine the current evidence base and biological rationale for the use of cannabis-derived medications or medications that act on the cannabinoid system in Tourette syndrome. We conducted a comprehensive literature search of PubMed for randomized controlled trials or clinical trials of cannabis-derived medications in Tourette syndrome. Data regarding the population, intervention, safety profile, and outcomes for each trial were extracted and reported and the evidence supporting use of individual cannabis-derived medications was critiqued. There is a strong biological rationale regarding how cannabis-derived medications could affect tic severity. Anecdotal case reports and series have noted that many patients report that their tics improve after using cannabis. However, only two small randomized, placebo-controlled trials of Δ9-tetrahydrocannabinol have been published; these suggested possible benefits of cannabis-derived agents for the treatment of tics. Trials examining other agents active on the cannabinoid system for tic disorders are currently ongoing. Cannabinoid-based treatments are a promising avenue of new research for medications that may help the Tourette syndrome population. However, given the limited research available, the overall efficacy and safety of cannabinoid-based treatments is largely unknown. Further trials are needed to examine dosing, active ingredients, and optimal mode of administration of cannabis-derived compounds, assuming initial trials suggest efficacy. Clinical use for refractory patients should at the very least be restricted to adult populations, given the uncertain efficacy and risk of developmental adverse effects that cannabinoids may have in children. Even in adult populations, cannabis-derived medications are associated with significant issues such as the effects they have on driving safety and the fact that they cause positive urine drug screens that can affect employment.

Similar content being viewed by others
References
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5®). Washington, DC: American Psychiatric Association; 2013.
Scahill L, Dalsgaard S, Bradbury K. The prevalence of Tourette syndrome and its relationship to clinical features. In: Martino D, Leckmand JF, editors. Tourette syndrome. New York: Oxford University Press; 2013. p. 121–33.
Cohen SC, Leckman JF, Bloch MH. Clinical assessment of Tourette syndrome and tic disorders. Neurosci Biobehav Rev. 2013;37(6):997–1007.
Peterson BS, Leckman JF. The temporal dynamics of tics in Gilles de la Tourette syndrome. Biol Psychiatry. 1998;44(12):1337–48.
Conelea CA, Woods DW. The influence of contextual factors on tic expression in Tourette’s syndrome: a review. J Psychosom Res. 2008;65(5):487–96.
Leckman JF, Bloch MH, Sukhodolsky DG, Scahill L, King RA. Phenomenology of tics and sensory urges: the self under siege. In: Martino D, Leckmand JF, editors. Tourette syndrome. New York: Oxford University Press; 2013. p. 3–25.
Leckman JF, Zhang H, Vitale A, Lahnin F, Lynch K, Bondi C, et al. Course of tic severity in Tourette syndrome: the first two decades. Pediatrics. 1998;102(1 Pt 1):14–9.
Freeman RD, Fast DK, Burd L, Kerbeshian J, Robertson MM, Sandor P. An international perspective on Tourette syndrome: selected findings from 3,500 individuals in 22 countries. Dev Med Child Neurol. 2000;42(7):436–47.
Khalifa N, von Knorring AL. Prevalence of tic disorders and Tourette syndrome in a Swedish school population. Dev Med Child Neurol. 2003;45(5):315–9.
Peterson BS, Pine DS, Cohen P, Brook JS. Prospective, longitudinal study of tic, obsessive-compulsive, and attention-deficit/hyperactivity disorders in an epidemiological sample. J Am Acad Child Adolesc Psychiatry. 2001;40(6):685–95.
Torup E. A follow-up study of children with tics. Acta Paediatr. 1962;51:261–8.
Bloch M, Peterson B, Scahill L, Otka J, Katsovich L, Leckman J. Clinical predictors of future tic and OCD severity in children with Tourette syndrome. Arch Pediatr Adolesc Med. 2006;160:65–9.
da Silva Prado H, do Rosário MC, Shavitt RG, Miguel EC. Sensory phenomena, ‘just right’, and ‘not just right’experiences in OD patients: looking for consensus. CNS Spect. 2007;12:95–6.
Rothenberger A, Roessner V. The phenomenology of attention-deficit/hyperactivity disorder in Tourette syndrome. In: Martino D, Leckmand JF, editors. Tourette syndrome. New York: Oxford University Press; 2013. p. 26–49.
Cavanna AE, Servo S, Monaco F, Robertson MM. The behavioral spectrum of Gilles de la Tourette syndrome. J Neuropsychiatry Clin Neurosci. 2009;21(1):13–23.
Gorman DA, Thompson N, Plessen KJ, Robertson MM, Leckman JF, Peterson BS. Psychosocial outcome and psychiatric comorbidity in older adolescents with Tourette syndrome: controlled study. Br J Psychiatry. 2010;197(1):36–44.
Eddy CM, Cavanna AE, Gulisano M, Agodi A, Barchitta M, Calì P, et al. Clinical correlates of quality of life in Tourette syndrome. Mov Disord. 2011;26(4):735–8.
Price RA, Kidd KK, Cohen DJ, Pauls DL, Leckman JF. A twin study of Tourette syndrome. Arch Gen Psychiatry. 1985;42(8):815–20.
Fernandez TV, State MW, Pittenger C. Chapter 23—Tourette disorder and other tic disorders. In: Geschwind DH, Paulson HL, Klein C, editors. Handbook of clinical neurology. Amsterdam: Elsevier; 2018. p. 343–54.
Fernandez TV, State MW, Pittenger C. Tourette disorder and other tic disorders. Handb Clin Neurol. 2018;147:343–54.
Ercan-Sencicek AG, Stillman AA, Ghosh AK, Bilguvar K, O’Roak BJ, Mason CE, et al. l-Histidine decarboxylase and Tourette’s syndrome. N Engl J Med. 2010;362(20):1901–8.
Shapiro AK, Shapiro E. Treatment of Gilles de la Tourette’s syndrome with haloperidol. Br J Psychiatry. 1968;114(508):345–50.
Bloch MH, Leckman JF, Zhu H, Peterson BS. Caudate volumes in childhood predict symptom severity in adults with Tourette syndrome. Neurology. 2005;65(8):1253–8.
Peterson BS, Thomas P, Kane MJ, Scahill L, Zhang H, Bronen R, et al. Basal ganglia volumes in patients with Gilles de la Tourette syndrome. Arch Gen Psychiatry. 2003;60(4):415–24.
Felling RJ, Singer HS. Neurobiology of Tourette syndrome: current status and need for further investigation. J Neurosci. 2011;31(35):12387–95.
Roessner V, Rothenberger A. Pharmacological treatment of tics. In: Martino D, Leckmand JF, editors. Tourette syndrome. New York: Oxford University Press; 2013. p. 524–52.
Yael D, Israelashvili M, Bar-Gad I. Animal models of Tourette syndrome-from proliferation to standardization. Front Neurosci. 2016;10:132.
Bronfeld M, Yael D, Belelovsky K, Bar-Gad I. Motor tics evoked by striatal disinhibition in the rat. Front Syst Neurosci. 2013;7:50.
McCairn KW, Nagai Y, Hori Y, Ninomiya T, Kikuchi E, Lee JY, et al. A primary role for nucleus accumbens and related limbic network in vocal tics. Neuron. 2016;89(2):300–7.
Quezada J, Coffman KA. Current approaches and new developments in the pharmacological management of Tourette syndrome. CNS Drugs. 2018;32(1):33–45.
Shapiro E. Controlled study of haloperidol, pimozide and placebo for the treatment of Gilles de la Tourette’s syndrome. Arch Gen Psychiatry. 1989;46(8):722–30.
Sallee FR. Relative efficacy of haloperidol and pimozide in children and adolescents with Tourette’s disorder. Am J Psychiatry. 1997;154(8):1057–62.
Bruggeman R. Risperidone versus pimozide in Tourette’s disorder: a comparative double-blind parallel-group study. J Clin Psychiatry. 2001;62(1):50–6.
Gilbert DL. Tic reduction with risperidone versus pimozide in a randomized, double-blind, crossover trial. J Am Acad Child Adolesc Psychiatry. 2004;43(2):206–14.
Dion Y. Risperidone in the treatment of tourette syndrome: a double-blind, placebo-controlled trial. J Clin Psychopharmacol. 2002;22(1):31–9.
Scahill L. A placebo-controlled trial of risperidone in Tourette syndrome. Neurology. 2003;60(7):1130–5.
Kang H. Efficacy of clonidine transdermal patch for treatment of Tourette’s syndrome in children [in Chinese]. Zhongguo Dang Dai Er Ke Za Zhi. 2009;11(7):537–9.
Leckman JF. Clonidine treatment of Gilles de la Tourette’s syndrome. Arch Gen Psychiatry. 1991;48(4):324–8.
Singer HS. The treatment of attention-deficit hyperactivity disorder in Tourette’s syndrome: a double-blind placebo-controlled study with clonidine and desipramine. Pediatrics. 1995;95(1):74–81.
Du YS, Li HF, Vance A, Zhong YQ, Jiao FY, Wang HM, et al. Randomized double-blind multicentre placebo-controlled clinical trial of the clonidine adhesive patch for the treatment of tic disorders. Aust N Z J Psychiatry. 2008;42(9):807–13.
Tourette’s Syndrome Study Group. Treatment of ADHD in children with tics: a randomized controlled trial. Neurology. 2002;58(4):527–36.
Sallee F. Randomized, double-blind, placebo-controlled trial demonstrates the efficacy and safety of oral aripiprazole for the treatment of Tourette’s disorder in children and adolescents. J Child Adolesc Psychopharmacol. 2017;27(9):771–81.
Murphy TK. Extended-release guanfacine does not show a large effect on tic severity in children with chronic tic disorders. J Child Adolesc Psychopharmacol. 2017;27(9):762–70.
Sallee FR. Ziprasidone treatment of children and adolescents with Tourette’s syndrome: a pilot study. J Am Acad Child Adolesc Psychiatry. 2000;39(3):292–9.
Weisman H. Systematic review: pharmacological treatment of tic disorders–efficacy of antipsychotic and alpha-2 adrenergic agonist agents. Neurosci Biobehav Rev. 2013;37(6):1162–71.
Gaffney GR. Risperidone versus clonidine in the treatment of children and adolescents with Tourette’s syndrome. J Am Acad Child Adolesc Psychiatry. 2002;41(3):330–6.
Cummings DD, Singer HS, Krieger M, Miller TL, Mahone EM. Neuropsychiatric effects of guanfacine in children with mild tourette syndrome: a pilot study. Clin Neuropharmacol. 2002;25(6):325–32.
Scahill L, Chappell PB, Kim YS, Schultz RT, Katsovich L, Shepherd E, et al. A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. Am J Psychiatry. 2001;158(7):1067–74.
Bloch M, State M, Pittenger C. Recent advances in Tourette syndrome. Curr Opin Neurol. 2011;24(2):119–25.
Pringsheim T, Marras C. Pimozide for tics in Tourette’s syndrome. Cochrane Database Syst Rev. 2009;2:CD006996.
Pierce A, Rickards HE. Atypical antipsychotics for Tourette’s syndrome. Cochrane Database Syst Rev. 2009;4:CD008151.
Müller-Vahl KR, Krueger D. Does Tourette syndrome prevent tardive dyskinesia? Mov Disord. 2011;26(13):2442–3.
Muroni A, Paba S, Puligheddu M, Marrosu F, Bortolato M. A preliminary study of finasteride in Tourette syndrome. Mov Disord. 2011;26(11):2146–7.
Baldermann JC, Schüller T, Huys D, Becker I, Timmermann L, Jessen F, et al. Deep brain stimulation for Tourette-syndrome: a systematic review and meta-analysis. Brain Stimul. 2016;9(2):296–304.
McGuire JF, Ricketts EJ, Piacentini J, Murphy TK, Storch EA, Lewin AB. Behavior therapy for tic disorders: an evidenced-based review and new directions for treatment research. Curr Dev Disord Rep. 2015;2(4):309–17.
Piacentini J, Woods DW, Scahill L, Wilhelm S, Peterson AL, Chang S, et al. Behavior therapy for children with Tourette disorder: a randomized controlled trial. JAMA. 2010;303(19):1929–37.
Wilhelm S, Peterson AL, Piacentini J, Woods DW, Deckersbach T, Sukhodolsky DG, et al. Randomized trial of behavior therapy for adults with Tourette syndrome. Arch Gen Psychiatry. 2012;69(8):795–803.
Verdellen CW, Keijsers GP, Cath DC, Hoogduin CA. Exposure with response prevention versus habit reversal in Tourettes’s syndrome: a controlled study. Behav Res Ther. 2004;42(5):501–11.
Sandyk R. Marijuana and Tourette’s syndrome. J Clin Psychopharmacol. 1988;8(6):444–5.
Muller-Vahl KR, Kolbe H, Dengler R. Gilles de la Tourette syndrome. Effect of nicotine, alcohol and marihuana on clinical symptoms [in German]. Der Nervenarzt. 1997;68(12):985–9.
Lubman DI, Cheetham A, Yucel M. Cannabis and adolescent brain development. Pharmacol Ther. 2015;148:1–16.
Rahn EJ, Hohmann AG. Cannabinoids as pharmacotherapies for neuropathic pain: from the bench to the bedside. Neurotherapeutics. 2009;6(4):713–37.
Galiegue S, Mary S, Marchand J, Dussossoy D, Carriere D, Carayon P, et al. Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur J Biochem. 1995;232(1):54–61.
Glass M, Dragunow M, Faull RL. Cannabinoid receptors in the human brain: a detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77(2):299–318.
Gong JP, Onaivi ES, Ishiguro H, Liu QR, Tagliaferro PA, Brusco A, et al. Cannabinoid CB2 receptors: immunohistochemical localization in rat brain. Brain Res. 2006;1071(1):10–23.
Van Sickle MD, Duncan M, Kingsley PJ, Mouihate A, Urbani P, Mackie K, et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310(5746):329–32.
Onaivi ES. Neuropsychobiological evidence for the functional presence and expression of cannabinoid CB2 receptors in the brain. Neuropsychobiology. 2006;54(4):231–46.
Atwood BK, Mackie K. CB2: a cannabinoid receptor with an identity crisis. Br J Pharmacol. 2010;160(3):467–79.
Oz M. Receptor-independent actions of cannabinoids on cell membranes: focus on endocannabinoids. Pharmacol Ther. 2006;111(1):114–44.
Begg M, Pacher P, Batkai S, Osei-Hyiaman D, Offertaler L, Mo FM, et al. Evidence for novel cannabinoid receptors. Pharmacol Ther. 2005;106(2):133–45.
Muller C, Morales P, Reggio PH. Cannabinoid ligands targeting TRP channels. Front Mol Neurosci. 2019;11:487.
Lauckner JE, Jensen JB, Chen H-Y, Lu H-C, Hille B, Mackie K. GPR55 is a cannabinoid receptor that increases intracellular calcium and inhibits M current. Proc Natl Acad Sci USA. 2008;105(7):2699–704.
Mor M, Lodola A. Pharmacological tools in endocannabinoid neurobiology. Curr Top Behav Neurosci. 2009;1:87–110.
Fezza F, De Simone C, Amadio D, Maccarrone M. Fatty acid amide hydrolase: a gate-keeper of the endocannabinoid system. Subcell Biochem. 2008;49:101–32.
Bari M, Battista N, Fezza F, Gasperi V, Maccarrone M. New insights into endocannabinoid degradation and its therapeutic potential. Mini Rev Med Chem. 2006;6(3):257–68.
Beltramo M, Stella N, Calignano A, Lin SY, Makriyannis A, Piomelli D. Functional role of high-affinity anandamide transport, as revealed by selective inhibition. Science. 1997;277(5329):1094–7.
Tsuboi K, Sun Y-X, Okamoto Y, Araki N, Tonai T, Ueda N. Molecular characterization of N-acylethanolamine-hydrolyzing acid amidase, a novel member of the choloylglycine hydrolase family with structural and functional similarity to acid ceramidase. J Biol Chem. 2005;280(12):11082–92.
McKinney MK, Cravatt BF. Structure and function of fatty acid amide hydrolase. Annu Rev Biochem. 2005;74:411–32.
Dinh T, Carpenter D, Leslie F, Freund T, Katona I, Sensi S, et al. Brain monoglyceride lipase participating in endocannabinoid inactivation. Proc Natl Acad Sci USA. 2002;99(16):10819–24.
Obeso JA, Rodriguez-Oroz MC, Stamelou M, Bhatia KP, Burn DJ. The expanding universe of disorders of the basal ganglia. Lancet. 2014;384(9942):523–31.
Graybiel AM. Habits, rituals, and the evaluative brain. Ann Rev Neurosci. 2008;31:359–87.
Gillan CM, Morein-Zamir S, Urcelay GP, Sule A, Voon V, Apergis-Schoute AM, et al. Enhanced avoidance habits in obsessive-compulsive disorder. Biol Psychiatry. 2014;75(8):631–8.
Morera-Herreras T, Miguelez C, Aristieta A, Ruiz-Ortega JÁ, Ugedo L. Endocannabinoid modulation of dopaminergic motor circuits. Front Pharmacol. 2012;3:110.
Mink JW. The basal ganglia: focused selection and inhibition of competing motor programs. Prog Neurobiol. 1996;50(4):381–425.
Mink JW. Basal ganglia dysfunction in Tourette’s syndrome: a new hypothesis. Pediatr Neurol. 2001;25(3):190–8.
Greene DJ, Black KJ, Schlaggar BL. Neurobiology and functional anatomy of tic disorders. Oxford: Oxford University Press; 2013.
Singer HS, Reiss AL, Brown JE, Aylward EH, Shih B, Chee E, et al. Volumetric MRI changes in basal ganglia of children with Tourette’s syndrome. Neurology. 1993;43(5):950–6.
Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, De Costa BR, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA. 1990;87(5):1932–6.
Glass M, Faull R, Dragunow M. Cannabinoid receptors in the human brain: a detailed anatomical and quantitative autoradiographic study in the fetal, neonatal and adult human brain. Neuroscience. 1997;77(2):299–318.
Tinaz S, Belluscio BA, Malone P, van der Veen JW, Hallett M, Horovitz SG. Role of the sensorimotor cortex in Tourette syndrome using multimodal imaging. Hum Brain Mapp. 2014;35(12):5834–46.
Soros P. Tourette syndrome, ADHD, and the limbic system: investigating the pathophysiology. Dev Med Child Neurol. 2008;50(7):486.
Nolte J. Essentials of the human brain e-book: With student consult online access. Oxford: Elsevier Health Sciences; 2009.
Albin RL, Mink JW. Recent advances in Tourette syndrome research. Trends Neurosci. 2006;29(3):175–82.
Bohlhalter S, Goldfine A, Matteson S, Garraux G, Hanakawa T, Kansaku K, et al. Neural correlates of tic generation in Tourette syndrome: an event-related functional MRI study. Brain. 2006;129(Pt 8):2029–37.
Hong KE, Ock SM, Kang MH, Kim CE, Bae JN, Lim MK, et al. The segmented regional volumes of the cerebrum and cerebellum in boys with Tourette syndrome. J Korean Med Sci. 2002;17(4):530–6.
Lerner A, Bagic A, Boudreau EA, Hanakawa T, Pagan F, Mari Z, et al. Neuroimaging of neuronal circuits involved in tic generation in patients with Tourette syndrome. Neurology. 2007;68(23):1979–87.
Pourfar M, Feigin A, Tang CC, Carbon-Correll M, Bussa M, Budman C, et al. Abnormal metabolic brain networks in Tourette syndrome. Neurology. 2011;76(11):944–52.
Tobe RH, Bansal R, Xu D, Hao X, Liu J, Sanchez J, et al. Cerebellar morphology in Tourette syndrome and obsessive-compulsive disorder. Ann Neurol. 2010;67(4):479–87.
Singer HS, Szymanski S, Giuliano J, Yokoi F, Dogan AS, Brasic JR, et al. Elevated intrasynaptic dopamine release in Tourette’s syndrome measured by PET. Am J Psychiatry. 2002;159(8):1329–36.
Wong DF, Brasic JR, Singer HS, Schretlen DJ, Kuwabara H, Zhou Y, et al. Mechanisms of dopaminergic and serotonergic neurotransmission in Tourette syndrome: clues from an in vivo neurochemistry study with PET. Neuropsychopharmacology. 2008;33(6):1239–51.
Yoon DY, Gause CD, Leckman JF, Singer HS. Frontal dopaminergic abnormality in Tourette syndrome: a postmortem analysis. J Neurol Sci. 2007;255(1–2):50–6.
Giuffrida A, Parsons LH, Kerr TM, Rodriguez de Fonseca F, Navarro M, Piomelli D. Dopamine activation of endogenous cannabinoid signaling in dorsal striatum. Nature Neurosci. 1999;2(4):358–63.
Muller-Vahl KR. Treatment of Tourette syndrome with cannabinoids. Behav Neurol. 2013;27(1):119–24.
Tzavara ET, Li DL, Moutsimilli L, Bisogno T, Di Marzo V, Phebus LA, et al. Endocannabinoids activate transient receptor potential vanilloid 1 receptors to reduce hyperdopaminergia-related hyperactivity: therapeutic implications. Biol Psychiatry. 2006;59(6):508–15.
Hohmann AG, Herkenham M. Localization of cannabinoid CB1 receptor mRNA in neuronal subpopulations of rat striatum: a double-label in situ hybridization study. Synapse. 2000;37(1):71–80.
Herkenham M, Groen BG, Lynn AB, De Costa BR, Richfield EK. Neuronal localization of cannabinoid receptors and second messengers in mutant mouse cerebellum. Brain Res. 1991;552(2):301–10.
Kofalvi A, Rodrigues RJ, Ledent C, Mackie K, Vizi ES, Cunha RA, et al. Involvement of cannabinoid receptors in the regulation of neurotransmitter release in the rodent striatum: a combined immunochemical and pharmacological analysis. J Neurosci. 2005;25(11):2874–84.
Fernández-Ruiz J. The endocannabinoid system as a target for the treatment of motor dysfunction. Br J Pharmacol. 2009;156(7):1029–40.
Friedman E, Jin LQ, Cai GP, Hollon TR, Drago J, Sibley DR, et al. D1-like dopaminergic activation of phosphoinositide hydrolysis is independent of D1A dopamine receptors: evidence from D1A knockout mice. Mol Pharmacol. 1997;51(1):6–11.
Rosengarten H, Friedhoff AJ. A phosphoinositide-linked dopamine D1 receptor mediates repetitive jaw movements in rats. Biol Psychiatry. 1998;44(11):1178–84.
Jin LQ, Cai G, Wang HY, Smith C, Friedman E. Characterization of the phosphoinositide-linked dopamine receptor in a mouse hippocampal-neuroblastoma hybrid cell line. J Neurochem. 1998;71(5):1935–43.
Undieh AS. Pharmacology of signaling induced by dopamine D(1)-like receptor activation. Pharmacol Ther. 2010;128(1):37–60.
Alger BE. Endocannabinoid identification in the brain: studies of breakdown lead to breakthrough, and there may be NO hope. Sci STKE. 2005;2005(309):pe51.
Sugiura T, Kishimoto S, Oka S, Gokoh M. Biochemistry, pharmacology and physiology of 2-arachidonoylglycerol, an endogenous cannabinoid receptor ligand. Prog Lipid Res. 2006;45(5):405–46.
Kirchheimer C, Mendez CF, Acquier A, Nowicki S. Role of 20-HETE in D1/D2 dopamine receptor synergism resulting in the inhibition of Na+-K+-ATPase activity in the proximal tubule. Am J Physiol Renal Physiol. 2007;292(5):F1435–42.
Di Marzo V, Hill MP, Bisogno T, Crossman AR, Brotchie JM. Enhanced levels of endogenous cannabinoids in the globus pallidus are associated with a reduction in movement in an animal model of Parkinson’s disease. FASEB J. 2000;14(10):1432–8.
Maneuf YP, Crossman AR, Brotchie JM. The cannabinoid receptor agonist WIN 55,212-2 reduces D2, but not D1, dopamine receptor-mediated alleviation of akinesia in the reserpine-treated rat model of Parkinson’s disease. Exp Neurol. 1997;148(1):265–70.
Segovia G, Mora F, Crossman AR, Brotchie JM. Effects of CB1 cannabinoid receptor modulating compounds on the hyperkinesia induced by high-dose levodopa in the reserpine-treated rat model of Parkinson’s disease. Mov Disord. 2003;18(2):138–49.
Sieradzan KA, Fox SH, Hill M, Dick JPR, Crossman AR, Brotchie JM. Cannabinoids reduce levodopa-induced dyskinesia in Parkinson’s disease: a pilot study. Neurology. 2001;57(11):2108–11.
Carroll CB, Bain PG, Teare L, Liu X, Joint C, Wroath C, et al. Cannabis for dyskinesia in Parkinson disease. A randomized double-blind crossover study. Neurology. 2004;63(7):1245–50.
Renard J, Norris C, Rushlow W, Laviolette SR. Neuronal and molecular effects of cannabidiol on the mesolimbic dopamine system: implications for novel schizophrenia treatments. Neurosci Biobehav Rev. 2017;75:157–65.
Singer HS, Minzer K. Neurobiology of Tourette’s syndrome: concepts of neuroanatomic localization and neurochemical abnormalities. Brain Dev. 2003;25:S70–84.
Singer HS. The neurochemistry of Tourette syndrome. In: Martino D, Leckmand JF, editors. Tourette syndrome. New York: Oxford University Press; 2013. p. 276–300.
Anderson GM, Pollak ES, Chatterjee D, Leckman JF, Riddle MA, Cohen DJ. Brain monoamines and amino acids in Gilles de la Tourette’s syndrome: a preliminary study of subcortical regions. Arch Gen Psychiatry. 1992;49(7):584–6.
Iversen L. Cannabis and the brain. Brain. 2003;126(Pt 6):1252–70.
Sanchez-Blazquez P, Rodriguez-Munoz M, Garzon J. The cannabinoid receptor 1 associates with NMDA receptors to produce glutamatergic hypofunction: implications in psychosis and schizophrenia. Front Pharmacol. 2014;2(4):169.
Rodríguez-Muñoz M, Sánchez-Blázquez P, Merlos M, Garzón-Niño J. Endocannabinoid control of glutamate NMDA receptors: the therapeutic potential and consequences of dysfunction. Oncotarget. 2016;7(34):55840–62.
Henstridge CM, Balenga NA, Ford LA, Ross RA, Waldhoer M, Irving AJ. The GPR55 ligand L-alpha-lysophosphatidylinositol promotes RhoA-dependent Ca2+ signaling and NFAT activation. FASEB J. 2009;23(1):183–93.
Sylantyev S, Jensen TP, Ross RA, Rusakov DA. Cannabinoid- and lysophosphatidylinositol-sensitive receptor GPR55 boosts neurotransmitter release at central synapses. Proc Natl Acad Sci USA. 2013;110(13):5193–8.
Gadzicki D, Müller-Vahl KR, Heller D, Ossege S, Nöthen MM, Hebebrand J, et al. Tourette syndrome is not caused by mutations in the central cannabinoid receptor (CNR1) gene. Am J Med Genet B Neuropsychiatr Genet. 2004;127(1):97–103.
Hemming M, Yellowlees PM. Effective treatment of Tourette’s syndrome with marijuana. J Psychopharmacol. 1993;7(4):389–91.
Abi-Jaoude E, Chen L, Cheung P, Bhikram T, Sandor P. Preliminary evidence on cannabis effectiveness and tolerability for adults with Tourette syndrome. J Neuropsychiatry Clin Neurosci. 2017;29(4):391–400.
Thaler A, Arad S, Schleider LB-L, Knaani J, Taichman T, Giladi N, et al. Single center experience with medical cannabis in Gilles de la Tourette syndrome. Parkinsonism Relat Disord. 2018. https://doi.org/10.1016/j.parkreldis.2018.10.004.
Brunnauer A, Segmiller FM, Volkamer T, Laux G, Müller N, Dehning S. Cannabinoids improve driving ability in a Tourette’s patient. Psychiatry Res. 2011;190(2):382.
Hasan A, Rothenberger A, Münchau A, Wobrock T, Falkai P, Roessner V. Oral Δ9-tetrahydrocannabinol improved refractory Gilles de la Tourette syndrome in an adolescent by increasing intracortical inhibition: a case report. J Clin Psychopharmacol. 2010;30(2):190–2.
Szejko N, Jakubovski E, Fremer C, Kunert K, Müller-Vahl K. Delta-9-tetrahydrocannabinol for the treatment of a child with Tourette syndrome: case report. Eur J Med Case Rep. 2018;2(2):39–41.
Jakubovski E, Muller-Vahl K. Speechlessness in Gilles de la Tourette syndrome: cannabis-based medicines improve severe vocal blocking tics in two patients. Int J Mol Sci. 2017;18(8):E1739.
Pichler EM, Kawohl W, Seifritz E, Roser P. Pure delta-9-tetrahydrocannabinol and its combination with cannabidiol in treatment-resistant Tourette syndrome: a case report. Int J Psychiatry Med. 2019;54(2):150–6.
Müller-Vahl KR, Schneider U, Koblenz A, Jöbges M, Kolbe H, Daldrup T, et al. Treatment of Tourette’s syndrome with Δ9-tetrahydrocannabinol (THC): a randomized crossover trial. Pharmacopsychiatry. 2002;35(02):57–61.
Müller-Vahl KR, Schneider U, Prevedel H, Theloe K, Kolbe H, Daldrup T, et al. Δ9-tetrahydrocannabinol (THC) is effective in the treatment of tics in Tourette syndrome: a 6-week randomized trial. J Clin Psychiatry. 2003;64(4):459–65.
Trainor D. Severe motor and vocal tics controlled with Sativex®. Australas Psychiatry. 2016;24(6):541–4.
Kanaan AS. Significant tic reduction in an otherwise treatment-resistant patient with Gilles de la Tourette syndrome following treatment with nabiximols. Brain Sci. 2017;7(5):E47.
Abide Therapeutics. Abide Therapeutics reports positive topline data from phase 1b study of ABX- 1431 in Tourette syndrome. 2017. http://abidetx.com/news/abide-therapeutics-reports-positive-topline-datafrom-phase-1b-study-of-abx-1431-in-tourette-syndrome. Accessed 1 Apr 2019.
FDA. FDA finds drugs under investigation in the U.S. related to French BIA 10-2474 drug do not pose similar safety risks. Updated 8/12/16. https://www.fda.gov/Drugs/DrugSafety/ucm482740.htm. Accessed 1 Nov 2018.
Thiele EA, Marsh ED, French JA, Mazurkiewicz-Beldzinska M, Benbadis SR, Joshi C, et al. Cannabidiol in patients with seizures associated with Lennox-Gastaut syndrome (GWPCARE4): a randomised, double-blind, placebo-controlled phase 3 trial. Lancet. 2018;391(10125):1085–96.
Meier MH, Caspi A, Ambler A, Harrington H, Houts R, Keefe RS, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci USA. 2012;109(40):E2657–64.
Pope HG Jr, Gruber AJ, Hudson JI, Cohane G, Huestis MA, Yurgelun-Todd D. Early-onset cannabis use and cognitive deficits: what is the nature of the association? Drug Alcohol Depend. 2003;69(3):303–10.
Ehrenreich H, Rinn T, Kunert HJ, Moeller MR, Poser W, Schilling L, et al. Specific attentional dysfunction in adults following early start of cannabis use. Psychopharmacology. 1999;142(3):295–301.
Fontes MA, Bolla KI, Cunha PJ, Almeida PP, Jungerman F, Laranjeira RR, et al. Cannabis use before age 15 and subsequent executive functioning. Br J Psychiatry. 2011;198(6):442–7.
Solowij N, Jones KA, Rozman ME, Davis SM, Ciarrochi J, Heaven PC, et al. Verbal learning and memory in adolescent cannabis users, alcohol users and non-users. Psychopharmacology. 2011;216(1):131–44.
Lisdahl KM, Gilbart ER, Wright NE, Shollenbarger S. Dare to delay? The impacts of adolescent alcohol and marijuana use onset on cognition, brain structure, and function. Front Psychiatry. 2013;4:53.
Hadland SE, Knight JR, Harris SK. Medical marijuana: review of the science and implications for developmental-behavioral pediatric practice. J Dev Behav Pediatr. 2015;36(2):115–23.
Moore TH, Zammit S, Lingford-Hughes A, Barnes TR, Jones PB, Burke M, et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–28.
Galve-Roperh I, Palazuelos J, Aguado T, Guzmán M. The endocannabinoid system and the regulation of neural development: potential implications in psychiatric disorders. Eur Arch Psychiatry Clin Neurosci. 2009;259(7):371–82.
Brunnauer A, Segmiller FM, Volkamer T, Laux G, Müller N, Dehning S. Cannabinoids improve driving ability in a Tourette’s patient. Psychiatry Res. 2011;190(2–3):382.
Leckman J, Towbin K, Ort S, Cohen D. Clinical assessment of tic disorder severity. Tourette’s syndrome and tic disorders. New York: Wiley; 1988. p. 55–78.
Yoo HK, Joung YS, Lee JS, Song DH, Lee YS, Kim JW, et al. A multicenter, randomized, double-blind, placebo-controlled study of aripiprazole in children and adolescents with Tourette’s disorder. J Clin Psychiatry. 2013;74(8):e772–80.
Sallee F, Kohegyi E, Zhao J, McQuade R, Cox K, Sanchez R, et al. Randomized, double-blind, placebo-controlled trial demonstrates the efficacy and safety of oral aripiprazole for the treatment of Tourette’s disorder in children and adolescents. J Child Adolesc Psychopharmacol. 2017;27(9):771–81.
Hannover Medical School. CANNAbinoids in the Treatment of TICS (CANNA-TICS) [ClinicalTrials.gov identifier NCT03087201]. National Institutes of Health, ClinicalTrials.gov. https://ClinicalTrials.gov. Accessed 1 Apr 2019.
Artukoglu BB, Beyer C, Zuloff-Shani A, Brener E, Bloch MH. Efficacy of palmitoylethanolamide for pain: a meta-analysis. Pain Physician. 2017;20(5):353–62.
LoVerme J, La Rana G, Russo R, Calignano A, Piomelli D. The search for the palmitoylethanolamide receptor. Life Sci. 2005;77(14):1685–98.
Russo EB. Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. Br J Pharmacol. 2011;163(7):1344–64.
del Carmen García M, Adler-Graschinsky E, Celuch SM. Enhancement of the hypotensive effects of intrathecally injected endocannabinoids by the entourage compound palmitoylethanolamide. Eur J Pharmacol. 2009;610(1–3):75–80.
Esposito E, Impellizzeri D, Mazzon E, Paterniti I, Cuzzocrea S. Neuroprotective activities of palmitoylethanolamide in an animal model of Parkinson’s disease. PLoS One. 2012;7(8):e41880.
Scuderi C, Valenza M, Stecca C, Esposito G, Carratu MR, Steardo L. Palmitoylethanolamide exerts neuroprotective effects in mixed neuroglial cultures and organotypic hippocampal slices via peroxisome proliferator-activated receptor-alpha. J Neuroinflamm. 2012;9(9):49.
Ahmad A, Crupi R, Impellizzeri D, Campolo M, Marino A, Esposito E, et al. Administration of palmitoylethanolamide (PEA) protects the neurovascular unit and reduces secondary injury after traumatic brain injury in mice. Brain Behav Immun. 2012;26(8):1310–21.
Kramar C, Loureiro M, Renard J, Laviolette SR. Palmitoylethanolamide modulates GPR55 receptor signaling in the ventral hippocampus to regulate mesolimbic dopamine activity, social interaction, and memory processing. Cannabis Cannabinoid Res. 2017;2(1):8–20.
Therapix Biosciences Ltd. Therapix Biosciences announces topline results of phase IIa study at Yale University for Tourette Syndrome Program. 2018. https://www.prnewswire.com/news-releases/therapix-biosciences-announces-topline-results-of-phase-iia-study-at-yale-university-for-tourette-syndrome-program-300626244.html. Accessed 11 Oct 2018.
Therapix Biosciences Ltd. A study to examine the efficacy of a Therapeutic THX-110 for Tourette syndrome. [ClinicalTrials.gov identifier NCT03651726]. National Institutes of Health, ClinicalTrials.gov. https://ClinicalTrials.gov.
Pan B, Wang W, Long JZ, Sun D, Hillard CJ, Cravatt BF, et al. Blockade of 2-arachidonoylglycerol hydrolysis by selective monoacylglycerol lipase inhibitor 4-nitrophenyl 4-(dibenzo[d][1,3]dioxol-5-yl(hydroxy)methyl)piperidine-1-carboxylate (JZL184) enhances retrograde endocannabinoid signaling. J Pharmacol Exp Ther. 2009;331(2):591–7.
Wang Y, Gu N, Duan T, Kesner P, Blaskovits F, Liu J, et al. Monoacylglycerol lipase inhibitors produce pro- or antidepressant responses via hippocampal CA1 GABAergic synapses. Mol Psychiatry. 2017;22(2):215–26.
Schlosburg JE, Blankman JL, Long JZ, Nomura DK, Pan B, Kinsey SG, et al. Chronic monoacylglycerol lipase blockade causes functional antagonism of the endocannabinoid system. Nat Neurosci. 2010;13(9):1113–9.
Long JZ, Nomura DK, Vann RE, Walentiny DM, Booker L, Jin X, et al. Dual blockade of FAAH and MAGL identifies behavioral processes regulated by endocannabinoid crosstalk in vivo. Proc Natl Acad Sci USA. 2009;106(48):20270–5.
Cravatt BF, Giang DK, Mayfield SP, Boger DL, Lerner RA, Gilula NB. Molecular characterization of an enzyme that degrades neuromodulatory fatty-acid amides. Nature. 1996;384(6604):83.
Giang DK, Cravatt BF. Molecular characterization of human and mouse fatty acid amide hydrolases. Proc Natl Acad Sci USA. 1997;94(6):2238–42.
Di Marzo V. The endocannabinoid system: its general strategy of action, tools for its pharmacological manipulation and potential therapeutic exploitation. Pharmacol Res. 2009;60(2):77–84.
Huggins JP, Smart TS, Langman S, Taylor L, Young T. An efficient randomised, placebo-controlled clinical trial with the irreversible fatty acid amide hydrolase-1 inhibitor PF-04457845, which modulates endocannabinoids but fails to induce effective analgesia in patients with pain due to osteoarthritis of the knee. Pain. 2012;153(9):1837–46.
Fegley D, Gaetani S, Duranti A, Tontini A, Mor M, Tarzia G, et al. Characterization of the fatty acid amide hydrolase inhibitor cyclohexyl carbamic acid 3′-carbamoyl-biphenyl-3-yl ester (URB597): effects on anandamide and oleoylethanolamide deactivation. J Pharmacol Exp Ther. 2005;313(1):352–8.
Cravatt BF, Demarest K, Patricelli MP, Bracey MH, Giang DK, Martin BR, et al. Supersensitivity to anandamide and enhanced endogenous cannabinoid signaling in mice lacking fatty acid amide hydrolase. Proc Natl Acad Sci USA. 2001;98(16):9371–6.
Salaga M, Sobczak M, Fichna J. Inhibition of fatty acid amide hydrolase (FAAH) as a novel therapeutic strategy in the treatment of pain and inflammatory diseases in the gastrointestinal tract. Eur J Pharm Sci. 2014;14(52):173–9.
Justinova Z, Mangieri RA, Bortolato M, Chefer SI, Mukhin AG, Clapper JR, et al. Fatty acid amide hydrolase inhibition heightens anandamide signaling without producing reinforcing effects in primates. Biol Psychiatry. 2008;64(11):930–7.
van Esbroeck ACM, Janssen APA, Cognetta AB 3rd, Ogasawara D, Shpak G, van der Kroeg M, et al. Activity-based protein profiling reveals off-target proteins of the FAAH inhibitor BIA 10-2474. Science. 2017;356(6342):1084–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bloch is on the Scientific Advisory Board of Therapix Biosciences and receives research support from Biohaven Pharmaceuticals, Neurocrine Biosciences, Janssen Pharmaceuticals, and Therapix Biosciences. Dr. Bloch also receives research support from the Lesbian Health Fund, the National Institutes of Health, Tourette Association of America, the Brain & Behavior Research Foundation (formerly NARSAD), and the Patterson Foundation. Dr. Artukoglu has no conflicts of interest to disclose.
Funding
No sources of funding were used to assist with the preparation of this article.
Rights and permissions
About this article
Cite this article
Artukoglu, B.B., Bloch, M.H. The Potential of Cannabinoid-Based Treatments in Tourette Syndrome. CNS Drugs 33, 417–430 (2019). https://doi.org/10.1007/s40263-019-00627-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40263-019-00627-1